Benecard Prior Authorization Form
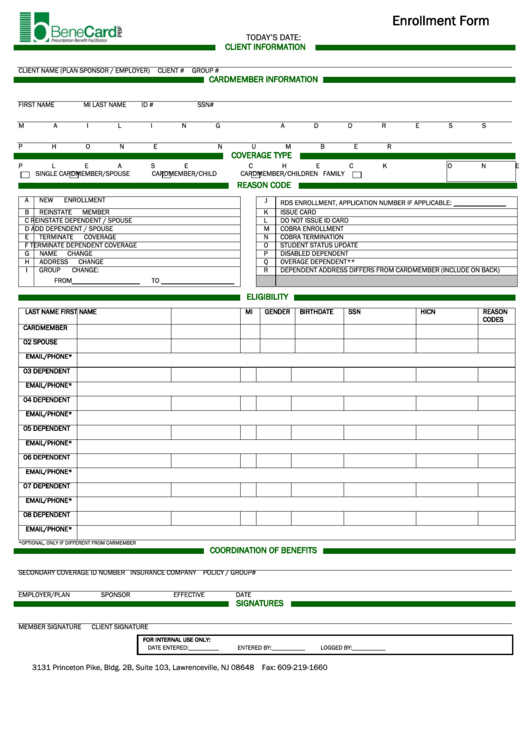
Benecard Prior Authorization Form - Our role is to help. Web find the benecard prior authorization form you require. You can access your plan’s formulary. We understand that behind each claim there is a person who needs our attention. The process begins by submitting the request to benecard. Web benecard prescription benefit facilitator information on mac for members for clients for professionals for pharmacy providers documents mac pricing / appeals pharmacy. Benecard services, llc is a full service, in house prescription benefit administrator that includes mail and specialty drug dispensing. Web we believe in providing a better experience for the patient and everyone involved in patient care. Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. At benecard services, our top priority is to ensure safety and healthier living. Concerned parties names, places of residence and. Working together, benecard pbf, pharmacies, and healthcare providers help. The process begins by submitting the request to benecard. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Clinical review for prior authorization; Open it with online editor and start altering. Empirx health reaches out to your doctor to. Use get form or simply click on the template preview to open it in the editor. Please call the number on the back of your id card or. Our role is to help. Web by submitting this form, you are consenting to receive marketing emails from: Concerned parties names, places of residence and. Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. Use get form or simply click on the template preview to open it in the editor. Web benefit programs since 1990. Please call the number on the back of your id card or. Working together, benecard pbf, pharmacies, and healthcare providers help. We understand that behind each claim there is a person who needs our attention. Use get form or simply click on the template preview to open it in the editor. At benecard services, our top priority is to ensure. Benecard services, llc is a full service, in house prescription benefit administrator that includes mail and specialty drug dispensing. Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. Our role is to help. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Use get form or. Web benefit programs since 1990. At benecard services, our top priority is to ensure safety and healthier living. We understand that behind each claim there is a person who needs our attention. Web authorization before benecard pbf actually receives my request to revoke the authorization. Working together, benecard pbf, pharmacies, and healthcare providers help. Web we focus on fast and accurate claims processing, easy access to information, clear and concise remittance statements, and timely authorization processes. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Please call the number on the back of your id card or. Open it with online editor and start altering. Use get form or. Clinical review for prior authorization; Open it with online editor and start altering. Concerned parties names, places of residence and. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Web by submitting this form, you are consenting to receive marketing emails from: Web we focus on fast and accurate claims processing, easy access to information, clear and concise remittance statements, and timely authorization processes. Benecard services, llc is a full service, in house prescription benefit administrator that includes mail and specialty drug dispensing. Web by submitting this form, you are consenting to receive marketing emails from: Web benefit programs since 1990. Clinical. Working together, benecard pbf, pharmacies, and healthcare providers help. Updates typically take effect in january and july. We understand that behind each claim there is a person who needs our attention. Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. Web benecard prescription benefit facilitator information on mac for members for. The process begins by submitting the request to benecard. Web benecard prescription benefit facilitator information on mac for members for clients for professionals for pharmacy providers documents mac pricing / appeals pharmacy. Web benefit programs since 1990. Open it with online editor and start altering. Benecard services, llc is a full service, in house prescription benefit administrator that includes mail and specialty drug dispensing. Please call the number on the back of your id card or. We understand that behind each claim there is a person who needs our attention. Web we believe in providing a better experience for the patient and everyone involved in patient care. Web by submitting this form, you are consenting to receive marketing emails from: Concerned parties names, places of residence and. Web find the benecard prior authorization form you require. Web authorization before benecard pbf actually receives my request to revoke the authorization. You can access your plan’s formulary. Our role is to help. Clinical review for prior authorization; Working together, benecard pbf, pharmacies, and healthcare providers help. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Web we focus on fast and accurate claims processing, easy access to information, clear and concise remittance statements, and timely authorization processes. Web a prior authorization reject means that the medication requires a diagnosis and information from the treating physician. Clinical review for prior authorization;Free Medicaid (Rx) Prior Authorization Forms PDF eForms
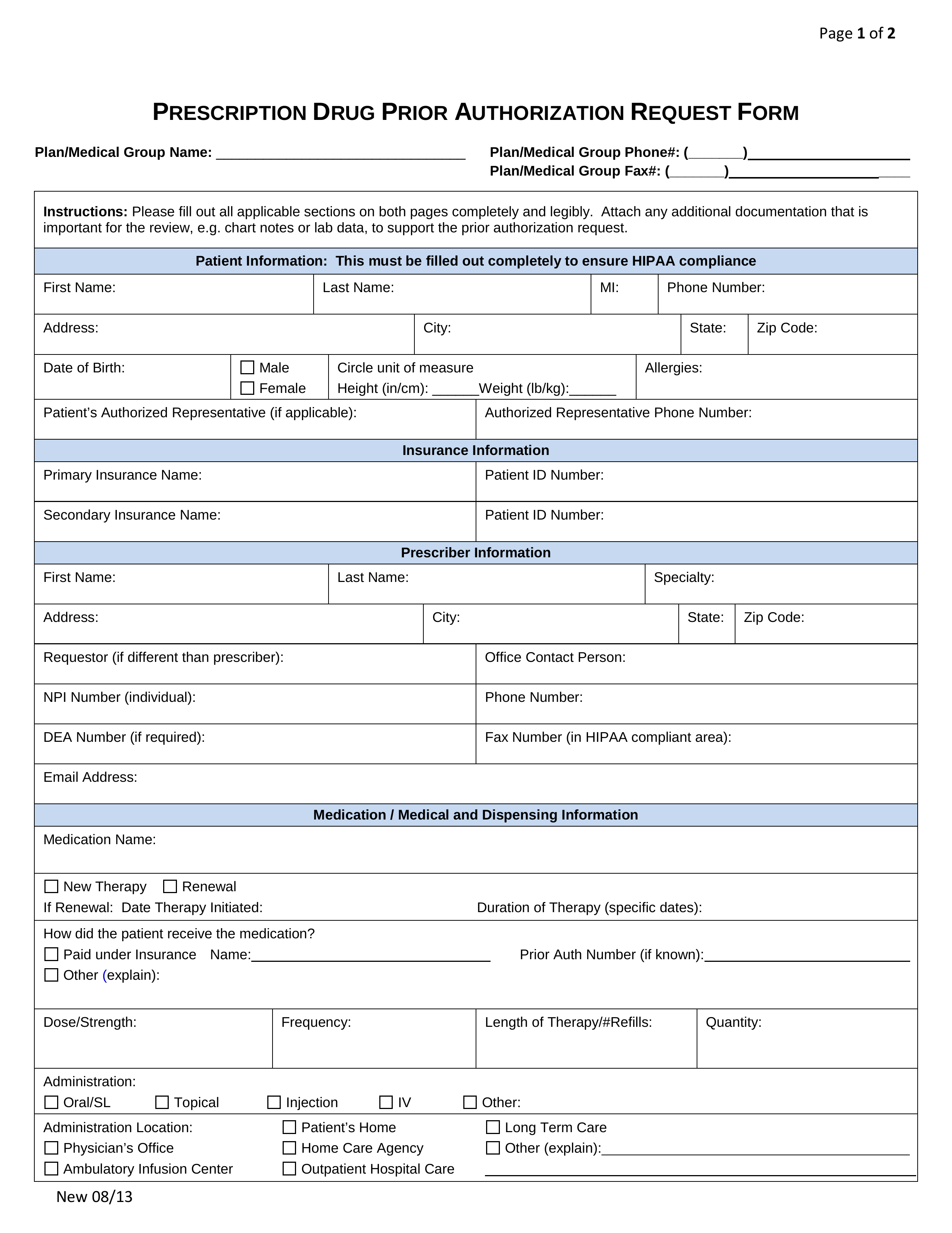
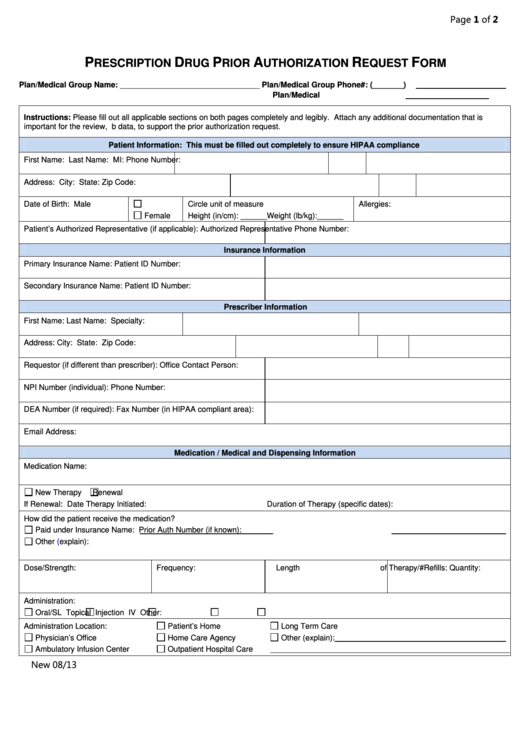
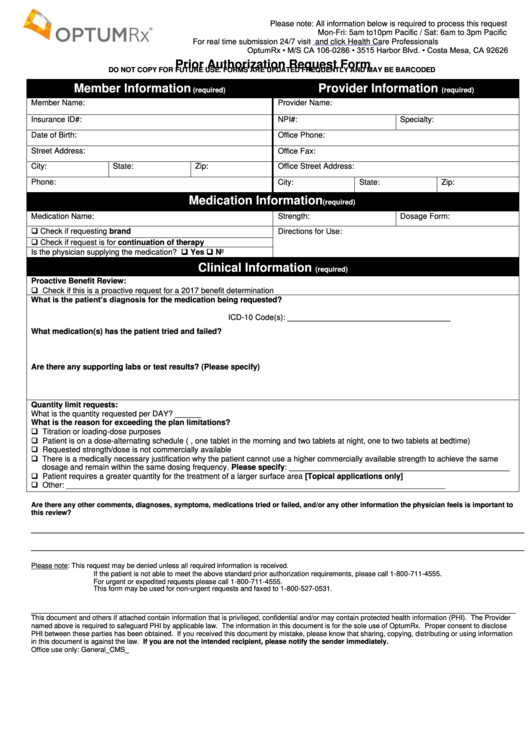
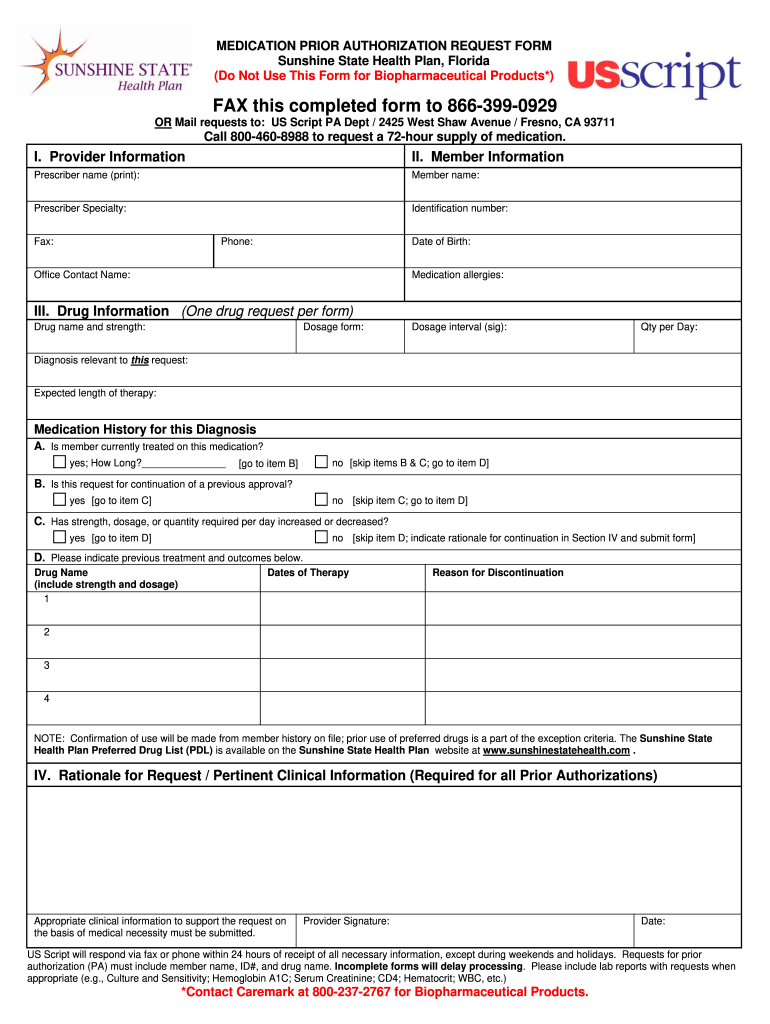
Fillable Prescription Drug Prior Authorization Request Form printable
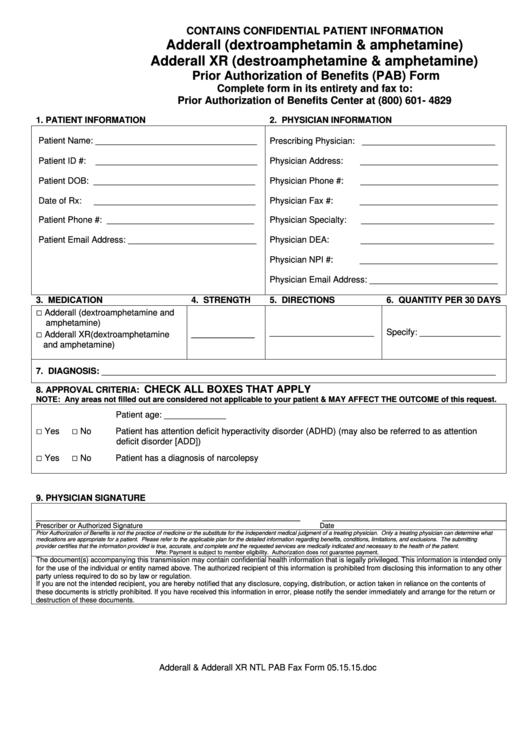
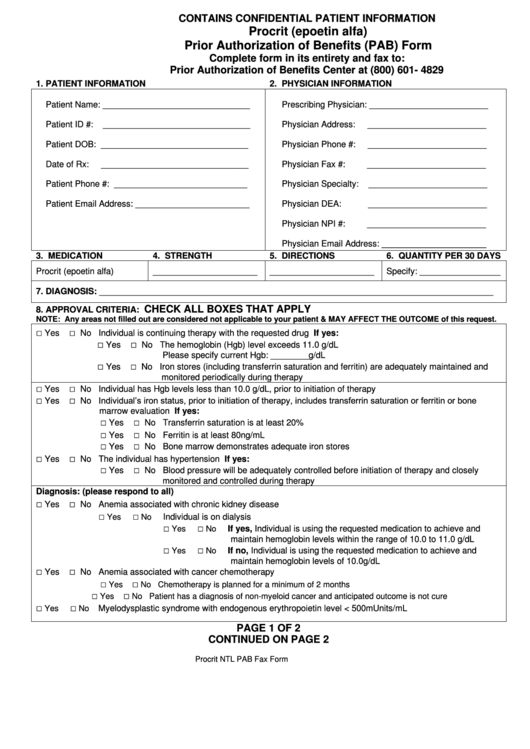
Prior Authorization Of Benefits (Pab) Form printable pdf download
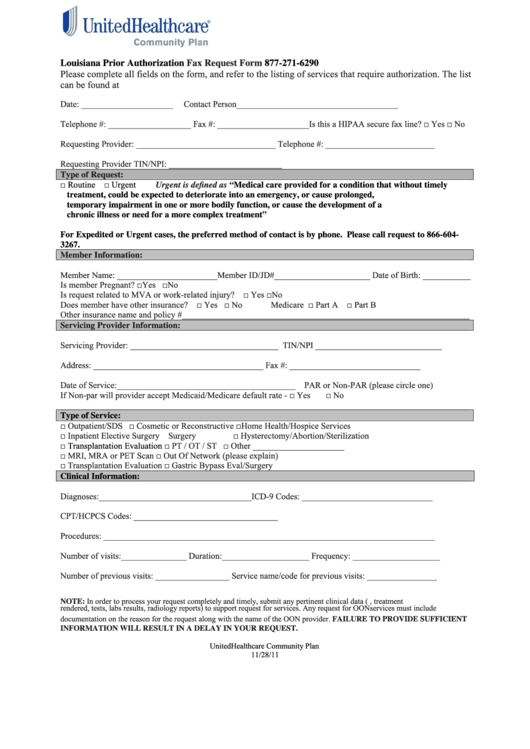
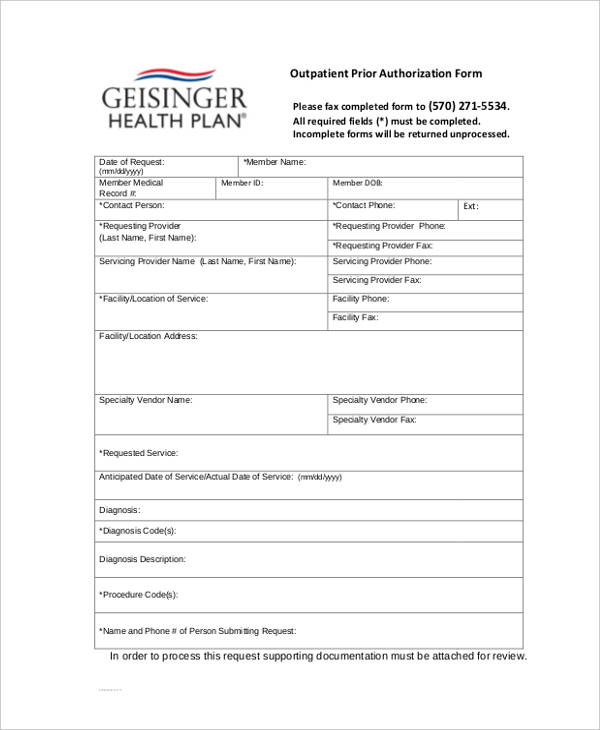
Fillable Louisiana Prior Authorization Fax Request Form printable pdf
Procrit (Epoetin Alfa) Prior Authorization Of Benefits (Pab) Form
Prior Authorization Request Form printable pdf download
Benecard Enrollment Form printable pdf download
FREE 13+ Prior Authorization Forms in PDF MS Word
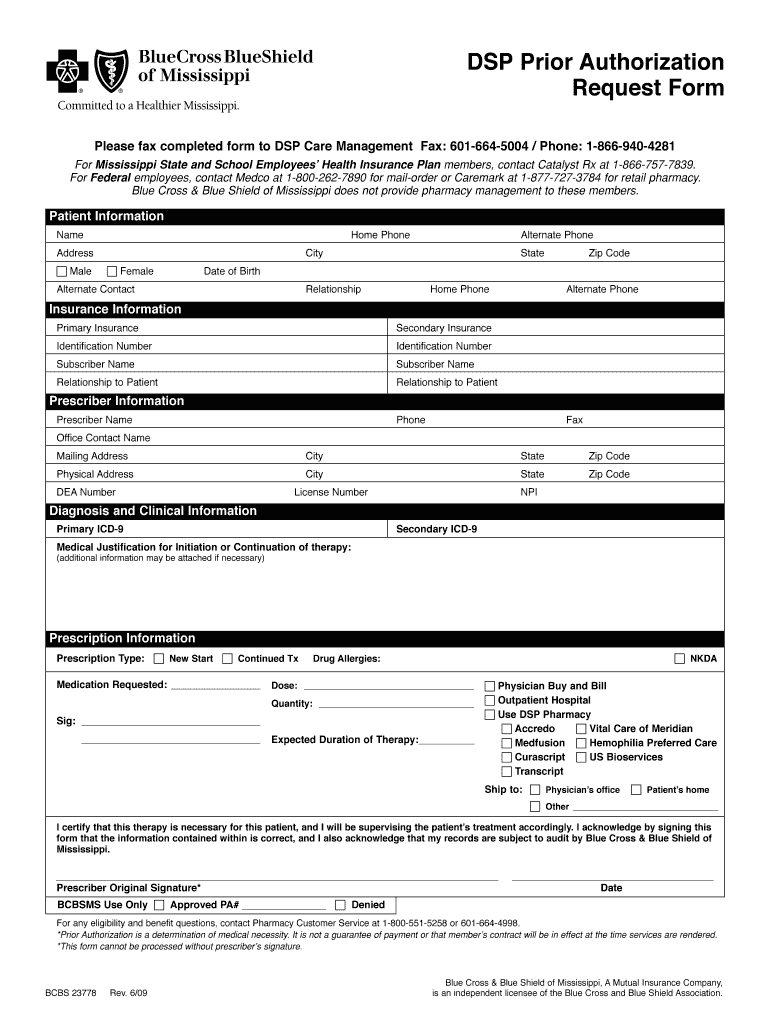
Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
Surescripts Prior Auth Printable Form Printable Form, Templates and
Related Post: