Molina Appeals Form
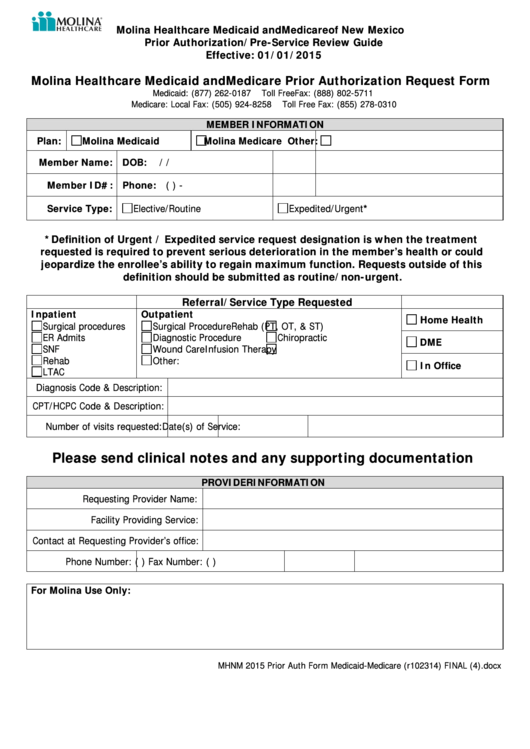
Molina Appeals Form - Web if molina medicare or one of our plan providers reduces or cuts back on services or benefits you have been receiving, you can file an appeal. You can provide it to us in person or in writing to: Web the authorization appeal should be submitted on the authorization reconsideration form (authorization appeal and clinical claim dispute request form) and submitted. Web all claim appeals and disputes should be submitted on the molina provider appeal/dispute form found on our website, www.molinahealthcare.com under forms. Web by submitting my information via this form, i consent to having molina healthcare collect my personal information. Appeals & grievances department or by mail to molina. Web authorization reconsideration form (authorization appeal or clinical claim dispute form) grievance/appeal request form. Web molina complete care. Web responsible for the comprehensive research and resolution of the appeals, dispute, grievances, and/or complaints from molina members, providers and related. Please include a copy of the eob with the appeal and any supporting. An appeal is a request to review an action or denial. Web provider appeals the molina healthcare of michigan appeals team coordinates clinical review for provider appeals with molina healthcare medical. Web wisconsin provider appeal form line of business: • you have a total of 60 calendar days from the date of this notice to ask for a plan appeal.. Did you know a pa denial reconsideration is. Please include a copy of the eob with the appeal and any supporting. Web wisconsin provider appeal form line of business: Web this form can be used for up to 9 claims that have the same denial reason. Web all claim appeals and disputes should be submitted on the molina provider appeal/dispute. 5055 e washington st, suite 210. Web if molina medicare or one of our plan providers reduces or cuts back on services or benefits you have been receiving, you can file an appeal. You can provide it to us in person or in writing to: Web by submitting my information via this form, i consent to having molina healthcare collect. To send us an appeal in writing, mail the document to: Web the last day to ask for a plan appeal to keep your services the same is [ ]. Web authorization reconsideration form (authorization appeal or clinical claim dispute form) grievance/appeal request form. Web if molina medicare or one of our plan providers reduces or cuts back on services. Web provider claim appeal and dispute form. Web all claim appeals and disputes should be submitted on the molina provider appeal/dispute form found on our website, www.molinahealthcare.com under forms. An appeal is a request to review an action or denial. Web the last day to ask for a plan appeal to keep your services the same is [ ]. Web. 5055 e washington st, suite 210. Web below is a form to assist you in making your appeal request in writing. Web the authorization appeal should be submitted on the authorization reconsideration form (authorization appeal and clinical claim dispute request form) and submitted. Did you know a pa denial reconsideration is. An appeal is a request to review an action. An appeal is a request to review an action or denial. Web below is a form to assist you in making your appeal request in writing. Molina healthcare’s grievance and appeal procedure is overseen by our grievance and appeal unit.its purpose is to resolve issues and. Web molina complete care. Web provider claim appeal and dispute form. Web authorization reconsideration form (authorization appeal or clinical claim dispute form) grievance/appeal request form. Web molina complete care. Did you know a pa denial reconsideration is. Deaf or hard of hearing members may call. Molina healthcare’s grievance and appeal procedure is overseen by our grievance and appeal unit.its purpose is to resolve issues and. Web the last day to ask for a plan appeal to keep your services the same is [ ]. Deaf or hard of hearing members may call. Web molina complete care. If you receive a denial letter and do not like the choice we made, you can file an appeal. Web provider claim appeal and dispute form. Web responsible for the comprehensive research and resolution of the appeals, dispute, grievances, and/or complaints from molina members, providers and related. If you receive a denial letter and do not like the choice we made, you can file an appeal. • you have a total of 60 calendar days from the date of this notice to ask for a plan. Molina healthcare’s grievance and appeal procedure is overseen by our grievance and appeal unit.its purpose is to resolve issues and. Web the last day to ask for a plan appeal to keep your services the same is [ ]. Web this form can be used for up to 9 claims that have the same denial reason. If you think we are. Please include a copy of the eob with the appeal and any supporting. Web by submitting my information via this form, i consent to having molina healthcare collect my personal information. Web molina complete care. Web below is a form to assist you in making your appeal request in writing. Web authorization reconsideration form (authorization appeal or clinical claim dispute form) grievance/appeal request form. If you have 10 or more claims, please email. Web provider appeals the molina healthcare of michigan appeals team coordinates clinical review for provider appeals with molina healthcare medical. Web the authorization appeal should be submitted on the authorization reconsideration form (authorization appeal and clinical claim dispute request form) and submitted. If you receive a denial letter and do not like the choice we made, you can file an appeal. • you have a total of 60 calendar days from the date of this notice to ask for a plan appeal. To send us an appeal in writing, mail the document to: Web provider claim appeal and dispute form. An appeal is a request to review an action or denial. Web claim reconsideration request form. Web filed 10/17/23 certified for publication in the court of appeal of the state of california fourth appellate district division three the. Web responsible for the comprehensive research and resolution of the appeals, dispute, grievances, and/or complaints from molina members, providers and related.Molina Healthcare Medicaid And Medicare Prior Authorization Request
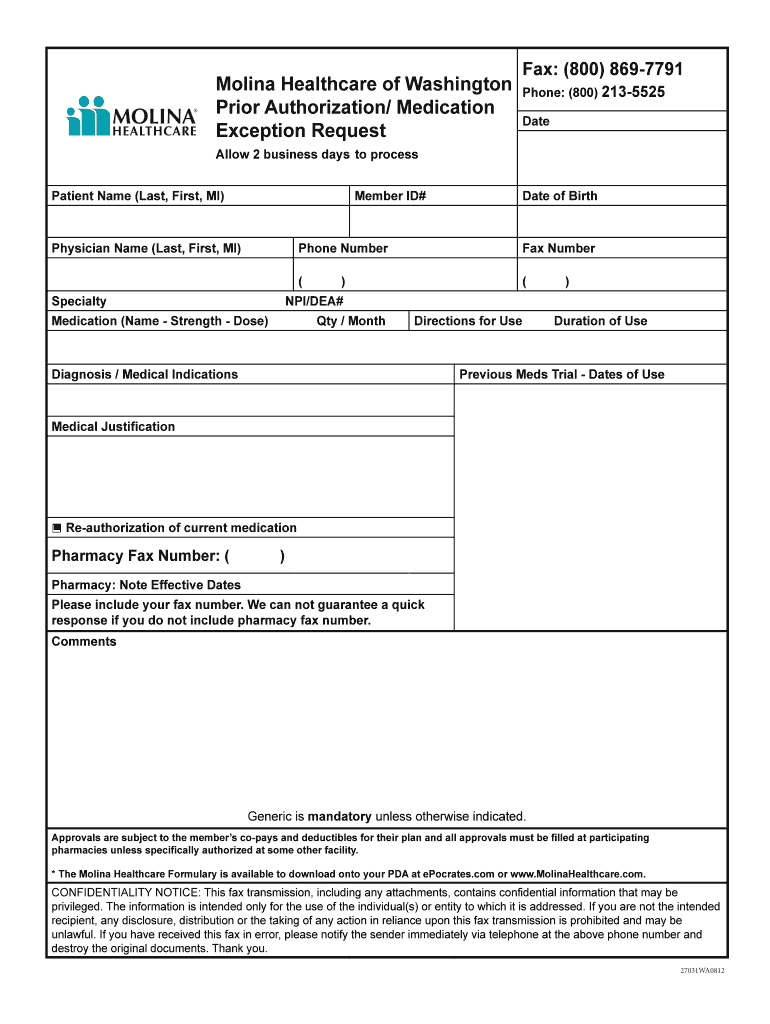
UT Molina Healthcare Prior Authorization Form 20162022 Fill and Sign
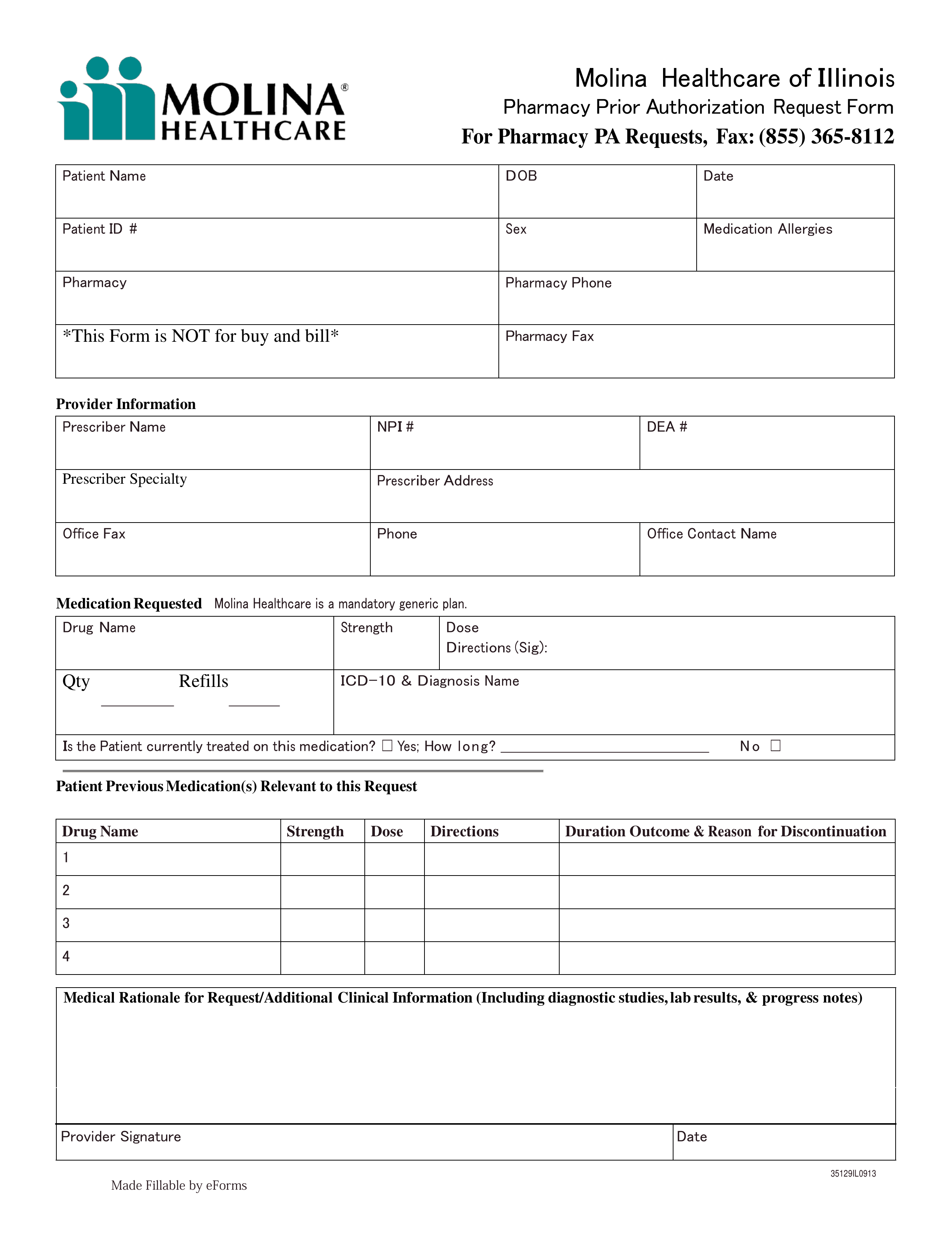
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
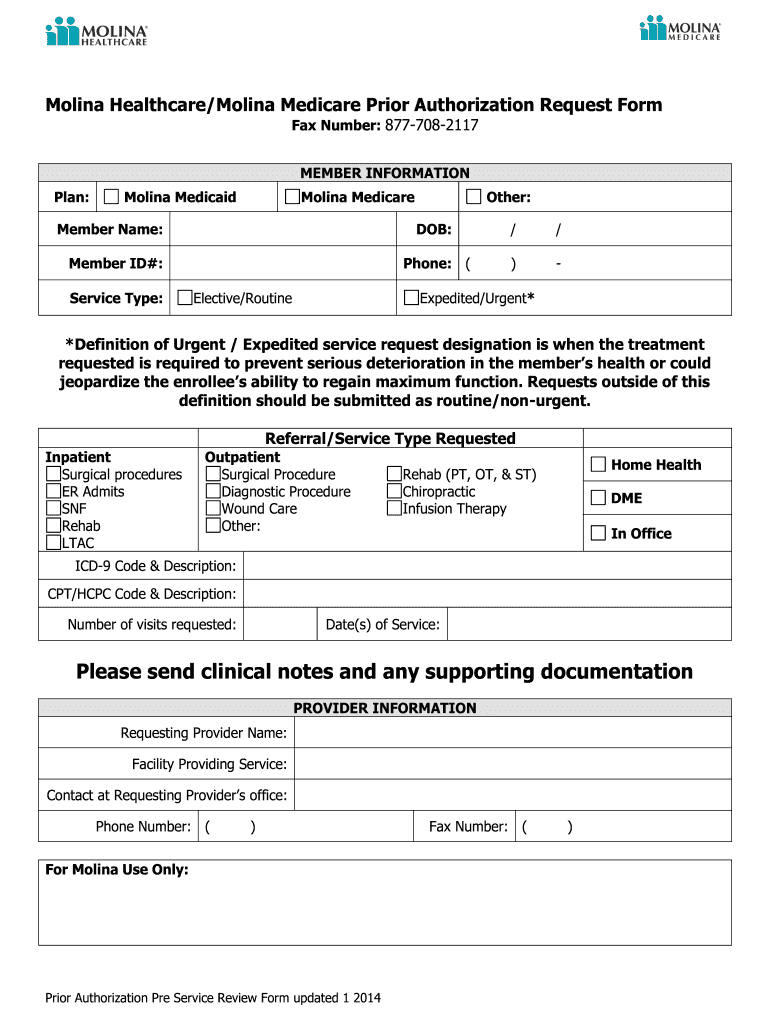
Medicare authorization pre form Fill out & sign online DocHub
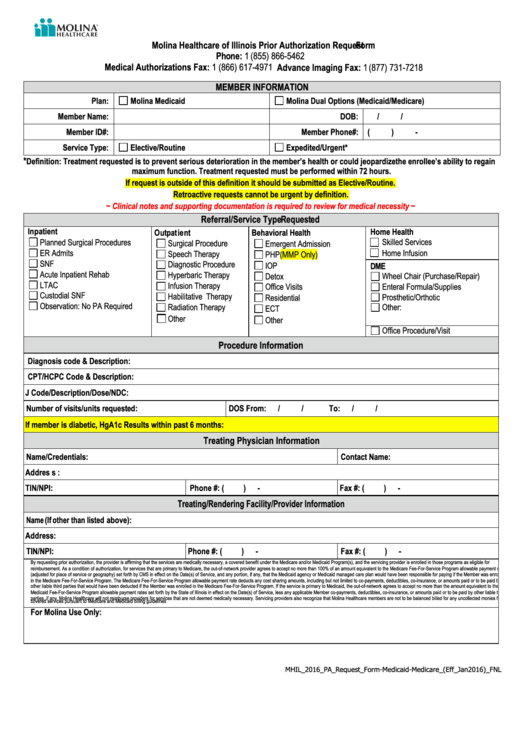
Molina Healthcare Of Illinois Prior Authorization Request printable pdf
Molina Authorization Form Fill Online, Printable, Fillable, Blank
WA Molina Healthcare Behavioral Health Authorization/Notification Form
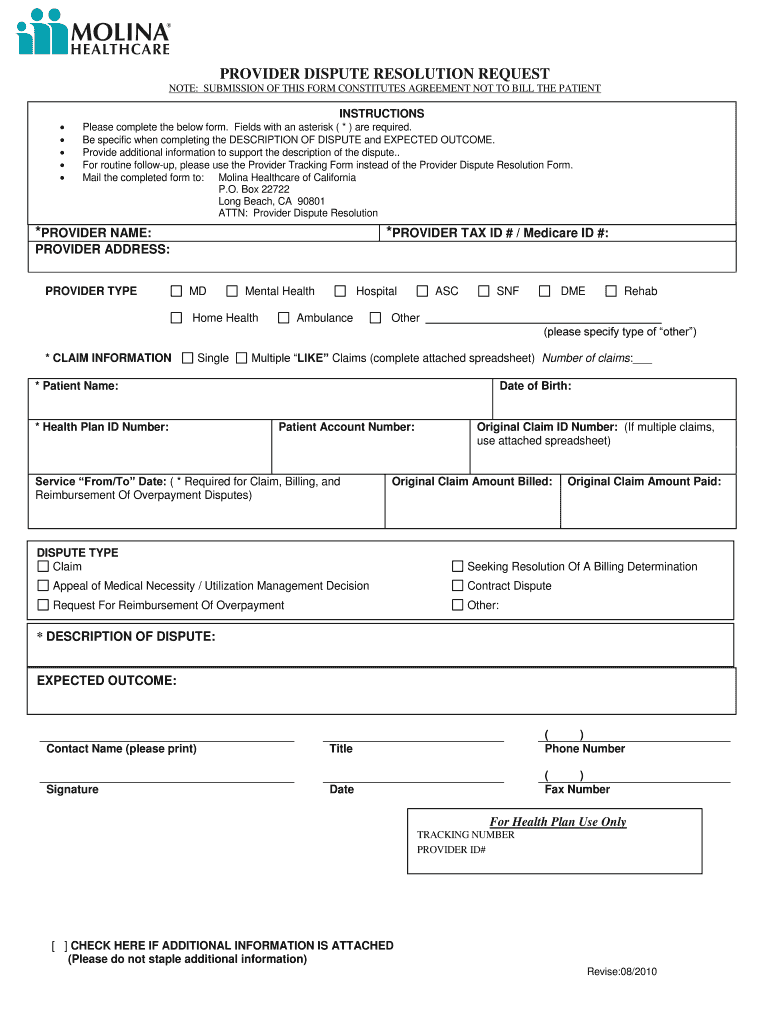
Molina provider dispute resolution form Fill out & sign online DocHub
Molina Appeal Form Washington Fill Online, Printable, Fillable, Blank
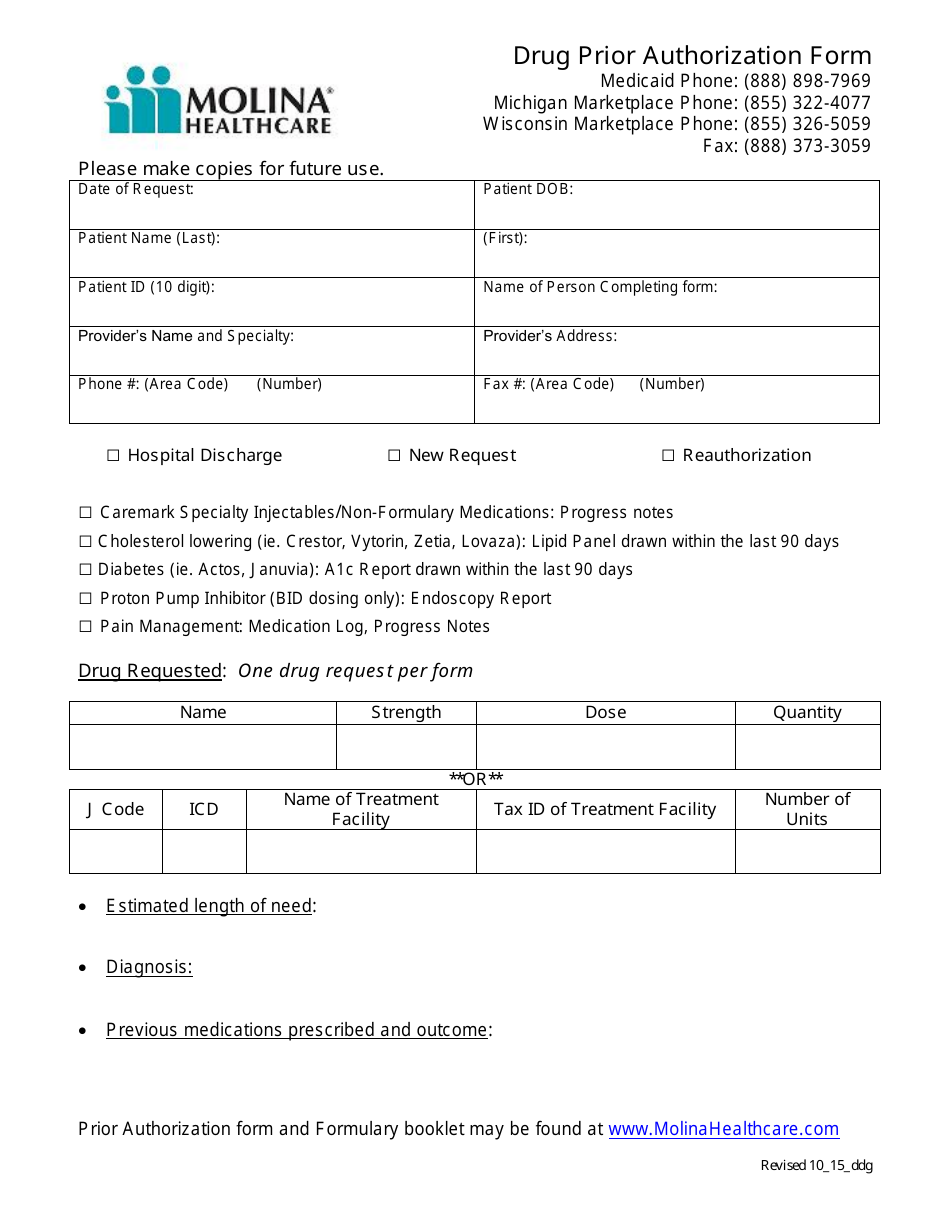
Drug Prior Authorization Form Molina Healthcare Fill Out, Sign
Related Post: