Pacificsource Prior Authorization Form
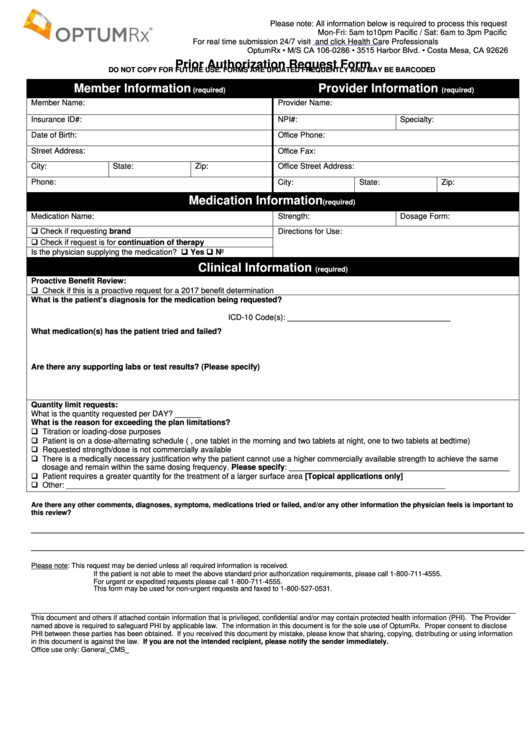
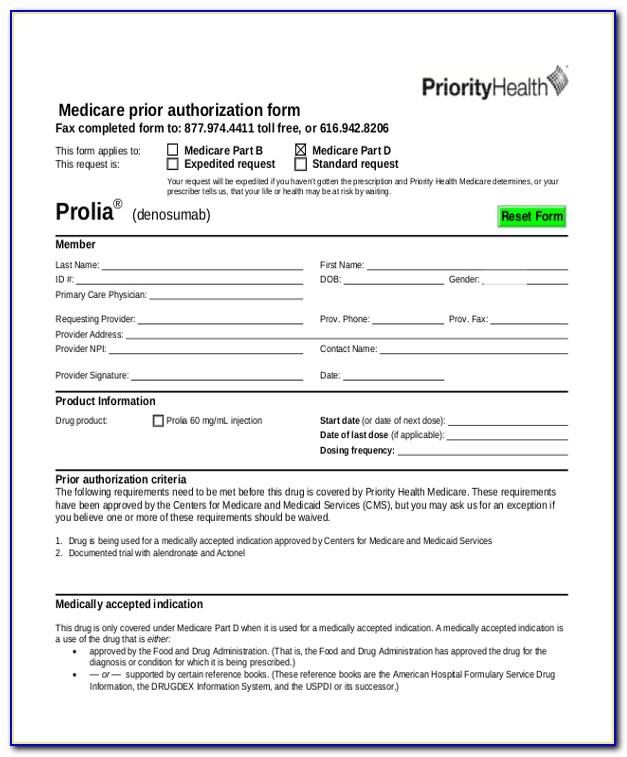
Pacificsource Prior Authorization Form - Web prior authorization requests may require supporting information. This login page requires that you have registered as a onehealthport subscriber. By checking this box and signing below, i certify that applying the. I’m not a onehealthport subscriber but would like. Web pacificsource community health plans is an hmo/ppo plan with a medicare contract. For questions about documents and forms specific to your plan and coverage, please contact customer service. For more information, please email. A determination notice will be mailed and/or faxed to the requesting provider, facility, and patient. Web prior authorization request form. Beyfortus prefilled syringe add tier 0. (cpt or hcpcs), or by name to learn whether prior. Web pharmacy prior authorization form; Whatever computer is, how it works. Web health services prior authorization request. With our updated provider authorization grid, you can search for a procedure by code. Web pharmacy prior authorization form; Determination notice will be mailed and/or faxed to the requesting provider, facility, and patient. Choose a line of business / group to begin your search. Web health services prior authorization request. Web pacificsource carefully observes hipaa privacy and consent guidelines when handling your data made available as part of hhs interoperability rules. Requests received after 3:00 p.m. Web pacificsource medicare responds to prior authorization requests within 14 calendar days. I’m not a onehealthport subscriber but would like. Service is typically faster through. Web pacificsource community health plans is an hmo/ppo plan with a medicare contract. What thereto is, how it works. Web learn nearly preauthorization and your pacificsource health plan. Web prior authorization request form. Web pacificsource supports a growing portfolio of health data interoperability resources to comply with federal regulations and enable the safe exchange of health data, which is. Web use this authorization grid search to find which codes require prior authorization from. Y0021_medm1844_plan approved 04222013 a determination notice will be mailed. This login page requires that you have registered as a onehealthport subscriber. Web pacificsource responds to preauthorization requests within two (2) working days. Web pacificsource medicare makes available prior authorization or exception request forms upon request to both enrollees and prescribing physicians via a variety of mechanisms,. For certain medical procedures,. Web health services prior authorization request. Web learn nearly preauthorization and your pacificsource health plan. Web pacificsource supports a growing portfolio of health data interoperability resources to comply with federal regulations and enable the safe exchange of health data, which is. All appeals must be received by the plan within 60. A determination notice will be mailed and/or faxed to. Web health services prior authorization request. For more information, please email. Incomplete requests will delay the prior authorization process. For questions about documents and forms specific to your plan and coverage, please contact customer service. Web pacificsource medicare responds to prior authorization requests within 14 calendar days. (cpt or hcpcs), or by name to learn whether prior. By checking this box and signing below, i certify that applying the. Web prior authorization request form. Web pacificsource carefully observes hipaa privacy and consent guidelines when handling your data made available as part of hhs interoperability rules. Please wait while we create your prior authorization criteria document. Web learn nearly preauthorization and your pacificsource health plan. Web pacificsource community health plans is an hmo/ppo plan with a medicare contract. What thereto is, how it works. Beyfortus prefilled syringe add tier 0. With our updated provider authorization grid, you can search for a procedure by code. Web prior authorization requests may require supporting information. Incomplete requests will delay the prior authorization process. Web pacificsource medicare responds to prior authorization requests within 14 calendar days. Web pacificsource carefully observes hipaa privacy and consent guidelines when handling your data made available as part of hhs interoperability rules. Requests received after 3:00 p.m. Medically appropriate expedited requests are processed in 24 hours. This login page requires that you have registered as a onehealthport subscriber. Web health services prior authorization request. Web use this authorization grid search to find which codes require prior authorization from pacificsource health plans. Web the following changes to the drug list are effective december 22, 2023: Web pacificsource medicare makes available prior authorization or exception request forms upon request to both enrollees and prescribing physicians via a variety of mechanisms,. Web developers wishing to access the pacificsource patient access api must register in advance to obtain an api key. For certain medical procedures, supplies, and drugs, pacificsource requires approval in advance—a process called prior authorization or preauthorization. Web learn about preauthorization and your pacificsource health plan. Web learn nearly preauthorization and your pacificsource health plan. A determination notice will be mailed and/or faxed to the requesting provider, facility, and patient. Web pacificsource community health plans is an hmo/ppo plan with a medicare contract. Choose a line of business / group to begin your search. For more information, please email. Web prior authorization requests may require supporting information. By checking this box and signing below, i certify that applying the. Web pharmacy prior authorization form; I’m not a onehealthport subscriber but would like. Incomplete requests will delay the prior authorization process. Network exception request one time.Prior Authorization Request Form printable pdf download
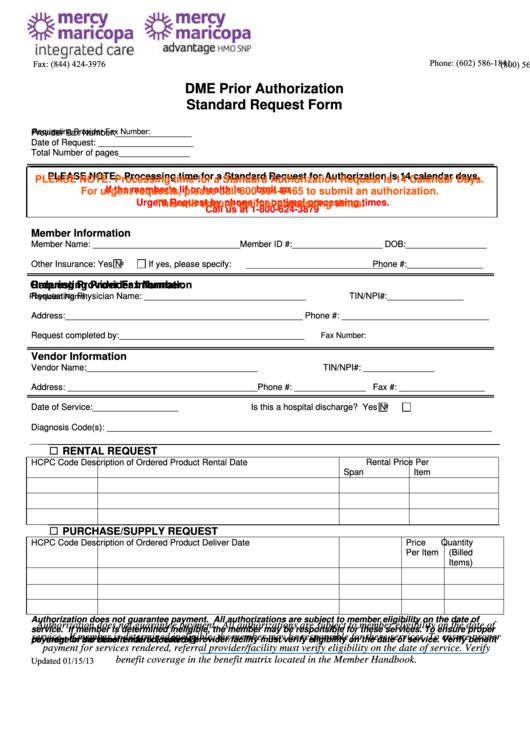
Fillable Dme Prior Authorization Standard Request Form printable pdf
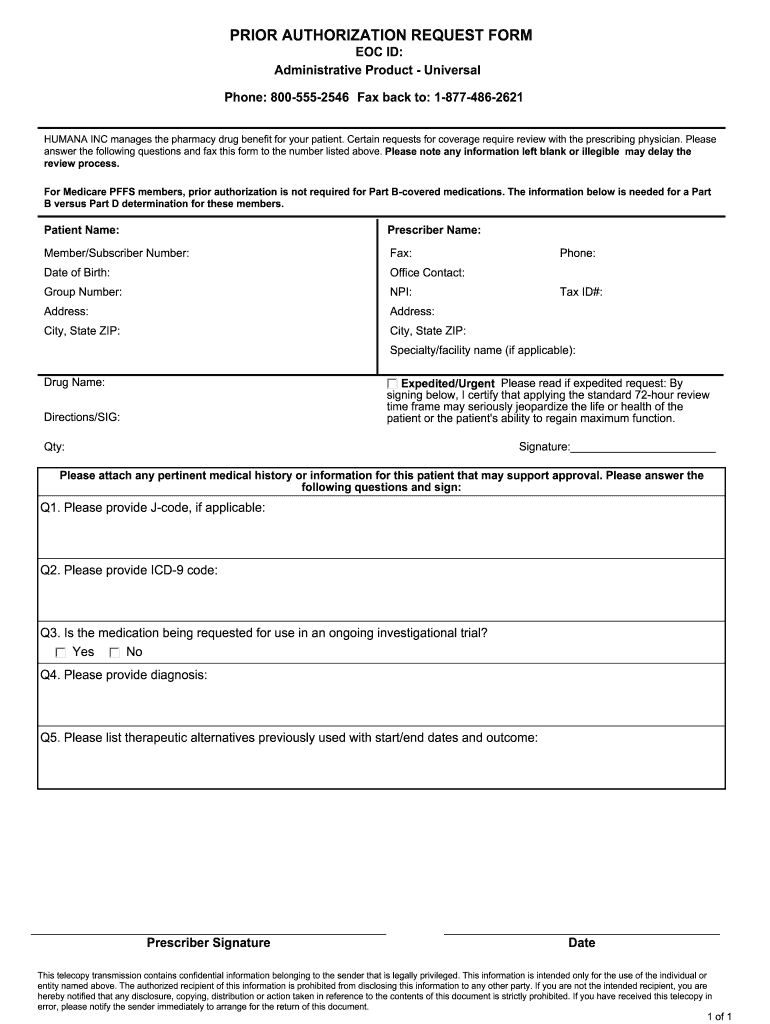
Humana Prior Authorization Form Fill Out and Sign Printable PDF
Free Prior (Rx) Authorization Forms PDF eForms
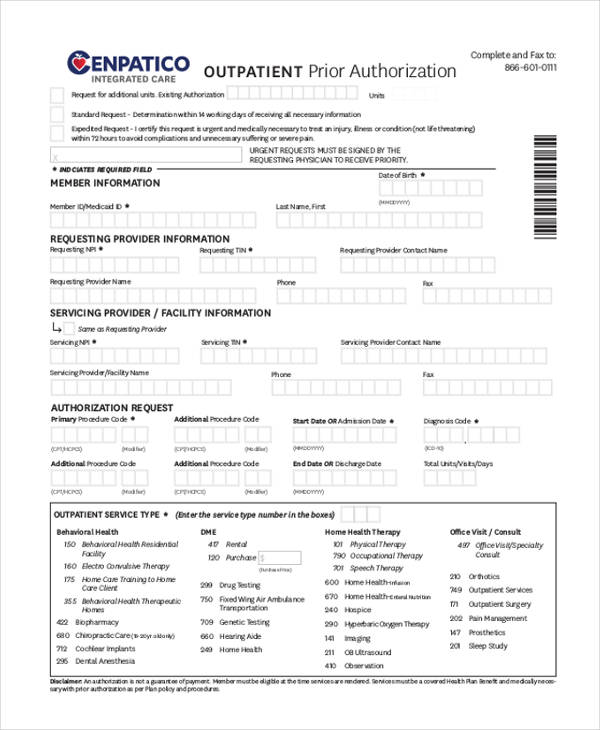
FREE 11+ Prior Authorization Forms in PDF MS Word
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
FREE 13+ Prior Authorization Forms in PDF MS Word
Medco Prior Auth Form Medication Form Resume Examples q25Z4Lxk0o
Prior Authorization Form Fill Out and Sign Printable PDF Template
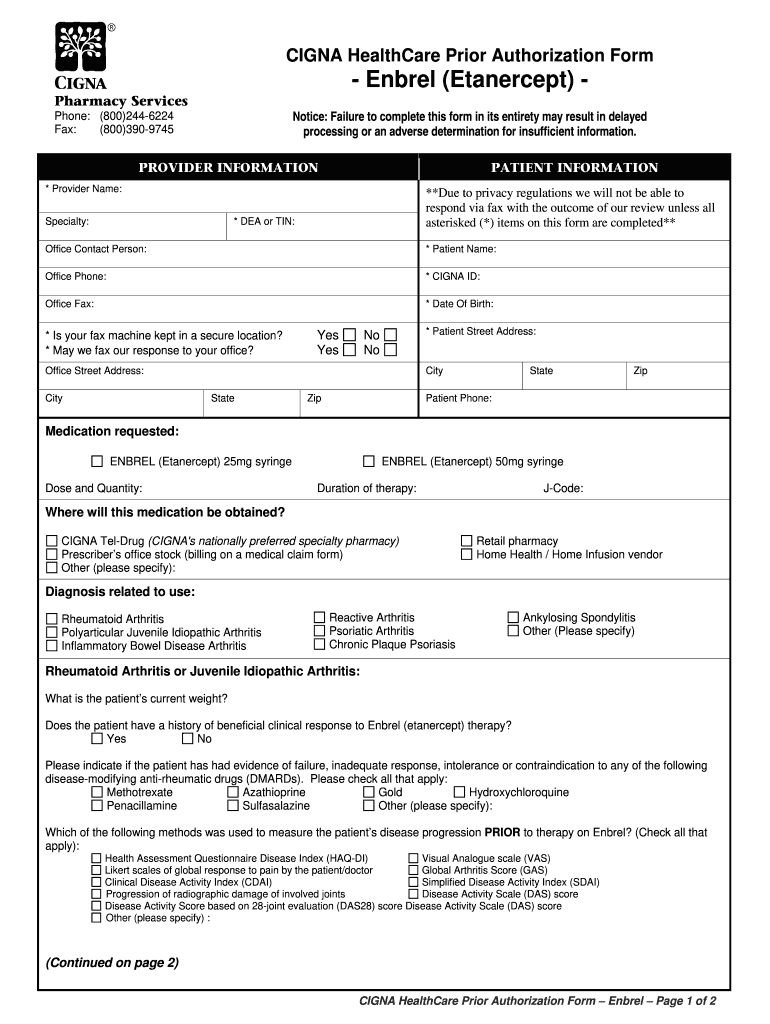
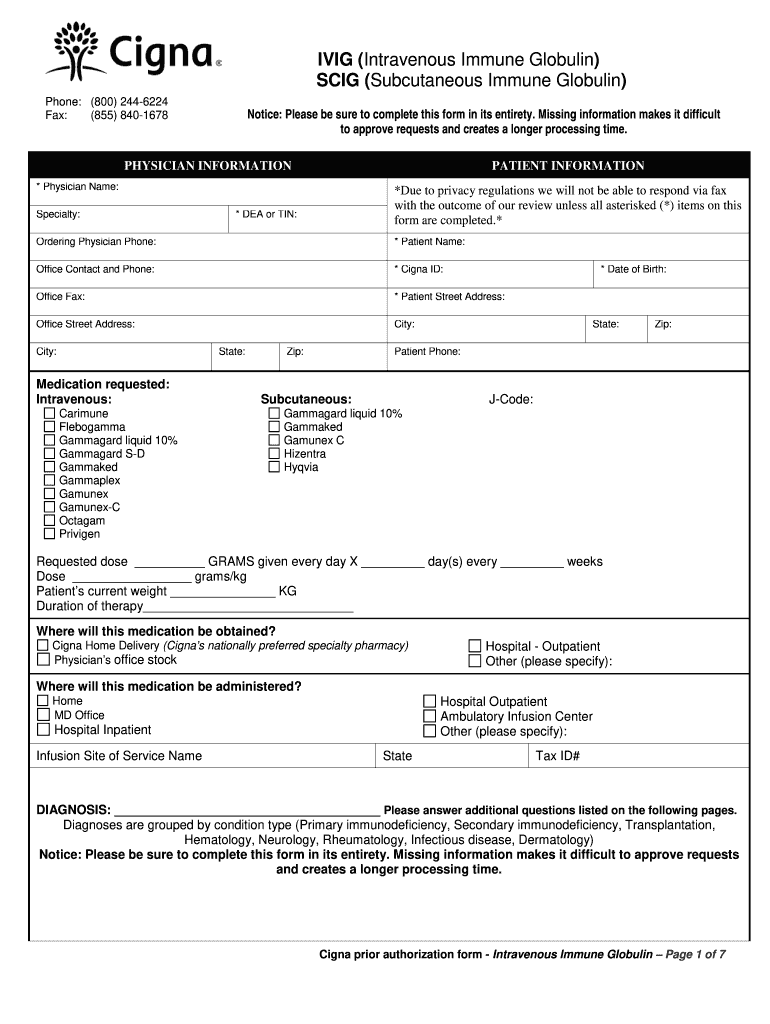
2016 Cigna IVIGSCIG PSP Prior Authorization FormFill Online, Printable
Related Post: