Prior Authorization Form Aetna
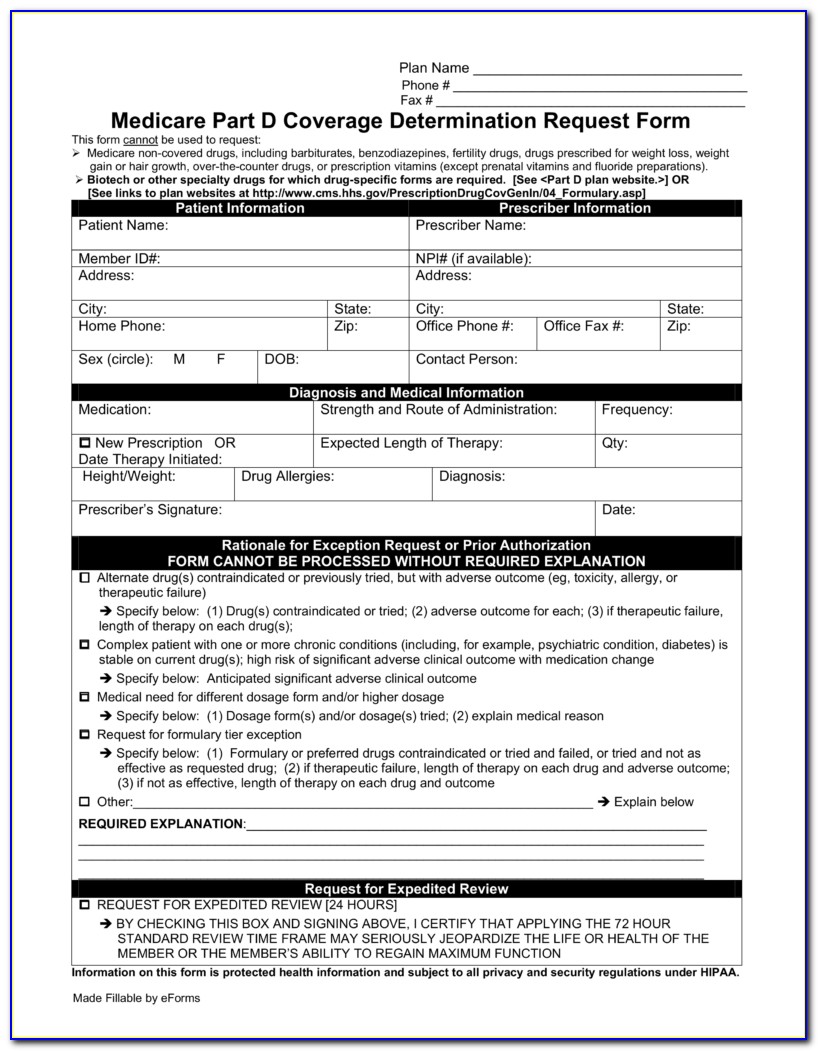
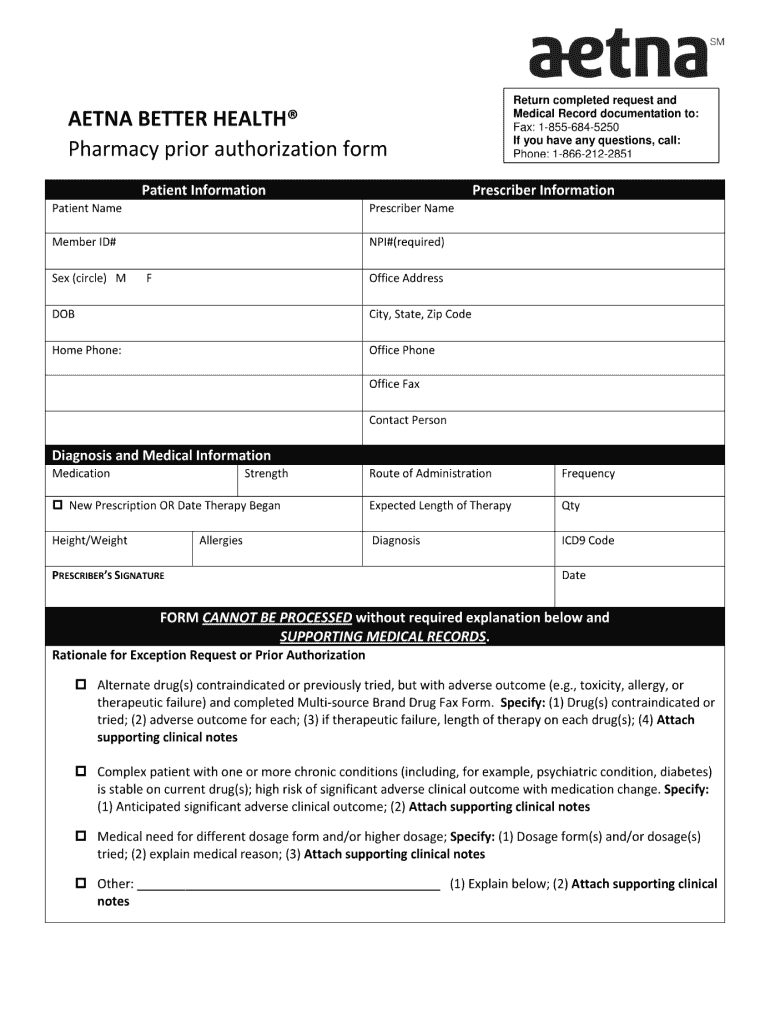
Prior Authorization Form Aetna - Prior authorization is required for select, acute outpatient services and planned hospital admissions. It means that aetna better. Learn how to request prior authorization here. Ad pdffiller.com has been visited by 1m+ users in the past month Notification of medical request — send us notification of. Ad signnow.com has been visited by 100k+ users in the past month Some care will require your doctor to get our approval first. Web medical exception/prior authorization/precertification* request for prescription medications. Pa is not needed for emergency care. The member has an aetna® fully insured commercial plan. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Pa is not needed for emergency care. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. It means that aetna better. Keying institutional claims in connectcenter. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. As an aetna better health provider, you need to prescribe medically necessary therapy or medications for a member. Web medical claim form (pdf) member complaint and appeal (pdf) pharmacy claim form (pdf) request for protected health information (phi) (pdf) revocation of. Ad pdffiller.com has. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Web site of service. Eylea® (aflibercept) injectable medication precertification request. Web medical claim form (pdf) member complaint and appeal (pdf) pharmacy claim form (pdf) request for protected health information (phi) (pdf) revocation of. Your clinical team or pcp requests prior authorization before. Web keying professional claims in connectcenter. Pa is not needed for emergency care. Learn how to request prior authorization here. Web what is prior authorization? Complete the texas standard prior authorization request form (pdf). Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Ad pdffiller.com has been visited by 1m+ users in the past month Web health benefits and health insurance plans contain exclusions and limitations. Complete the texas standard prior authorization request form (pdf). Web prior authorization (pa) aetna better health® of kentucky requires. Find and access provider related medicaid. Ad pdffiller.com has been visited by 1m+ users in the past month Web precertification — submit a precertification request for services that require utilization management (um) review. To submit a request, call our precertification. Notification of medical request — send us notification of. View and download provider related. Web (prior authorization needed for the drug and site of care): Your clinical team or pcp requests prior authorization before the service is rendered. Then, upload it to the provider portal. Web site of service. Ad signnow.com has been visited by 100k+ users in the past month Notification of medical request — send us notification of. This process is called prior authorization or preapproval. Web precertification — submit a precertification request for services that require utilization management (um) review. Web prior authorization (pa) aetna better health® of kentucky requires pa for some outpatient care, as. In these cases, your doctor can submit a request on your behalf to get that. Your clinical team or pcp requests prior authorization before the service is rendered. As an aetna better health provider, you need to prescribe medically necessary therapy or medications for a member. Web medical claim form (pdf) member complaint and appeal (pdf) pharmacy claim form (pdf). Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. As an aetna better health provider, you need to prescribe medically necessary therapy or medications for a member. Some care will require your doctor to get our approval first. Web prior authorization form all fields on this form are required. Notification of medical request. Get information about aetna’s precertification requirements, including. As an aetna better health provider, you need to prescribe medically necessary therapy or medications for a member. Eylea® (aflibercept) injectable medication precertification request. Cvs caremark prior authorization (pa) tools are developed to ensure safe, effective and appropriate use of selected drugs. Ad signnow.com has been visited by 100k+ users in the past month Learn how to request prior authorization here. Keying institutional claims in connectcenter. Web prior authorization is a request to aetna for you to get special services or see a specialist. Then, upload it to the provider portal. Prior authorization is required for select, acute outpatient services and planned hospital admissions. This process is called prior authorization or preapproval. Your clinical team or pcp requests prior authorization before the service is rendered. In these cases, your doctor can submit a request on your behalf to get that. Web precertification — submit a precertification request for services that require utilization management (um) review. Web what is prior authorization? Notification of medical request — send us notification of. Web medical claim form (pdf) member complaint and appeal (pdf) pharmacy claim form (pdf) request for protected health information (phi) (pdf) revocation of. Web keying professional claims in connectcenter. Complete the texas standard prior authorization request form (pdf). Ad pdffiller.com has been visited by 1m+ users in the past monthAetna xolair prior authorization form Fill out & sign online DocHub
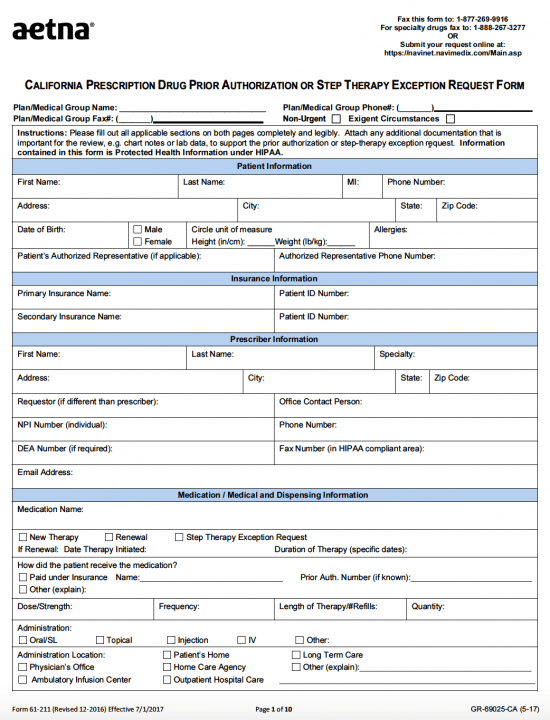
Free AETNA Prior Prescription (Rx) Authorization Form PDF
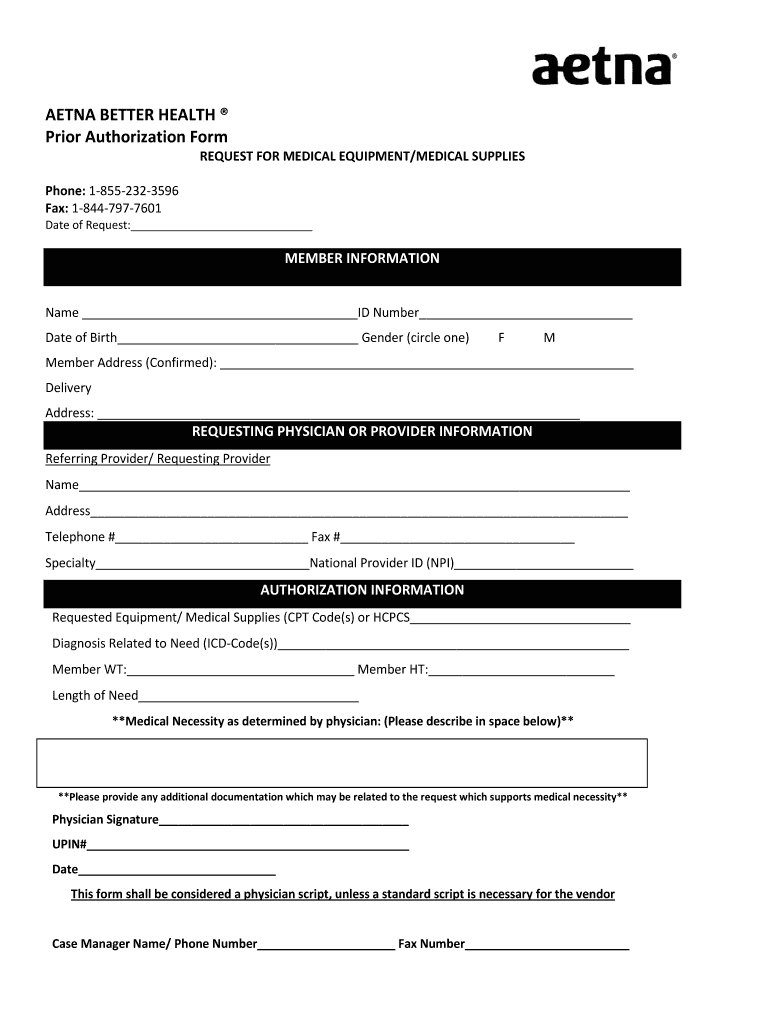
Aetna better health prior authorization form Fill out & sign online
Aetna Drug Plan Prior Authorization Form
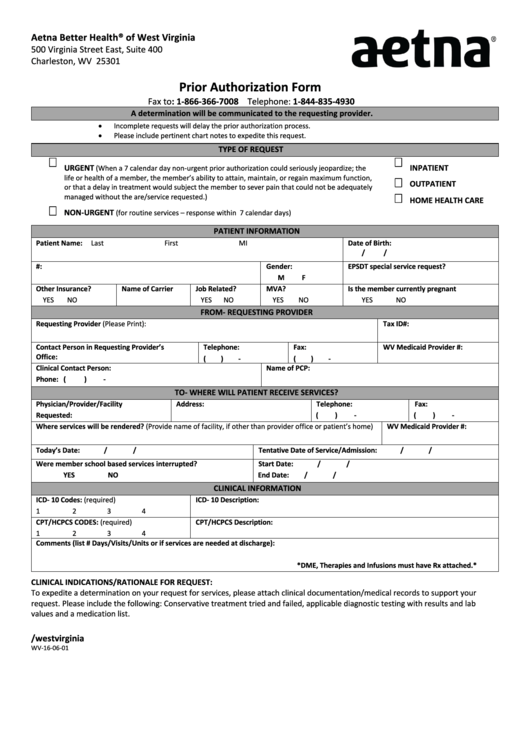
From Wv160601 Aetna Prior Authorization Form printable pdf download
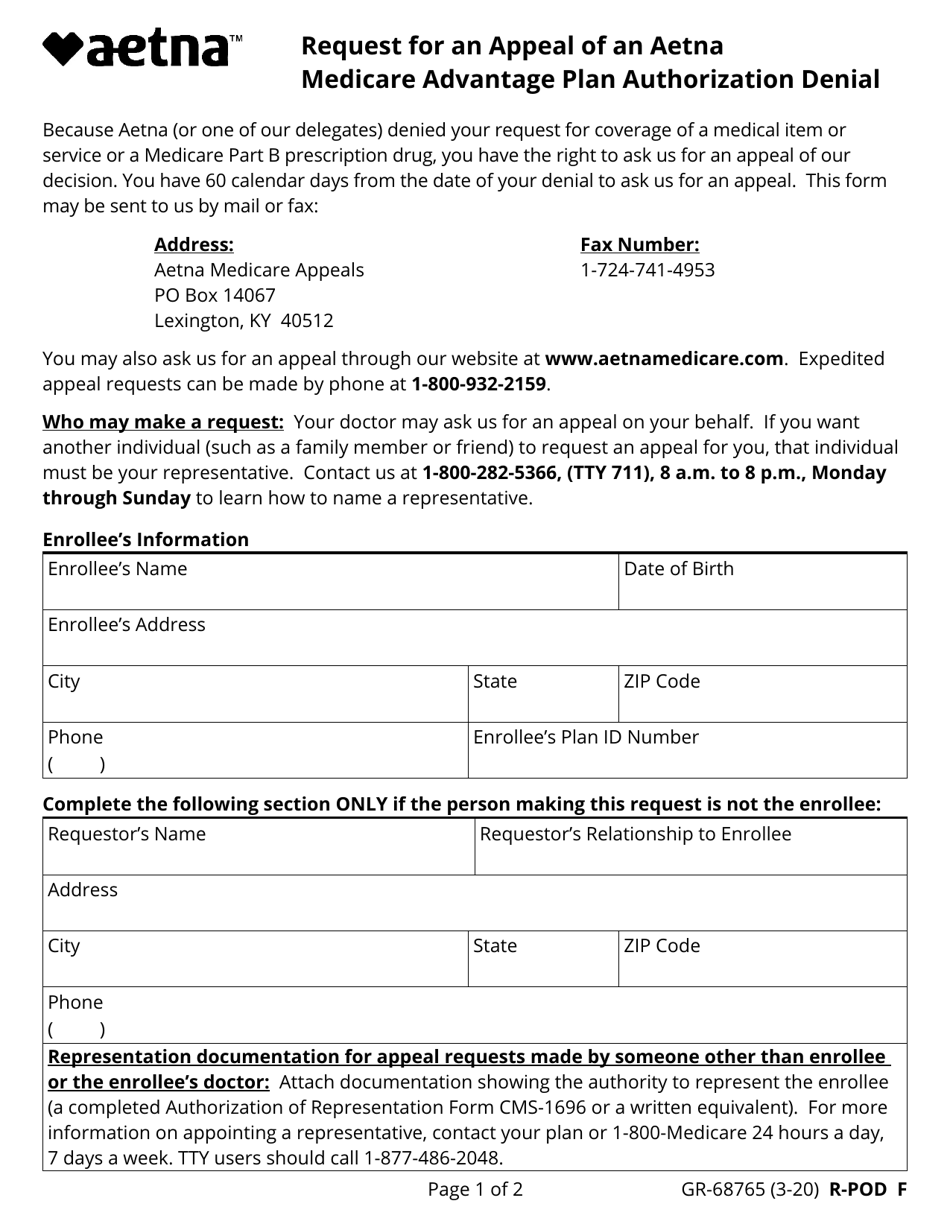
Form GR68765 Download Fillable PDF or Fill Online Request for an
Aetna Medicare Medication Prior Authorization Form Form Resume
Fill Free fillable Aetna Better Health PDF forms
TX AETNA GR69125 2015 Fill and Sign Printable Template Online US
Aetna blank prior authorization forms Fill out & sign online DocHub
Related Post: