Sunflower Prior Authorization Form
Sunflower Prior Authorization Form - You probably don't want to wait any later than that or else your sunflowers may not have a chance to. If necessary, qualified interpreters should be secured, the form should be available in the 15 most widely spoken languages in the patient’s area, and. Inpatient prior authorization form (pdf) outpatient prior authorization form (pdf) pregnancy and birth forms. Web prior authorization for services. Initial continuation if continuation, provide therapy start date: Has strength or daily dose changed? View our preferred drug list to see what drugs are covered. ★ ★ ★ ★ ★. Claim appeal / reconsideration request form (pdf). Prior authorization rules for medical benefits. Web prior authorization form complete and fax to: Web prior authorization for services. Prior authorization is a request made by you or your doctor to get wellcare by allwell medicare's approval before receiving treatment. To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or. Find everything you need in the member online. Prior authorization is a request made by you or your doctor to get wellcare by allwell medicare's approval before receiving treatment. You probably don't want to wait any later than that or else your sunflowers may not have a chance to. The requesting physician must complete an authorization request using one of the following methods: Permission is reversible and can. Optional form to report birth. Web prior authorization form complete and fax to: You probably don't want to wait any later than that or else your sunflowers may not have a chance to. Standard prior authorization requests should be submitted for medical necessity review at least five (5) business days before the scheduled service delivery date or as soon as. Standard prior authorization requests should be submitted for medical necessity review at least five (5) business days before the scheduled service delivery date or as soon as the need for service is identified. The last month that you can plant sunflowers and expect a good harvest is probably september. For questions, please call the pharmacy helpdesk specific to the member’s. Open form follow the instructions. Permission is reversible and can be. However, you really should wait until april if you don't want to take any chances. Sometimes, we need to approve medical services before you receive them. Web prior authorization for services. The requesting physician must complete an authorization request using one of the following methods: Web prior authorization for services. Sunflower prior auth tool rating. Web prior authorization form complete and fax to: Optional form to report birth. If necessary, qualified interpreters should be secured, the form should be available in the 15 most widely spoken languages in the patient’s area, and. Interested in becoming an ambetter provider? Web complete and fax to: Sunflower prior auth tool rating. View our preferred drug list to see what drugs are covered. Web inpatient prior authorization fax form (pdf) intensive outpatient/day treatment authorization form (pdf) outpatient prior authorization fax form (pdf) outpatient treatment request form (pdf) provider fax back form (pdf) applied behavioral analysis authorization form (pdf) birth event notification (pdf): Complete form in its entirety and fax to the appropriate plan’s pa department. Web kansas medicaid universal prior authorization form. Sunflower. Web complete and fax to: Send filled & signed form or save. Claim appeal / reconsideration request form (pdf). Web to submit a prior authorization login here. Web prior authorization for services. For questions, please call the pharmacy helpdesk specific to the member’s plan. Logging into the nch provider web portal. Standard prior authorization requests should be submitted for medical necessity review at least five (5) business days before the scheduled service delivery date or as soon as the need for service is identified. The last month that you can plant sunflowers. Claim appeal / reconsideration request form (pdf). This process is known as prior authorization. Web complete and fax to: The requesting physician must complete an authorization request using one of the following methods: Choose the appropriate medication request form below: Inpatient prior authorization form (pdf) outpatient prior authorization form (pdf) pregnancy and birth forms. To submit a prior authorization login here. Sunflower prior auth tool rating. Web prior authorization form complete and fax to: Web to submit a prior authorization login here. Ambetter from sunflower health plan oncology pathway solutions. For questions, please call the pharmacy helpdesk specific to the member’s plan. You probably don't want to wait any later than that or else your sunflowers may not have a chance to. View our preferred drug list to see what drugs are covered. Standard prior authorization requests should be submitted for medical necessity review at least five (5) business days before the scheduled service delivery date or as soon as the need for service is identified. To see if a service requires authorization, check with your primary care provider (pcp), the ordering provider or. Web use our prior authorization prescreen tool. Web prior authorization for services. Optional form to report birth. Initial continuation if continuation, provide therapy start date:Health Plan of San Mateo Prior Authorization Form Fill Out and Sign
Sunflower State Health Plan Prior Authroization Form
Medicare Generation Rx Prior Authorization Form Form Resume
Prior Authorization Form Fill Out and Sign Printable PDF Template
20182023 Form KS KSPAF0673Fill Online, Printable, Fillable, Blank
FREE 11+ Prior Authorization Forms in PDF MS Word
Banner University Prior Auth Form Fill Online, Printable, Fillable
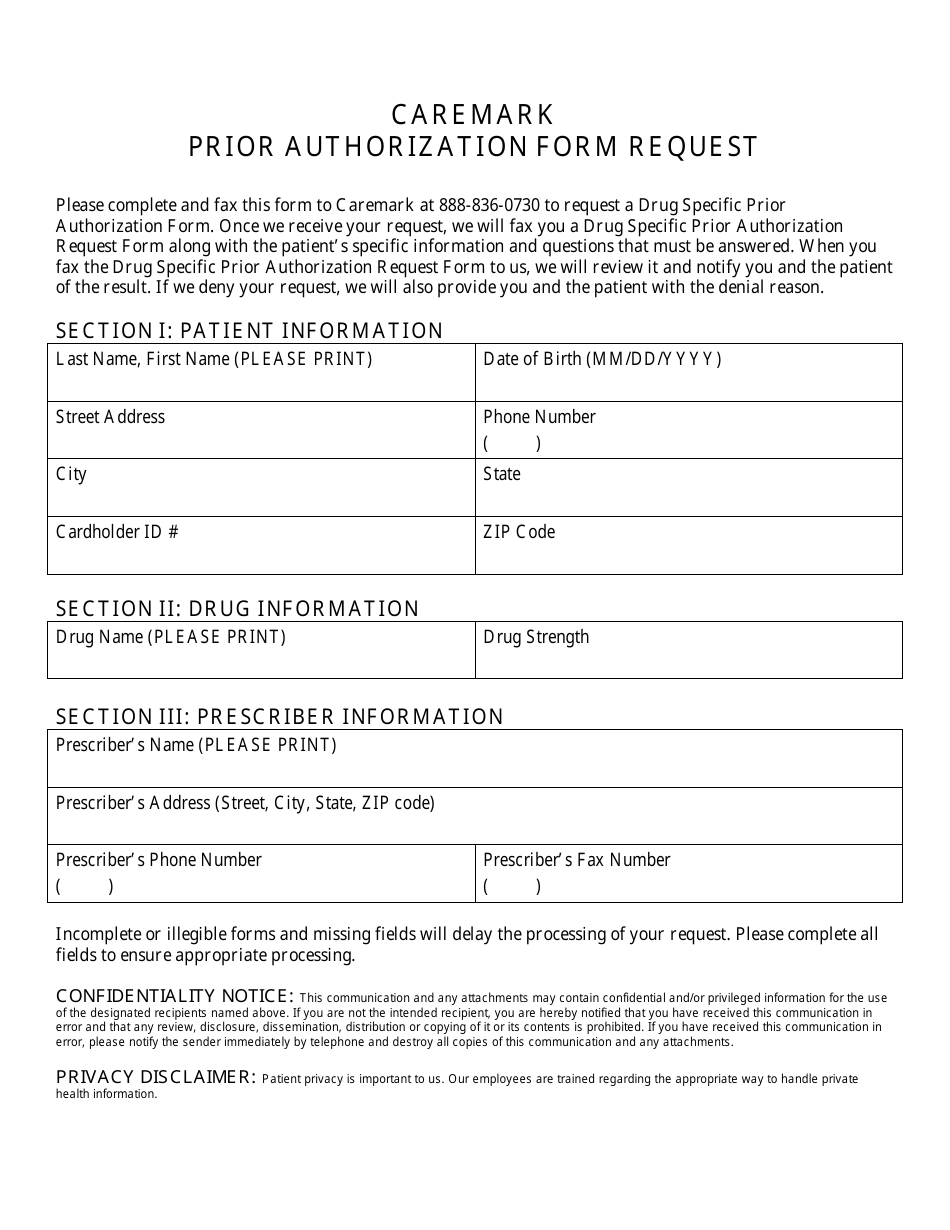
Prior Authorization Form Request Cvs Caremark Download Printable PDF
FREE 41+ Authorization Forms in PDF Excel MS word
Insurance Prior Authorization For Medication Stories Fix Prior Auth
Related Post: