Fepblue Prior Authorization Form
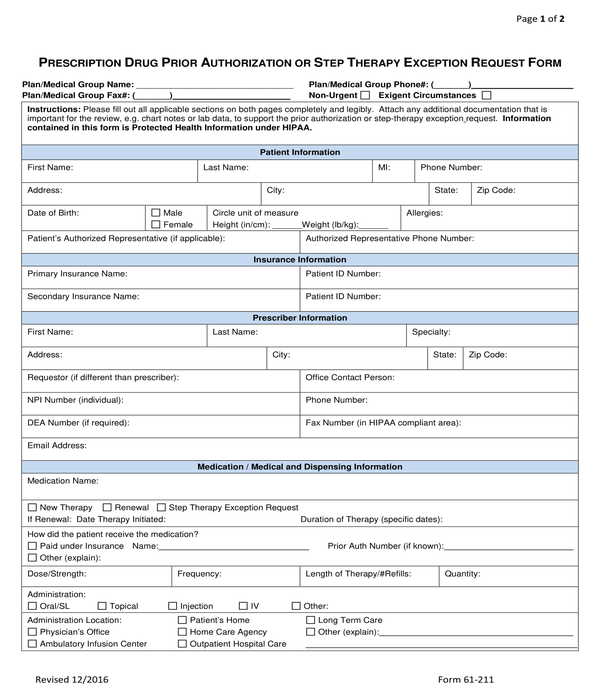
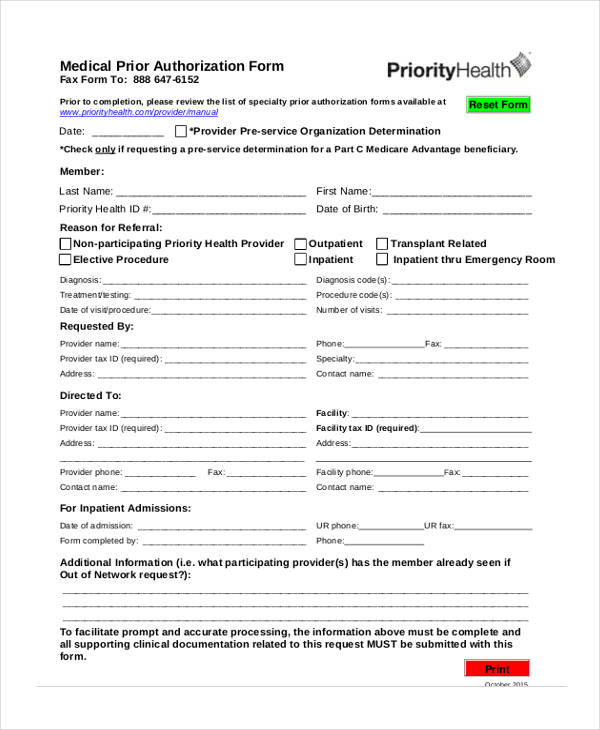
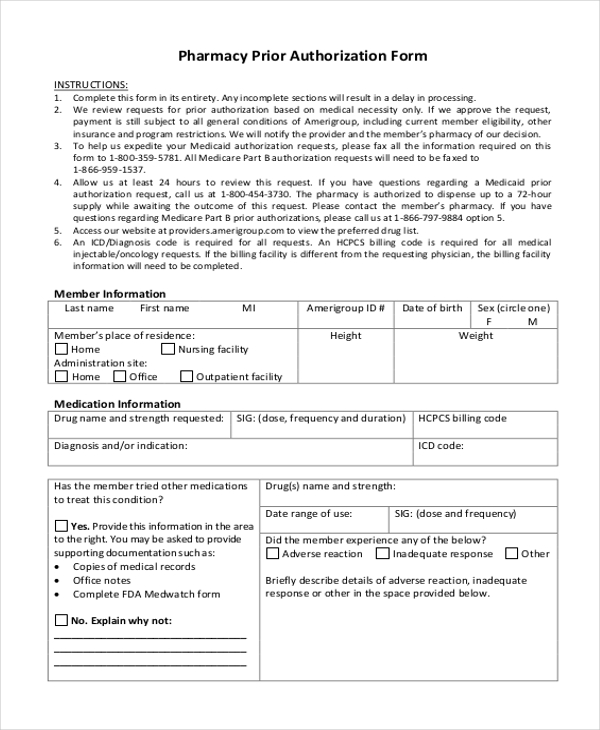
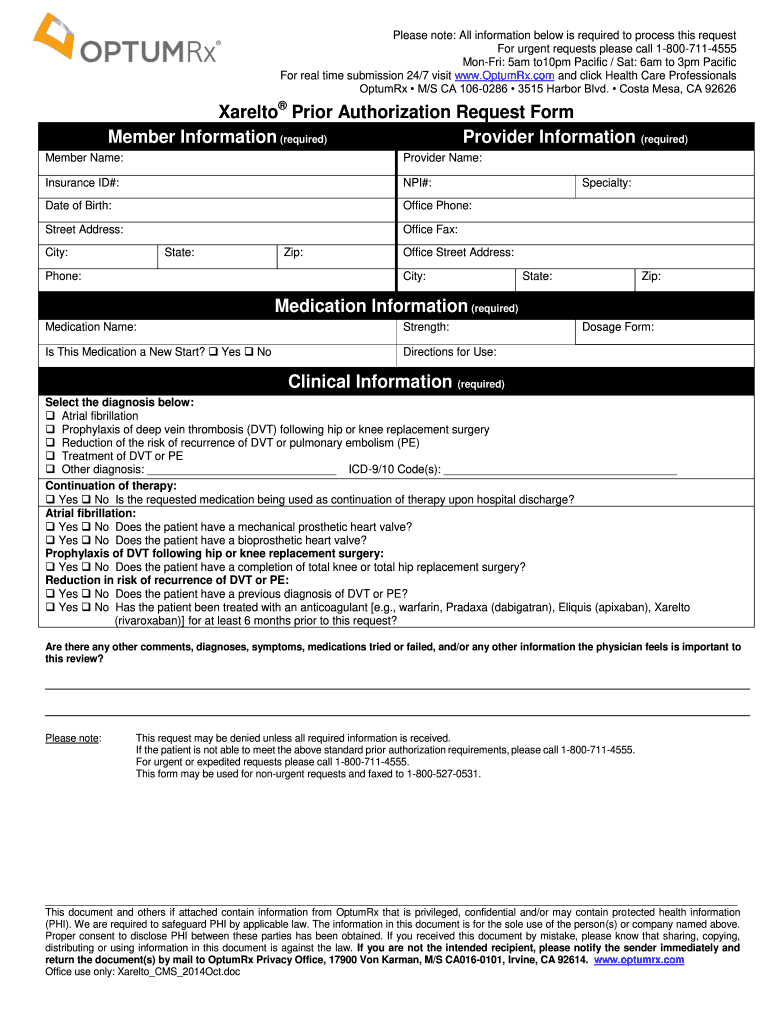
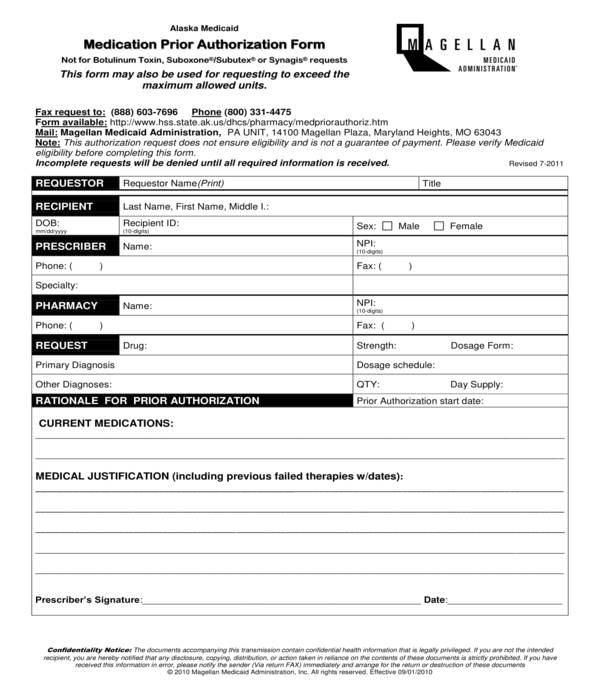
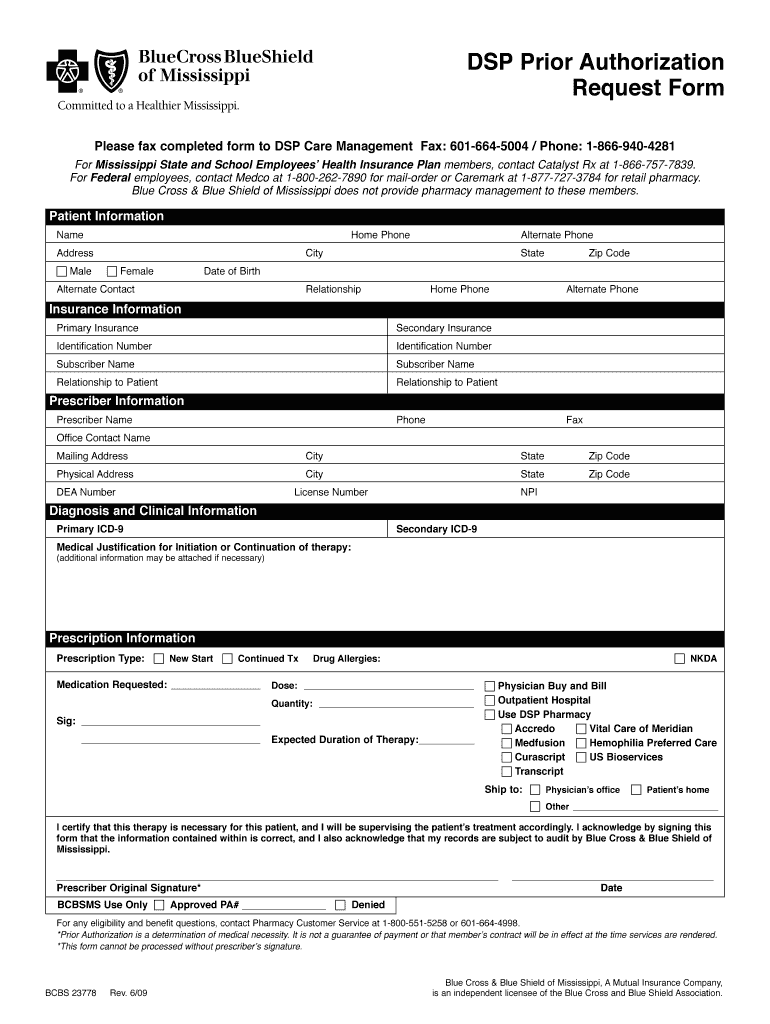
Fepblue Prior Authorization Form - Web 2023 fep prior approval drug list rev. Web a prior approval is required for the procedures listed below for both the fep standard and basic option plan and the fep blue focus plan. Prior approval may be required for certain prescription drugs before they can be covered under the pharmacy. Providers must obtain prior approval for the services below for fep standard and basic. If you have questions regarding the list,. Web home health/home infusion therapy/hospice: Edit, sign and save blue prescriptn drug auth form. Web prior approval must be renewed periodically. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Ad register and subscribe now to work on your blue advantage med part d prescriptn drug auth. Web spine services program participation to begin august 14, 2023. Web fep blue focus prior approval list. Web most drugs are covered without requiring prior approval. Effective august 14, 2023, fep members will also be participating in the surgical and implantable. View and download our medical, pharmacy and overseas claim forms. Case management is also required. If you have questions regarding the list,. Providers must obtain prior approval for the services below for fep standard and basic. Web 2023 fep prior approval drug list rev. Web home health/home infusion therapy/hospice: Web this guideline specifically addresses clinical review for prior approval of high technology diagnostic imaging requests for ct, mri and pet examinations. Ad register and subscribe now to work on your blue advantage med part d prescriptn drug auth. Edit, sign and save blue prescriptn drug auth form. This page provides prior approval requirements, contact information, and forms for the. Web this guideline specifically addresses clinical review for prior approval of high technology diagnostic imaging requests for ct, mri and pet examinations. 1 results found for search term : Web fep blue focus prior approval list. However, some select drugs require your doctor to provide information about your prescription to determine coverage. If we approve the request for prior approval. Prior approval may be required for certain prescription drugs before they can be covered under the pharmacy. Web this guideline specifically addresses clinical review for prior approval of high technology diagnostic imaging requests for ct, mri and pet examinations. Web most drugs are covered without requiring prior approval. 9 30 23 cyclobenzaprine powder cyclocort cream, lotion, ointment 0.1%cyramz(amcinonide)a + d. If you have questions regarding the list,. Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral health (bh) preservice request and review process for. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Providers must obtain. Web a prior approval is required for the procedures listed below for both the fep standard and basic option plan and the fep blue focus plan. 1 results found for search term : Web prior approval must be renewed periodically. Web fep prior approval documents. 9 30 23 cyclobenzaprine powder cyclocort cream, lotion, ointment 0.1%cyramz(amcinonide)a + d dalmane daptomycin econazole. Case management is also required. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web fep prior approval documents. Web prior approval is the process of determining the medical necessity of elective services. For more information about pharmacy prior approval and the required. Web fep blue focus prior approval list. View and download our medical, pharmacy and overseas claim forms. For enrollment codes 131, 132, 133 (on the member’s id card). Web this guideline specifically addresses clinical review for prior approval of high technology diagnostic imaging requests for ct, mri and pet examinations. Prior approval may be required for certain prescription drugs before. Case management is also required. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web this guideline specifically addresses clinical review for prior approval of high technology diagnostic imaging requests for ct, mri and pet examinations. This page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Prior. This page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web most drugs are covered without requiring prior approval. View and download our medical, pharmacy and overseas claim forms. Web spine services program participation to begin august 14, 2023. Web starting in 2024, members with medicare part a and/or part b will be eligible to enroll in our new medicare part d drug plan that offers additional approved prescription drugs in. Web prior approval pharmacy forms. Ad register and subscribe now to work on your blue advantage med part d prescriptn drug auth. Web your pharmacy coverage works outside the u.s., too*. For more information about pharmacy prior approval and the required forms visit the prior approval page. Effective august 14, 2023, fep members will also be participating in the surgical and implantable. Providers must obtain prior approval for the services below for fep standard and basic. For enrollment codes 131, 132, 133 (on the member’s id card). Case management is also required. Web prior approval is the process of determining the medical necessity of elective services. Web this guideline specifically addresses clinical review for prior approval of high technology diagnostic imaging requests for ct, mri and pet examinations. Edit, sign and save blue prescriptn drug auth form. Web fep blue focus prior approval list. Web prior approval must be renewed periodically. • special prior authorization situations related to coordination of. Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral health (bh) preservice request and review process for.FREE 11+ Prior Authorization Forms in PDF MS Word
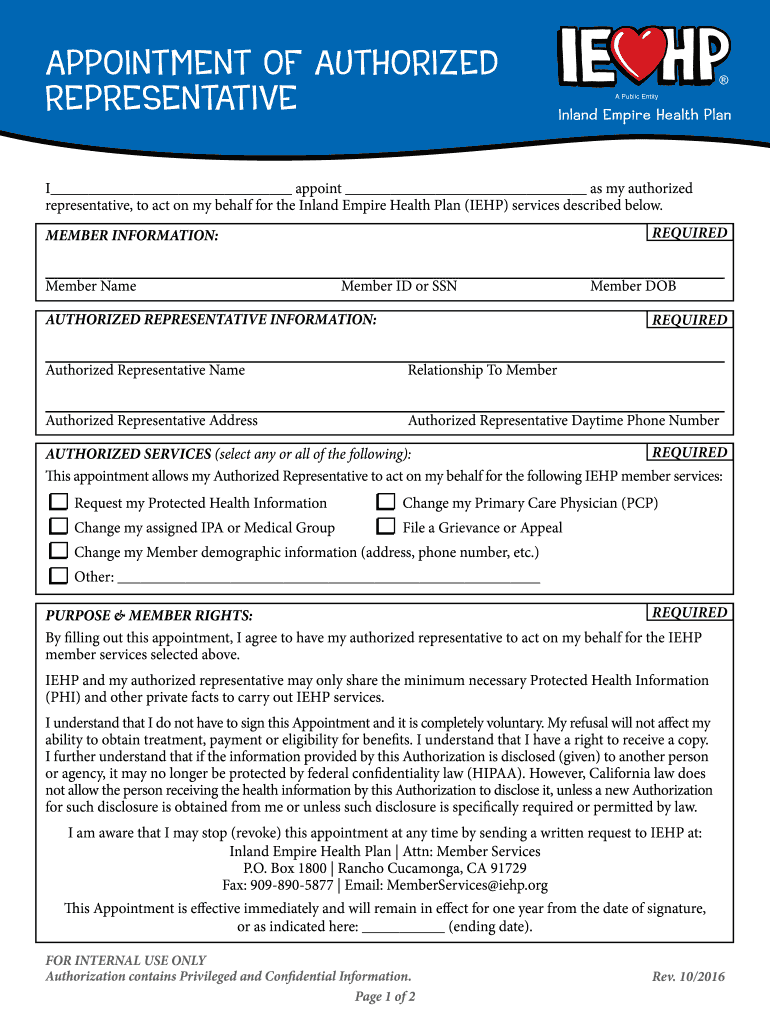
Iehp Authorized Representative Form Fill Out and Sign Printable PDF
How To Write A Prior Authorization Letter
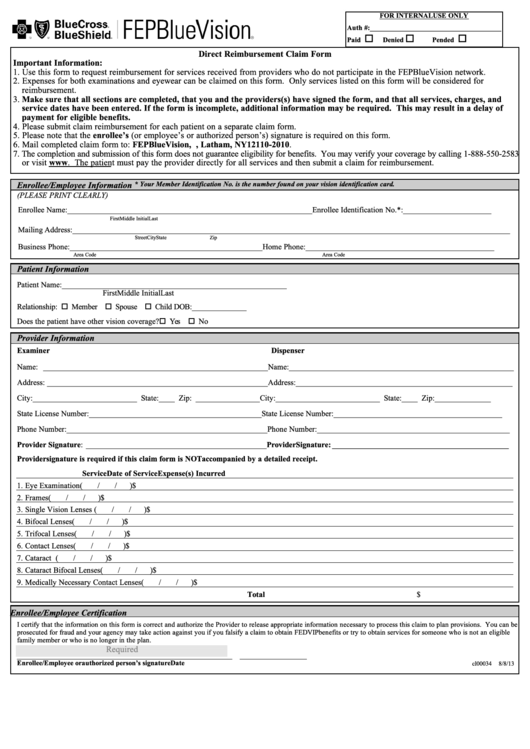
Fep Blue Fill Online, Printable, Fillable, Blank pdfFiller
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Optumrx Prior Auth Form Fill Out and Sign Printable PDF Template
Direct Reimbursement Claim Form Fep Bluevision printable pdf download
FREE 11+ Prior Authorization Forms in PDF MS Word
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Bcbs Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Related Post: