Affinity By Molina Prior Authorization Form
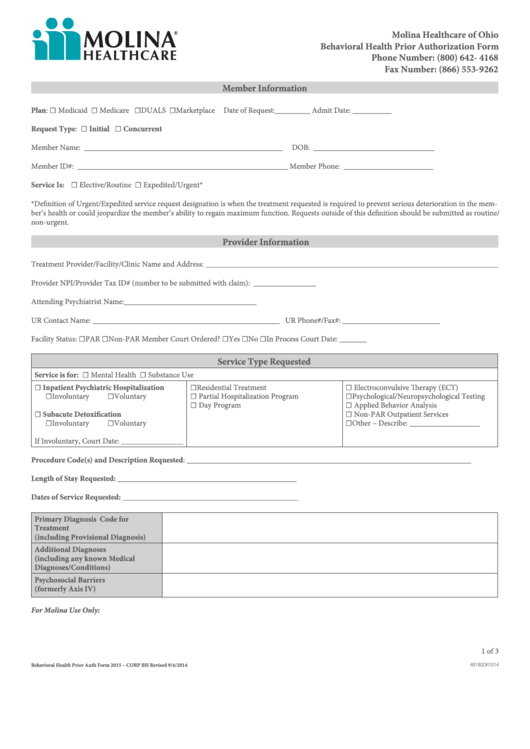
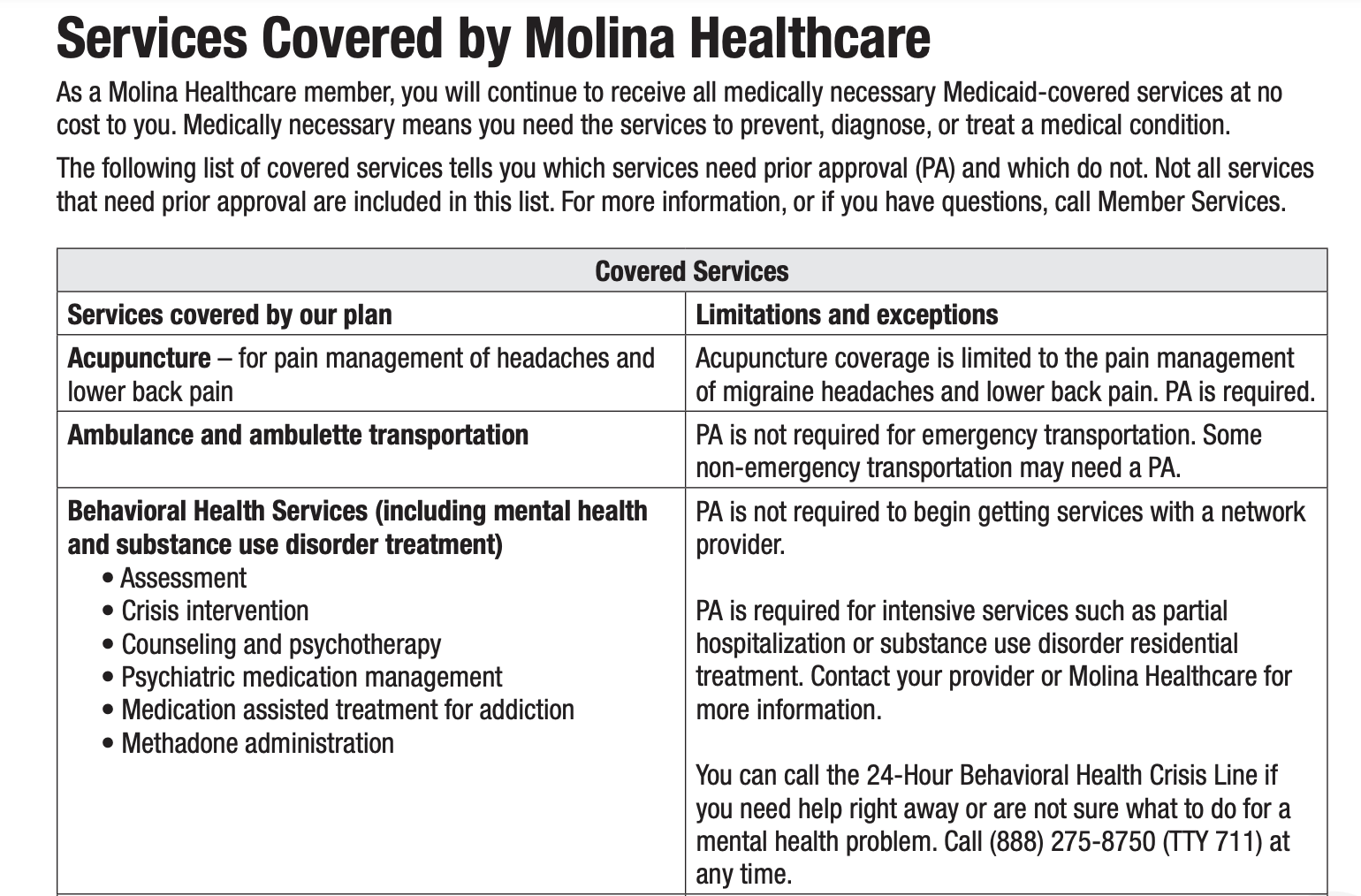
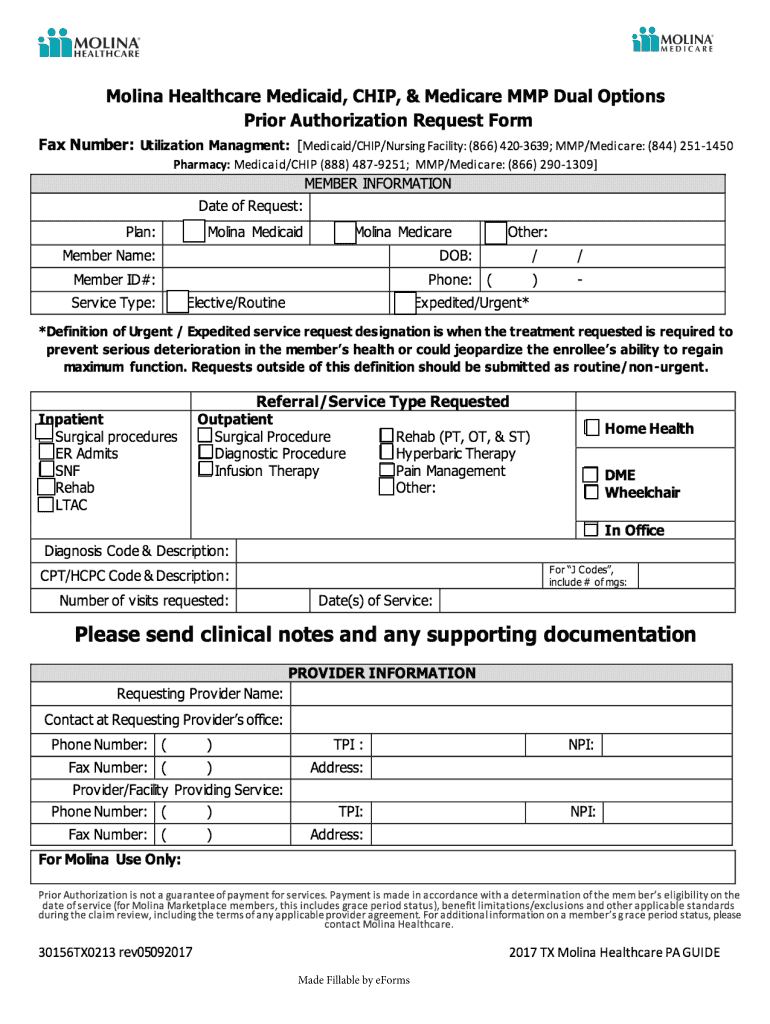
Affinity By Molina Prior Authorization Form - Web welcome to affinity by molina healthcare! 01/01/2022 refer to molina’s provider. Web do you need to add, terminate, or make demographic changes to an existing provider in your group? Web referrals and authorizations in accordance with mental plan requirement and affinity policy, certainly services require prior authorization before benefit can be offered by. Web home > members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? 10/01/2021 refer to molina’s provider website or. Web behavioral health prior authorization form. If you have questions or suggestions, please contact us. If you think that affinity by molina healthcare failed to. Should an unlisted or miscellaneous code be requested, medical. Web therapies, please direct prior authorization requests to novologix via the molina provider portal. Web referrals and authorizations in accordance with mental plan requirement and affinity policy, certainly services require prior authorization before benefit can be offered by. Web molina healthcare prior (rx) authorization form. Both affinity by molina healthcare and molina healthcare of new york,. Web molina requires standard. Children's cftss notification of service and concurrent auth form. Prior authorization is when your provider. Web at molina complete care, we value you as a provider in our network. Web behavioral health prior authorization form. Web home > members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? Let us connect you to the best quality care for you and your family register today Web molina healthcare prior (rx) authorization form. All pertinent community information (name, id #, class #, and member's giving date) pcp information. Please notify molina healthcare at least 30 days in advance. If you have questions or suggestions, please contact us. Web molina requires standard codes when requesting authorization. Web do you need to add, terminate, or make demographic changes to an existing provider in your group? Web provider self services * when prior authorization is 'required', click sra create to create service request/authorization error! Let us connect you to the best quality care for you and your family register today. Web provider resources > forms forms here you can find all your provider forms in one place. Both affinity by molina healthcare and molina healthcare of new york,. Web if you need these services, contact affinity by molina. Affinity health plan plan/pbm phone no. Web welcome to affinity by molina healthcare! Affinity health plan plan/pbm phone no. Both affinity by molina healthcare and molina healthcare of new york,. Affinity by molina healthcare is here to help you get coverage. Web provider resources > forms forms here you can find all your provider forms in one place. 10/01/2021 refer to molina’s provider website or. Children's cftss notification of service and concurrent auth form. Web do you need to add, terminate, or make demographic changes to an existing provider in your group? All pertinent community information (name, id #, class #, and member's giving date) pcp information. Covermymeds is affinity prior authorization forms’s preferred method for receiving. Web behavioral health prior authorization form. If you think that affinity by molina healthcare failed to. Web referrals and authorizations in accordance with mental plan requirement and affinity policy, certainly services require prior authorization before benefit can be offered by. Covermymeds is affinity prior authorization forms’s preferred method for receiving. Web do you need to add, terminate, or make demographic changes to an existing provider in. 10/01/2021 refer to molina’s provider website or. Affinity by molina healthcare is here to help you get coverage. Prior authorization is when your provider. 01/01/2022 refer to molina’s provider. All pertinent community information (name, id #, class #, and member's giving date) pcp information. Web referrals and authorizations in accordance with mental plan requirement and affinity policy, certainly services require prior authorization before benefit can be offered by. Children's cftss notification of service and concurrent auth form. Web behavioral health prior authorization form. Let us connect you to the best quality care for you and your family register today Web if you need these. Web make sure the prior authorization request is complete and contains: Looking to enroll or renew your coverage with affinity by molina healthcare? Affinity by molina healthcare is here to help you get coverage. 10/01/2021 refer to molina’s provider website or. If you think that affinity by molina healthcare failed to. Affinity health plan plan/pbm phone no. Web molina healthcare prior (rx) authorization form. 01/01/2022 refer to molina’s provider. Web at molina complete care, we value you as a provider in our network. Should an unlisted or miscellaneous code be requested, medical. Please notify molina healthcare at least 30 days in advance. Web if you need these services, contact affinity by molina. Web home > members > medicaid > about medicaid > getting care > prior authorizations prior authorizations what are prior authorizations? If you have questions or suggestions, please contact us. Web referrals and authorizations in accordance with mental plan requirement and affinity policy, certainly services require prior authorization before benefit can be offered by. All pertinent community information (name, id #, class #, and member's giving date) pcp information. Prior authorization request form rationale for exception request or. Both affinity by molina healthcare and molina healthcare of new york,. Covermymeds is affinity prior authorization forms’s preferred method for receiving. Children's cftss notification of service and concurrent auth form.Fillable Molina Behavioral Health Prior Authorization Form Ohio
Molina Drug Prior Authorization Fill Online, Printable, Fillable
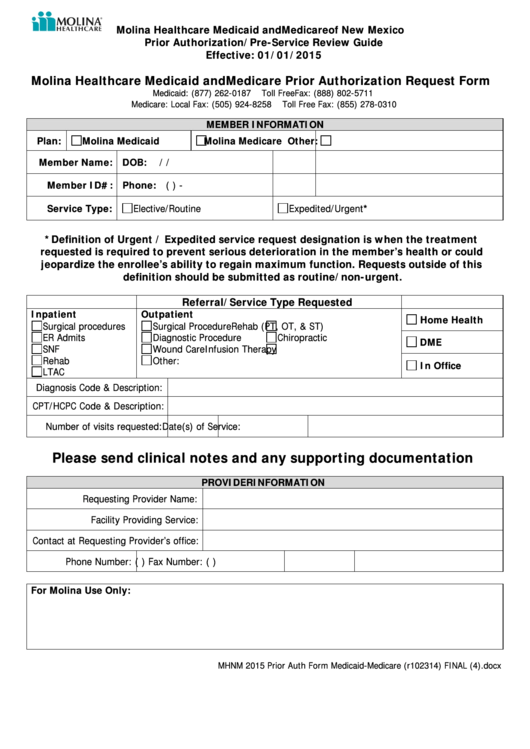
Gallery of Molina Healthcare Prior Authorization form New Mexico Lovely
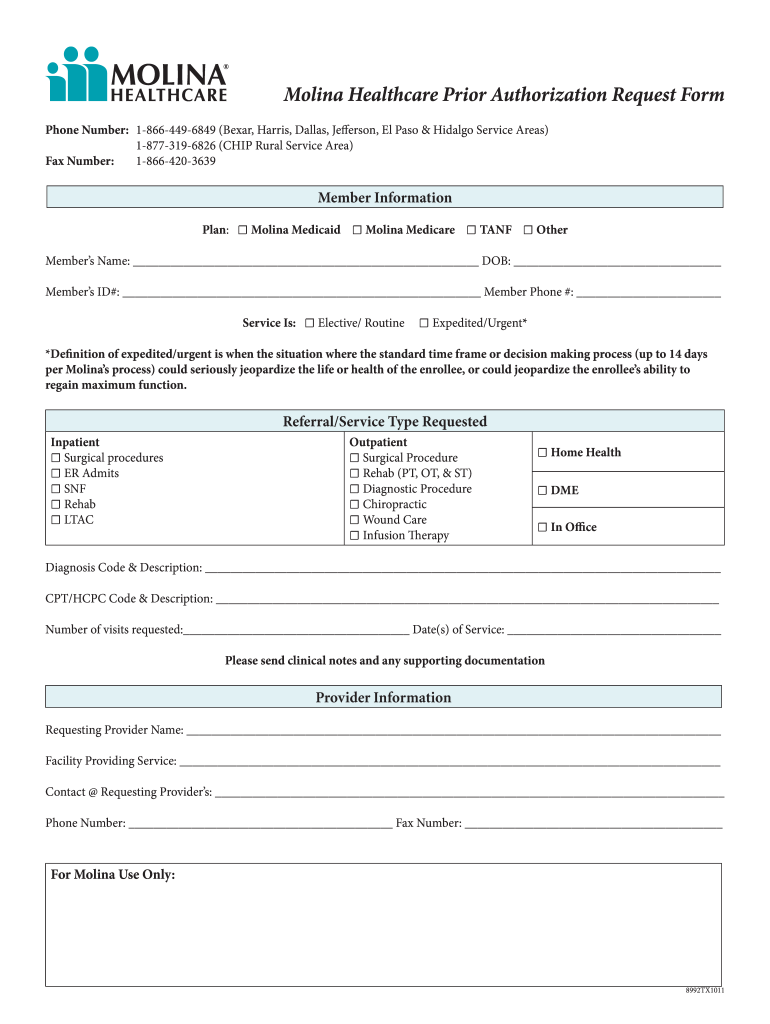
Molina Prior Authorization Request Form Fill Online
Molina Prior Authorization Form Fill Online, Printable, Fillable
Molina prior authorization form Fill out & sign online DocHub
Doing a PreCertification or Prior Authorization with Molina HealthCare
Molina Healthcare Medicaid And Medicare Prior Authorization Request
Doing a PreCertification or Prior Authorization with Molina HealthCare
Molina Prior Authorization Form Fill Out and Sign Printable PDF
Related Post: