Molina Appeal Form Ohio
Molina Appeal Form Ohio - Complete this form and mail or fax to: You, or someone you want to speak for you can contact the mce using this form. Web ohio medicaid managed care entity. Instructions for filing a grievance/appeal: Forms will be returned to the submitter. To 7 p.m., local time fax number: Web molina healthcare member grievance/appeal request form. Log in with your user id and password. Claim reconsideration request form requirements. When submitting via the provider portal, this action must be completed via the “appeal claim” feature. To file an appeal if molina healthcare denies, reduces or suspends your service or claim. Molina healthcare of ohio, attn: Web if a provider or someone else submits an appeal on your behalf, we must receive your written consent before we can begin processing your appeal. How to appeal a denial of services. | molina healthcare of ohio. Attach copies of any records you wish to submit. Web you may contact molina for assistance with filing your complaint over the phone, by mail or fax using the following contact information. You, or someone you want to speak for you can contact the mce using this form. Molina healthcare of ohio, attn: Complete this form and mail or fax. Describe the issue(s) in as much detail as possible. Web molina healthcare of ohio, inc. Fill out this form completely. Web claim and authorization reconsideration training. Molina healthcare of ohio, inc. Providers can access the most current provider manual at. • incomplete forms will not be processed. Web member appeal form if you do not agree with a decision made by your managed care entity (mce), you should contact the mce as soon as possible. Web you may contact molina for assistance with filing your complaint over the phone, by mail. • incomplete forms will not be processed. Mail letters or forms to: Web if molina medicare or one of our plan providers reduces or cuts back on services or benefits you have been receiving, you can file an appeal. Web if a provider or someone else submits an appeal on your behalf, we must receive your written consent before we. Web ohio provider contract request form *. Behavioral health respite services pa reference guide. You may write and sign a letter or complete the grievance/appeal form and send it to us. This form and send it back to molina healthcare. | molina healthcare of ohio. Molina healthcare of ohio, inc. Web ohio medicaid managed care entity. Log in with your user id and password. Forms will be returned to the submitter. Describe the issue(s) in as much detail as possible. Molina healthcare of ohio, inc. Mail letters or forms to: Web • the authorization reconsideration form (authorization appeal and clinical claim dispute form) filled out entirely with the following details (failure to do so will prevent the form from being processed, and the provider will be notified): Instructions for filing a grievance/appeal: Web molina healthcare member grievance/appeal request form. If you think we are stopping your coverage of a service or benefit too soon, you can file an appeal. Web molina healthcare member grievance/appeal request form. Complete this form and mail or fax to: Molina healthcare of ohio, inc. Send the completed form to one of the following: To file an appeal if molina healthcare denies, reduces or suspends your service or claim. Molina healthcare prior authorization request form and instructions. Fill out this form completely. If you do not agree with a decision made by your managed care entity (mce), you should contact the mce as soon as possible. Molina healthcare of ohio, inc. Web molina healthcare prior authorization request form and instructions. Serve as my representative throughout the appeal process. How to file a grievance. To file an appeal if molina healthcare denies, reduces or suspends your service or claim. 1, 2019, claim disputes or authorization reconsiderations submitted on an incorrect form, or submitted on a form that is not filled out completely,. Molina healthcare of ohio, inc. Instructions for provider portal submissions (if a claim has been filed): Web the advance beneficiary notice of noncoverage (abn) form should not be issued to molina members within the medicare and mycare ohio population of molina. Complete this form and mail or fax to: Molina healthcare prior authorization request form and instructions. Web ohio provider contract request form *. Send the completed form to one of the following: Web member appeal form if you do not agree with a decision made by your managed care entity (mce), you should contact the mce as soon as possible. Web • the authorization reconsideration form (authorization appeal and clinical claim dispute form) filled out entirely with the following details (failure to do so will prevent the form from being processed, and the provider will be notified): Forms will be returned to the submitter. Web you may contact molina for assistance with filing your complaint over the phone, by mail or fax using the following contact information. Attach copies of any records you wish to submit. We cannot process your appeal. Providers can access the most current provider manual at. Please send corrected claims as normal claim submissions via electronic or paper.Ohio Appeals Notice Form Fill Online, Printable, Fillable, Blank
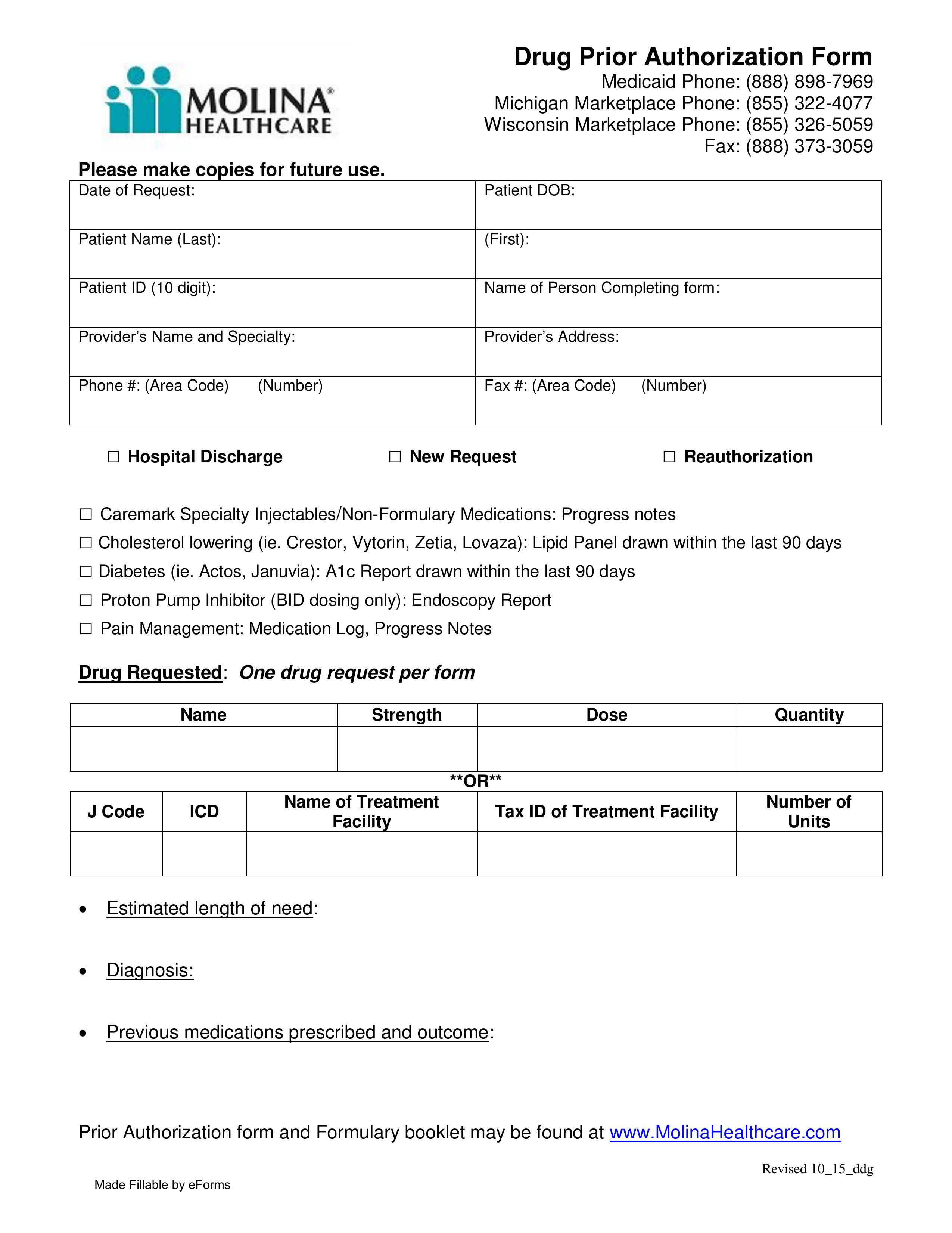
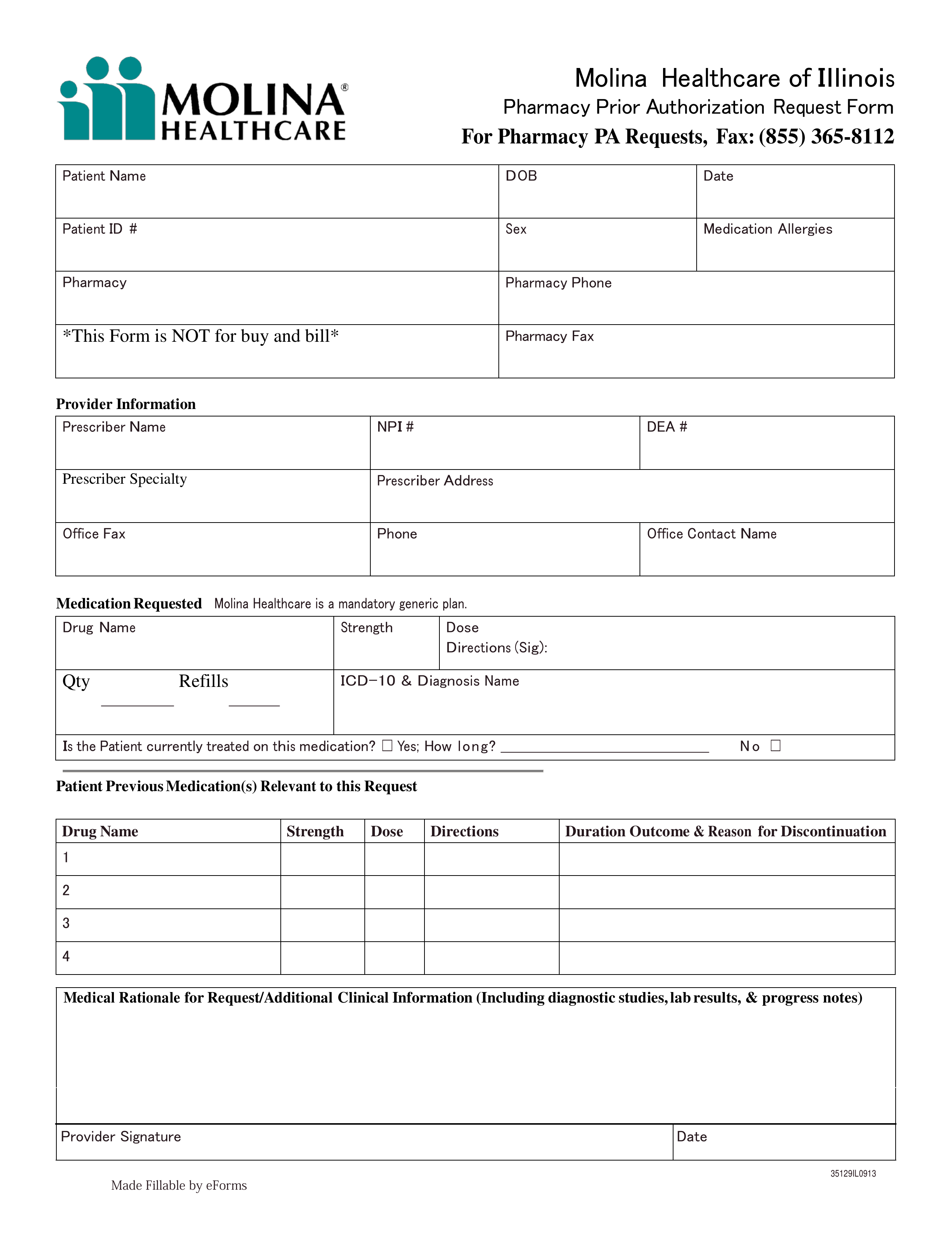
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
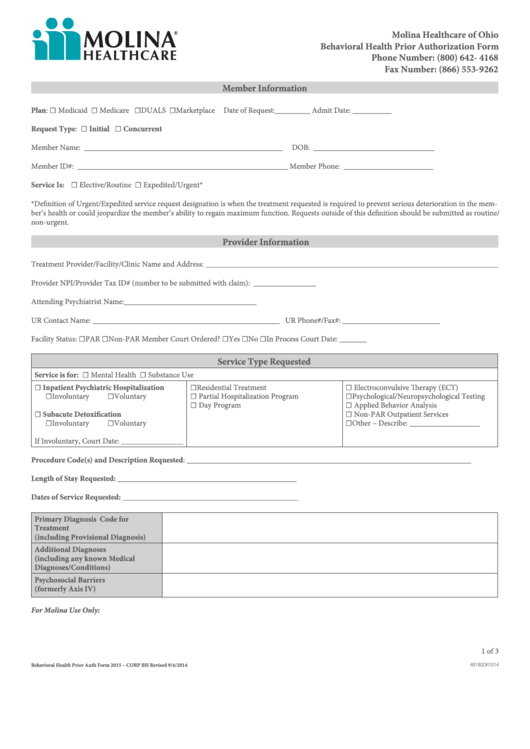
Fillable Molina Behavioral Health Prior Authorization Form Ohio
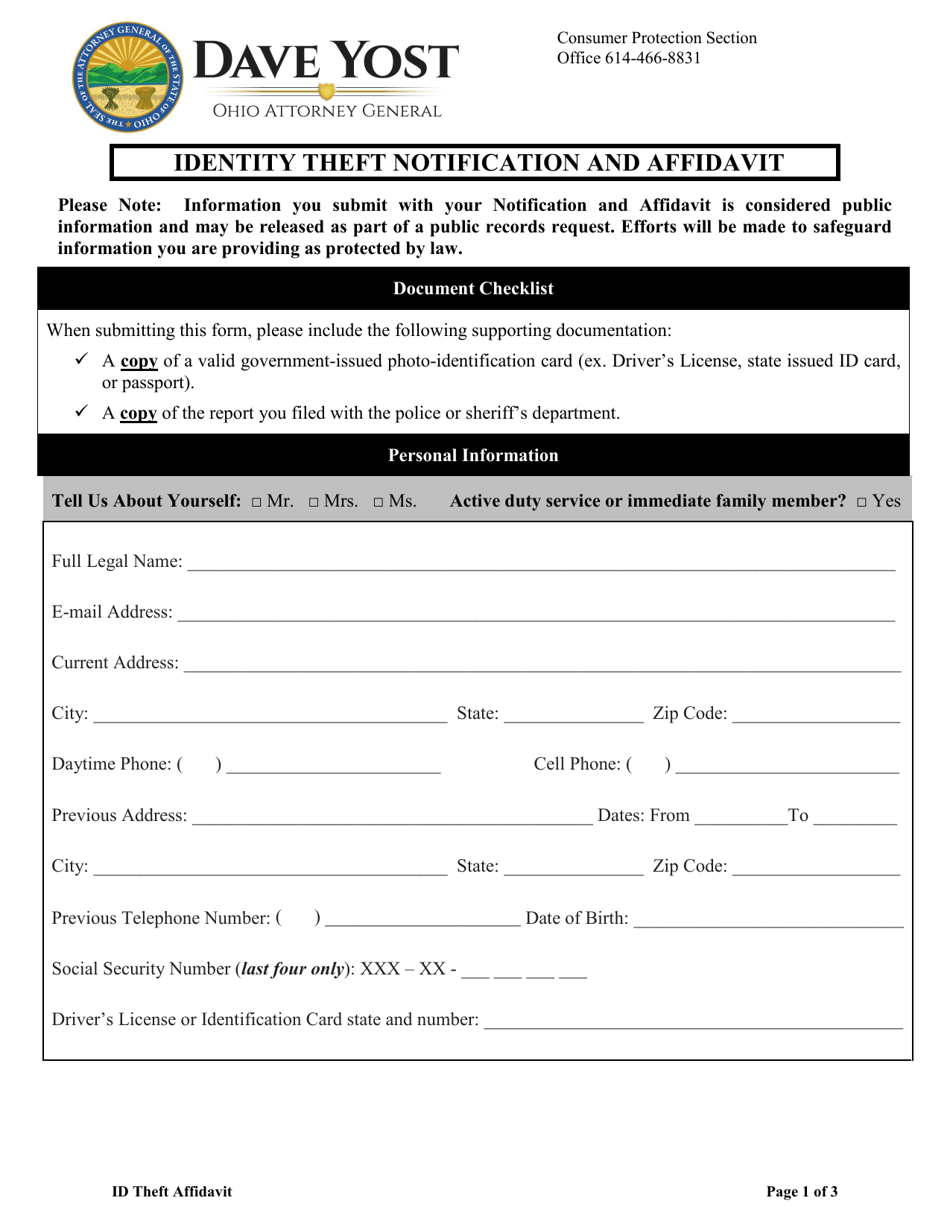
Ohio Affidavit Form Fill Out And Sign Printable Pdf Template 1DF
IN THE COURT Ohio Twelfth District Court Of Appeals Fill and Sign
Molina Drug Prior Authorization Fill Online, Printable, Fillable
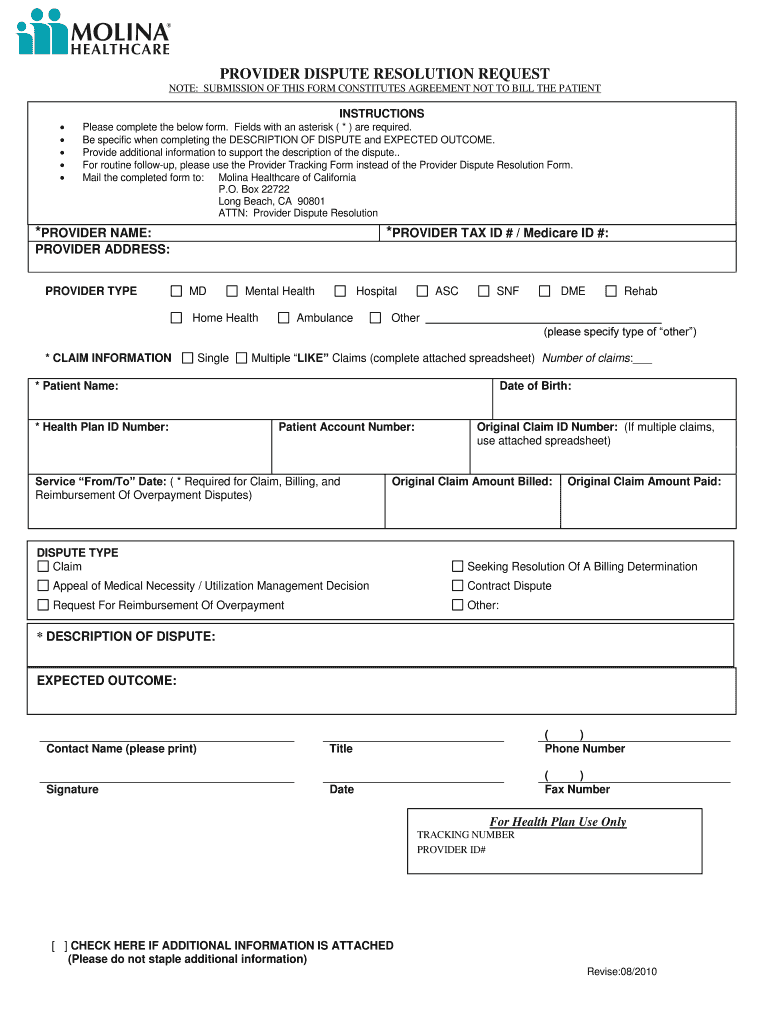
Molina provider dispute resolution form Fill out & sign online DocHub
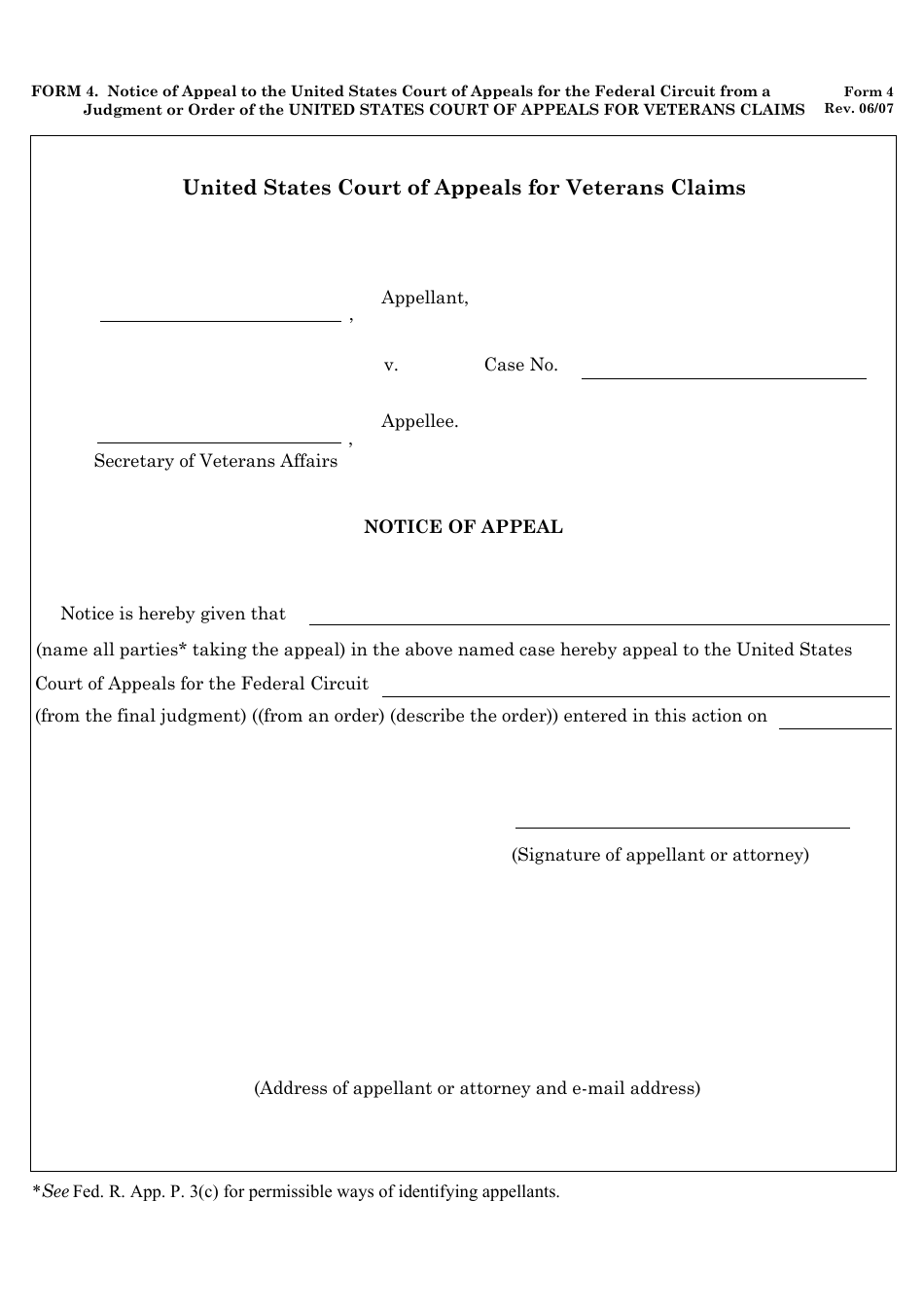
Form 4 Fill Out, Sign Online and Download Fillable PDF Templateroller
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
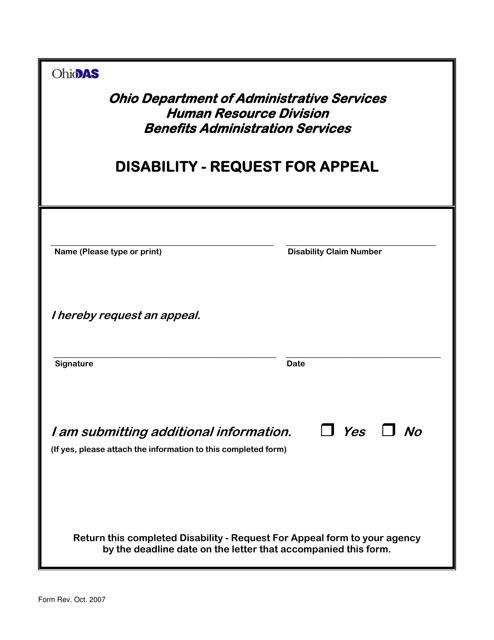
Ohio Disability Request for Appeal Fill Out, Sign Online and
Related Post: