Cvs Caremark Dupixent Prior Authorization Form
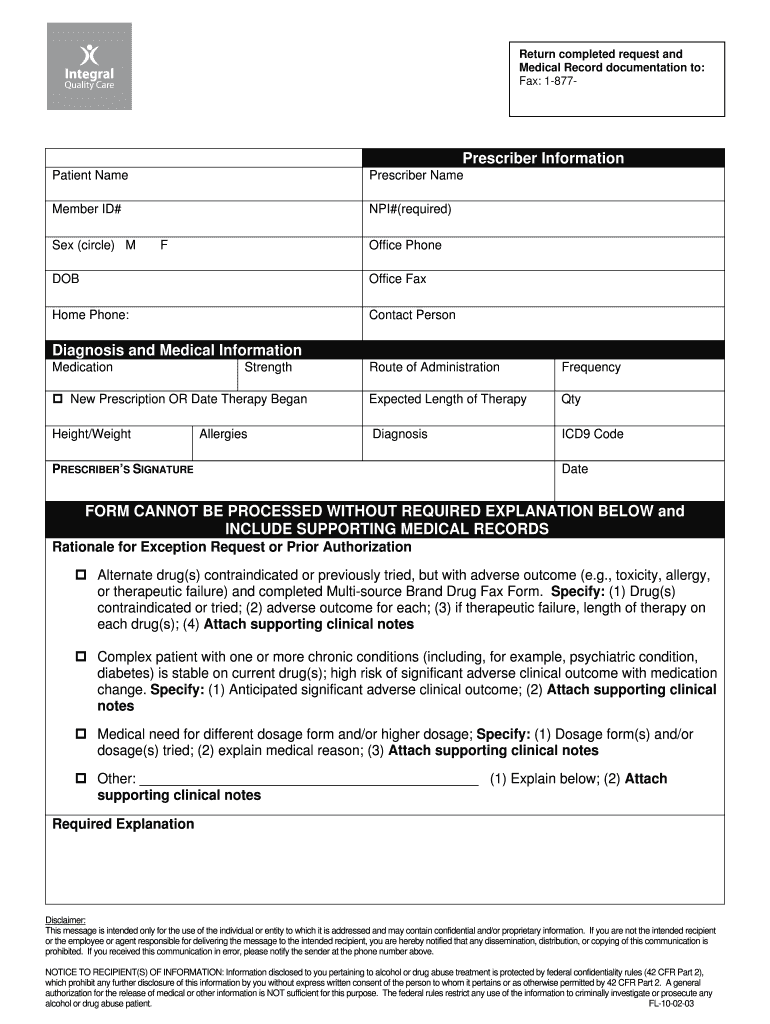
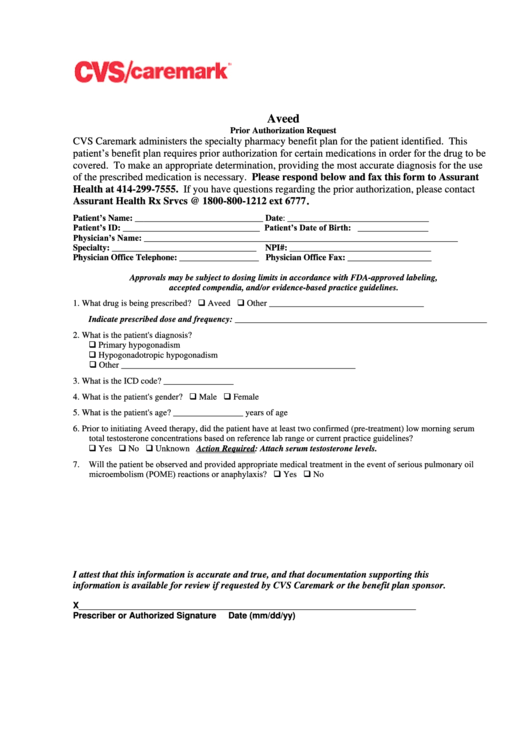
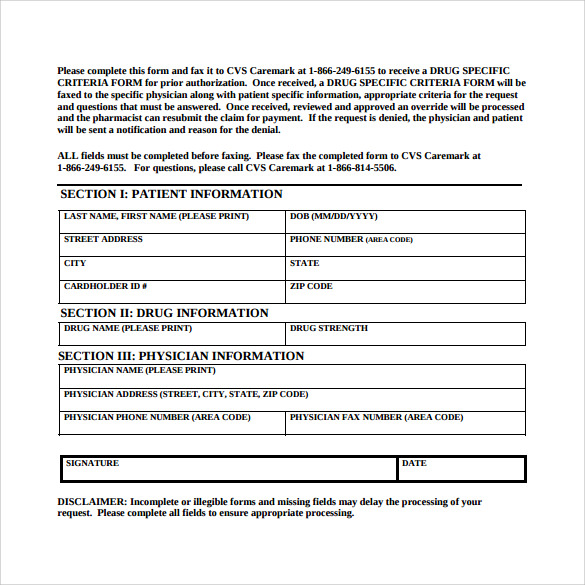
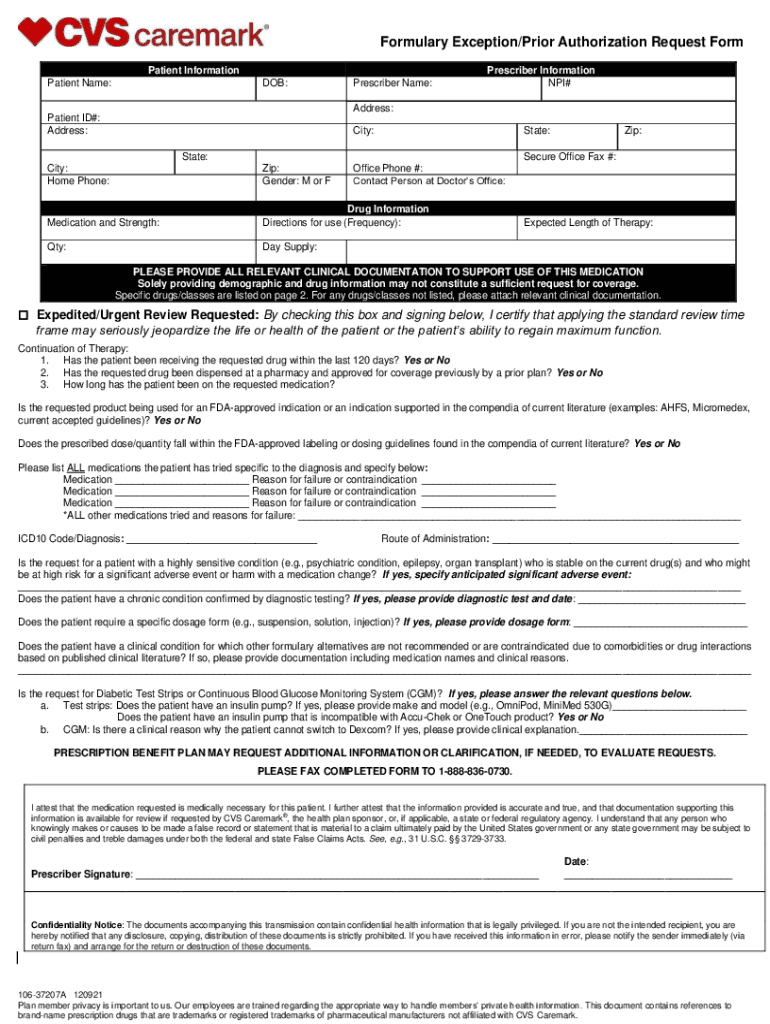
Cvs Caremark Dupixent Prior Authorization Form - Web a patient’s health plan is likely to require a prior authorization (pa) before it approves dupixent for appropriate patients. Web we offer access to specialty medications and infusion therapies, centralized intake and benefits verification, and prior authorization assistance. Signnow allows users to edit, sign, fill and share all type of documents online. Complete the cvs caremark prior authorization form: Prior approval criteria, forms, and rationale. Ad get the lowest price on your prescriptions. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Select your specialty therapy, then download and complete the appropriate enrollment form when you send. To access other state specific forms, please click here. Complete/review information, sign and date. Web to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Attach an itemized receipt to the claim form, and. To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. How to obtain prior approval. However you choose to submit a pa. Web up to $40 cash back 02. To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web clinical prior authorization criteria. Service benefit plan prior approval p.o. Ad get the lowest price on your prescriptions. Web let cvs caremark help you understand your plan requirements as well as which of your medications are covered and which may need prior authorization. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web to make an appropriate determination, providing the most accurate diagnosis for the use of the. Complete the cvs caremark prior authorization form: Ad register and subscribe now to work on your cvs caremark formulary prior auth req form. If you have questions regarding the prior. Web cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior authorization (pa) requests to payors for the prescribed medication for this patient and to attach this enrollment. Web up to $40 cash back 02. Complete the cvs caremark prior authorization form: Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. If you have questions regarding the prior. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Ad register and subscribe now to work on your cvs caremark formulary prior auth req form. Web to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Signnow allows users to edit,. Don’t miss out on future savings. Select your specialty therapy, then download and complete the appropriate enrollment form when you send. Service benefit plan prior approval p.o. Web cvs specialty pharmacy and/or its affiliate pharmacies to complete and submit prior authorization (pa) requests to payors for the prescribed medication for this patient and to attach this enrollment form to the. To make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web up to $40 cash back 02. Web let cvs caremark help you understand your plan requirements as well as which of your medications are covered and which may need prior authorization. Covermymeds automates the prior authorization. Don’t miss out on. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). If you have questions regarding the prior. Covermymeds automates the prior authorization. Web we offer access to specialty medications and infusion therapies, centralized intake. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web cvs/caremark fax form proton pump inhibitors post limit this fax machine is located in a secure location as required by hipaa regulations. Covermymeds is cvs caremark prior authorization forms’s preferred method for receiving epa requests. To access other state specific. Web let cvs caremark help you understand your plan requirements as well as which of your medications are covered and which may need prior authorization. If you have questions regarding the prior. Complete/review information, sign and date. This checklist can help guide you through the. Attach an itemized receipt to the claim form, and. How to obtain prior approval. Covermymeds automates the prior authorization. Web to make an appropriate determination, providing the most accurate diagnosis for the use of the prescribed medication is necessary. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Ad get the lowest price on your prescriptions. Don’t miss out on future savings. Select your specialty therapy, then download and complete the appropriate enrollment form when you send. You, your provider, or pharmacist, may check with cvs caremark customer care to verify covered. Web if a form for the specific medication cannot be found, please use the global prior authorization form. California members please use the california global pa form. Get a coupon, save at the counter now! Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web up to $40 cash back 02. Obtain the prior authorization form from cvs caremark's website or your healthcare provider. Ad register and subscribe now to work on your cvs caremark formulary prior auth req form.Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
Cvs Caremark Appeal Form Printable Fill Out and Sign Printable PDF
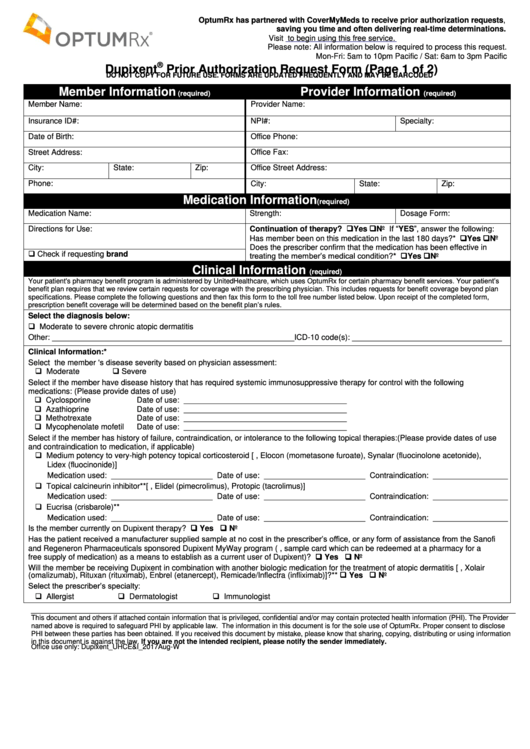
Fillable Online Dupixent Prior Authorization Request Form (Page 1 of 2
Cvs Aveed Prior Authorization Request Form printable pdf download
Sample Caremark Prior Authorization Form 8+ Free Documents in PDF
Caremark Authorization Form Fill Out and Sign Printable PDF Template
Dupixent Prior Authorization Request Form printable pdf download
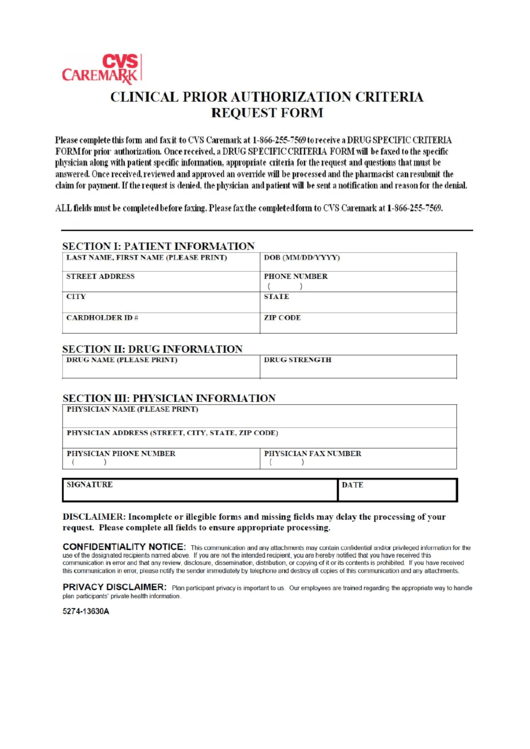
Caremark Prior Authorization Criteria Request Form printable pdf download
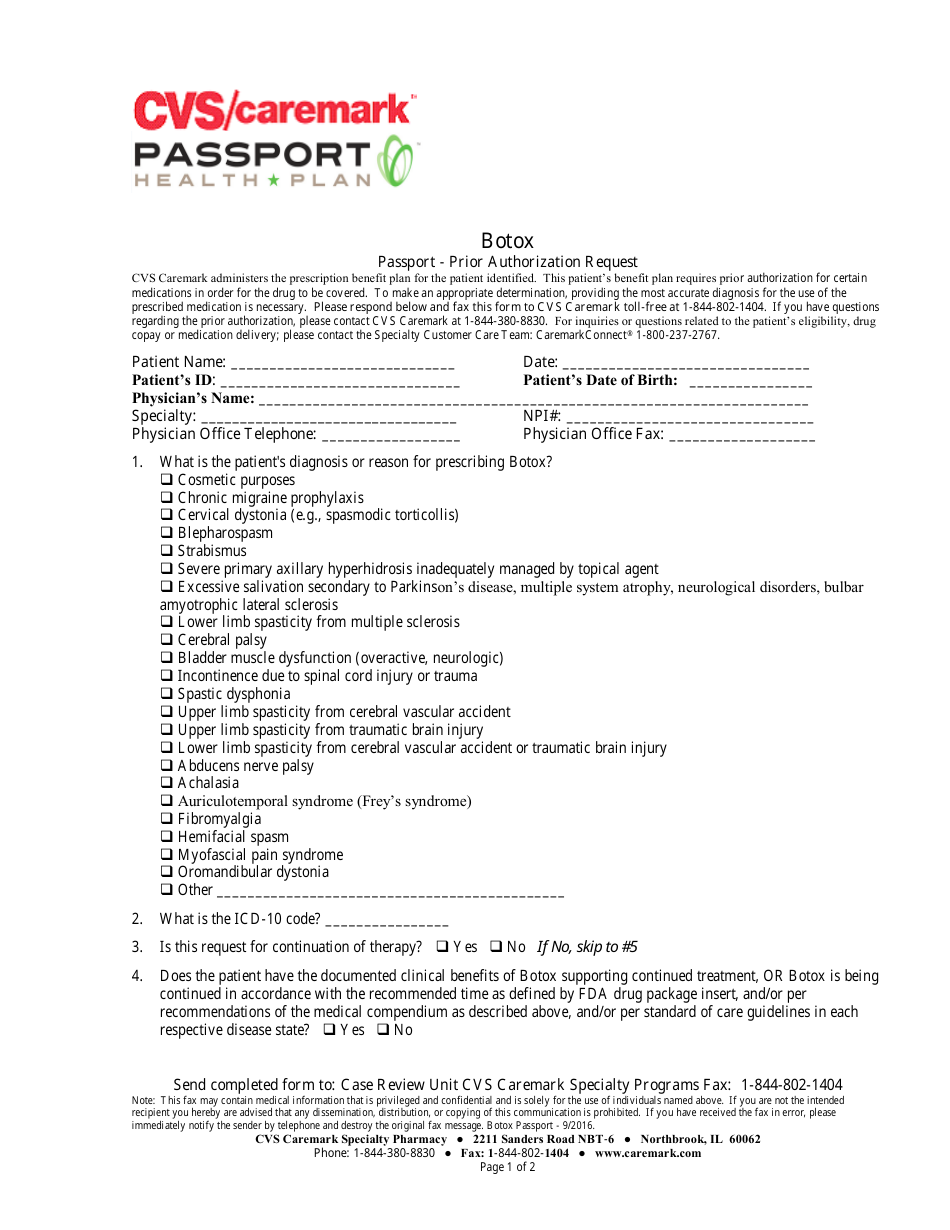
Botox Passport Prior Authorization Request Form Cvs Caremark Fill
Cvs Caremark Wegovy Prior Authorization Form
Related Post: