Blue Cross Blue Shield Fep Prior Authorization Form
Blue Cross Blue Shield Fep Prior Authorization Form - Web prior approval pharmacy forms. Web call the national information center at weekdays from 8 a.m. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800. Web members of the federal employee blue cross/blue shield service benefit plan (fep) are subject to different prior authorization requirements. Explore prior approval topics learn about prior. Effective august 14, 2023, fep members will also be participating in the surgical and implantable. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web fep blue focus prior approval list. Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. Web a prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure, service, or supply is provided. Web blue cross and blue shield federal employee program ® forms use these forms to obtain prior authorization for administering medications in physician's offices and. Get access to over 55,000 retail pharmacies. Effective august 14, 2023, fep members will also be participating in the surgical and implantable. Web pharmacy the blue cross and blue shield service benefit plan has a. Web blue shield ® service benefit plan and blue cross ® and blue shield ® service b enefit plan fep ® blue focus brochures.) covered facilities must meet. 1 results found for search term : Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). To prevent any delay in the review process,. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800. Web the specific effective date will be noted for each change that is posted. Web members of the federal employee blue cross/blue shield service benefit plan (fep) are subject to different prior authorization requirements. Web fep ppo. Alaska prior approval form washington prior. For more information about pharmacy prior approval and the required forms visit the prior approval page. Please complete a separate claim form for each patient and each pharmacy. Web pharmacy the blue cross and blue shield service benefit plan has a variety of pharmacy programs to meet your prescription needs. To view this information,. Each claim form must be signed. Get access to over 55,000 retail pharmacies. Effective august 14, 2023, fep members will also be participating in the surgical and implantable. Web authorization is hereby given to any provider of service, which participated in any way in my care, to release to the blue cross and blue shield plan any medical information. Web. Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral health (bh) preservice request and review process for. Web blue cross and blue shield federal employee program ® forms use these forms to obtain prior authorization for administering medications in physician's offices and. Web the specific effective date will be noted for each change. Blue cross and blue shield service benefit plan 750 9th street nw washington,. Get access to over 55,000 retail pharmacies. Web the address for the blue cross and blue shield service benefit plan administrative office is: Fep medicare prescription drug program (mpdp). To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the. Explore prior approval topics learn about prior. For more information about pharmacy prior approval and the required forms visit the prior approval page. To prevent any delay in the review process, please ensure the form is filled out completely, signed and dated, and included with the dispute request. Effective august 14, 2023, fep members will also be participating in the. Most drugs are covered without requiring prior approval. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web drug prior approval is a process to obtain advanced approval of coverage for a prescription drug. Remember to submit room rate updates 30 days prior to implementing the material change. Alaska prior approval form washington. Get access to over 55,000 retail pharmacies. Web drug prior approval is a process to obtain advanced approval of coverage for a prescription drug. Important contact information for blue cross and blue shield of arizona. To prevent any delay in the review process, please ensure the form is filled out completely, signed and dated, and included with the dispute request.. Web call the national information center at weekdays from 8 a.m. Web fep ppo prescription drug prior authorization or step therapy exception request form plan/medical group name: Blue cross and blue shield service benefit plan 750 9th street nw washington,. Important contact information for blue cross and blue shield of arizona. Web a prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment, procedure, service, or supply is provided. Web fep blue focus prior approval list. *cvs caremark is an independent company that provides pharmacy benefit. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Most drugs are covered without requiring prior approval. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800. Web the address for the blue cross and blue shield service benefit plan administrative office is: Web authorization is hereby given to any provider of service, which participated in any way in my care, to release to the blue cross and blue shield plan any medical information. Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral health (bh) preservice request and review process for. Web spine services program participation to begin august 14, 2023. Get access to over 55,000 retail pharmacies. Web prior approval must be renewed periodically. Web blue cross and blue shield federal employee program ® forms use these forms to obtain prior authorization for administering medications in physician's offices and. Web drug prior approval is a process to obtain advanced approval of coverage for a prescription drug. 2023 open season see what’s new take a look at the changes and updates. Please use the hospital room rate update form available on the.Fep Blue Fill Online, Printable, Fillable, Blank pdfFiller
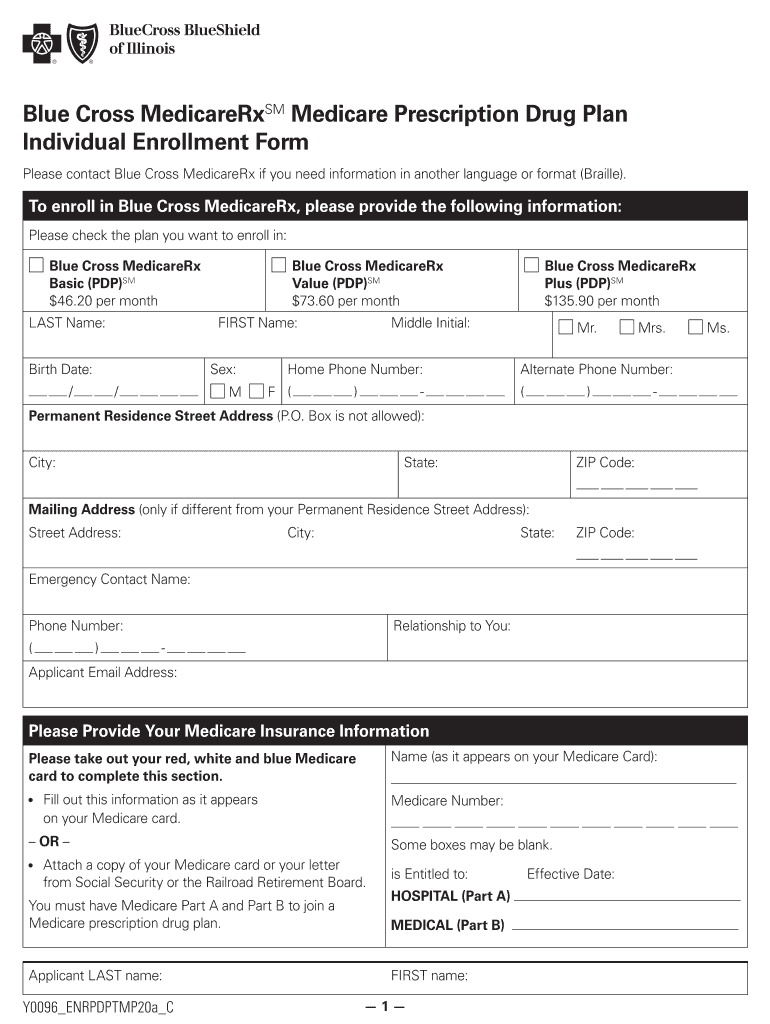
IL Blue Cross Blue Shield Prescription Drug Plan Individual Enrollment
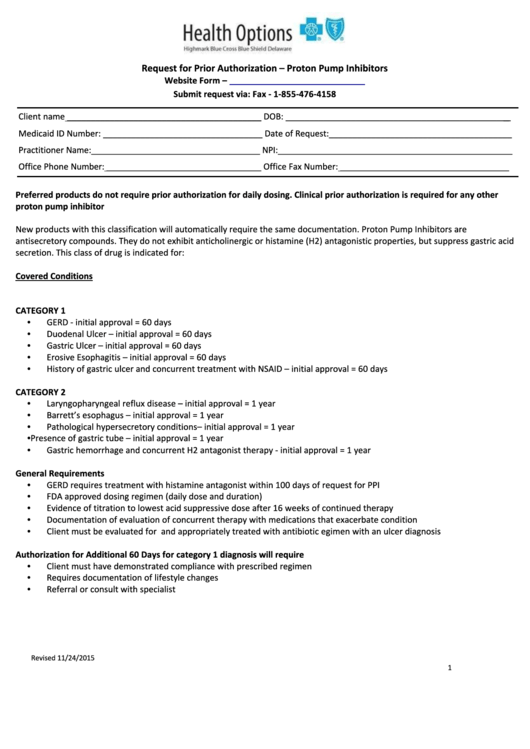
Request For Prior Authorization Form Proton Pump Inhibitors
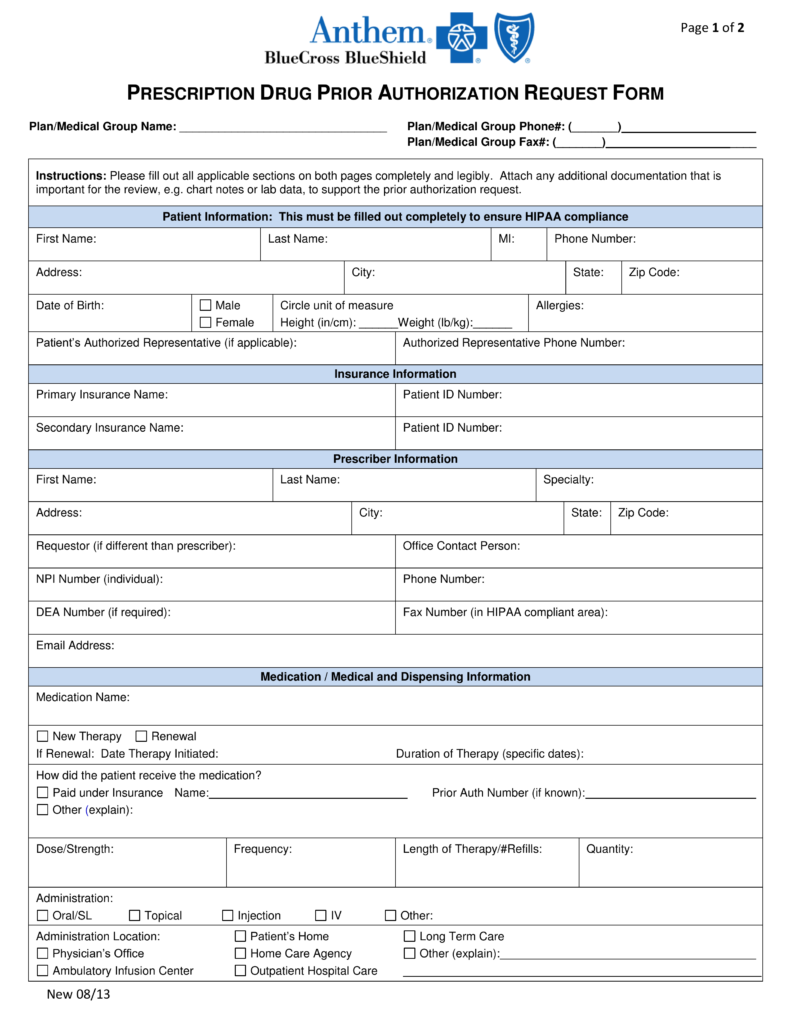
Free Anthem (Blue Cross Blue Shield) Prior (Rx) Authorization Form
Blue cross blue shield anthem eft enrollment form Fill out
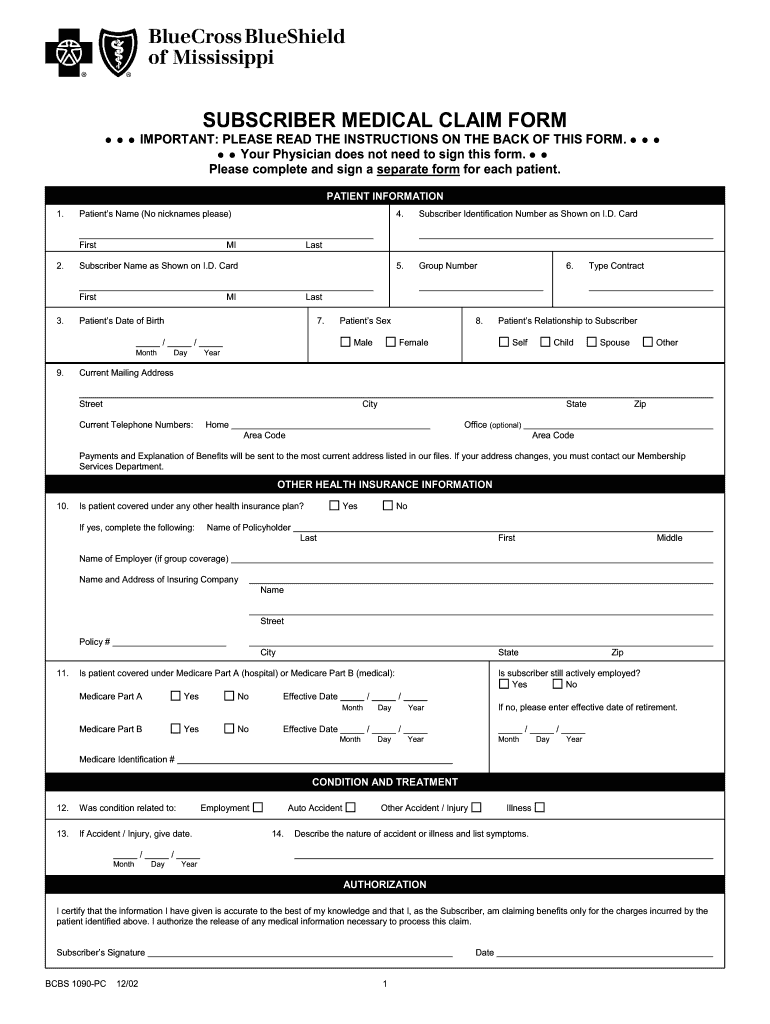
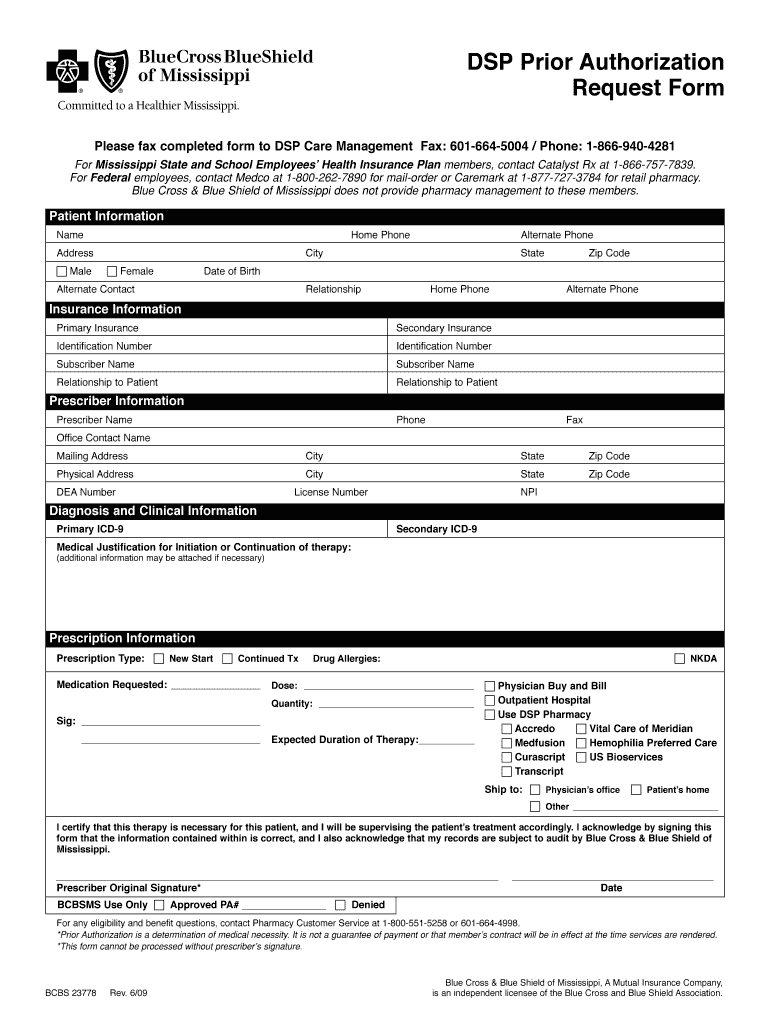
Mississippi Bluecross Blueshield Fill Out and Sign Printable PDF
Highmark blue shield prescription forms
Fill Free fillable Blue Cross and Blue Shield of Texas PDF forms
Bcbs mississippi prior authorization Fill out & sign online DocHub
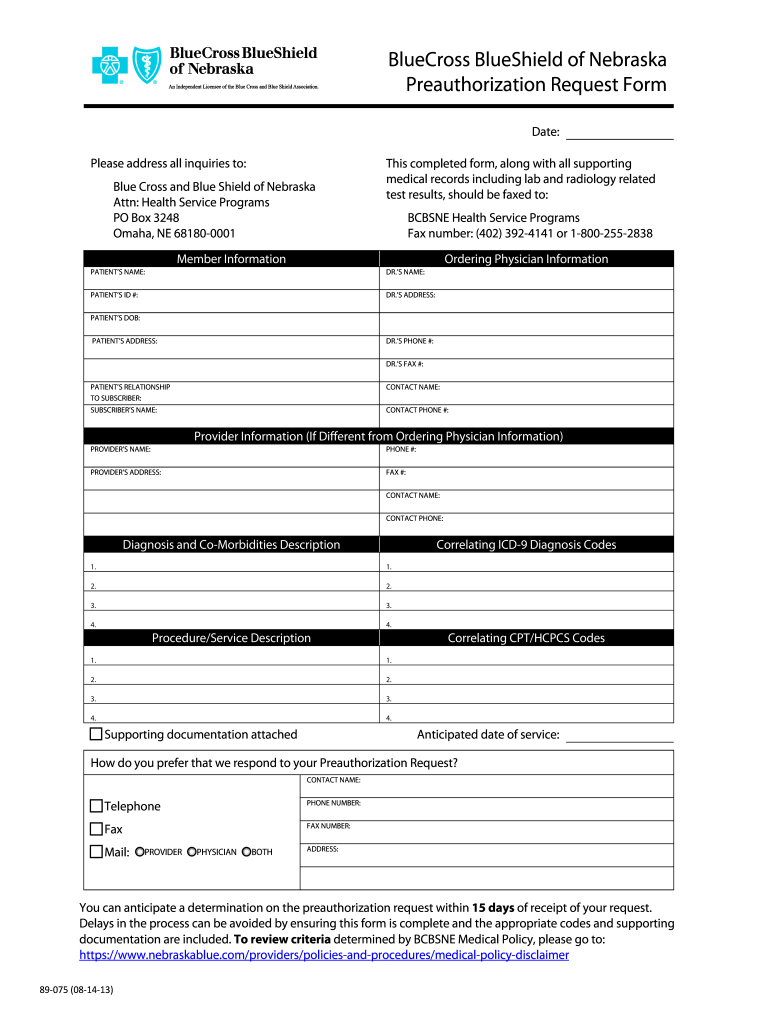
HSP Preauthorization Form Nebraska Blue Com Blue Cross Blue Fill Out
Related Post: