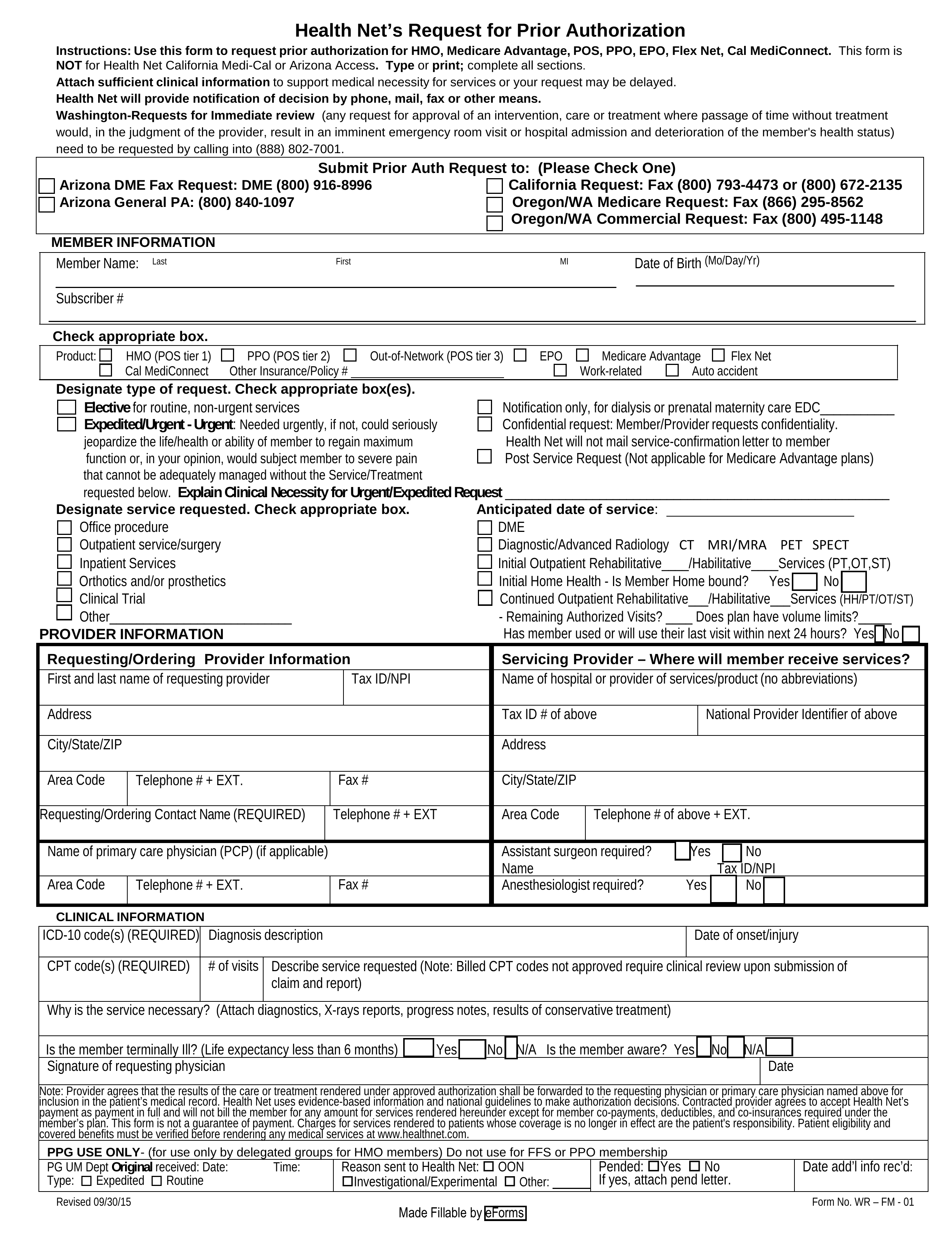
Healthnet Prior Authorization Form
Healthnet Prior Authorization Form - Wellcare by health net medicare advantage (ma) ppo and hmo direct network1. Web you, your representative, or your network primary care provider (pcp), or the provider that furnishes or intends to furnish the services to you, may request a prior. Web health net’s request for prior authorization instructions: In the secure portal, click on submit authorization request to access careaffiliate. Determination within 5 business days. Web health net’s request for prior authorization. Ad net health isn't just an ehr software, it's specialized to the needs of your care setting. Health net providers can view and download files including prior authorization forms, hospice forms, covered dme and more. This means that members must receive approval from health net before a drug will be covered. To initiate the prior authorization process, pcps and specialists must: Web some drugs require prior authorization. This form is not for. Find information about health net's criteria regarding prior drug authorizations, step therapy and drug quantity limits. Web provider.healthnet.com > working with health net > services requiring prior authorization. Web health net request for prior authorization form must be completed in its entirety and include sufficient clinical information or notes. Web health net request for prior authorization form must be completed in its entirety and include sufficient clinical information or notes to support medical necessity for services. Go beyond generic softwares to truly improve outcomes for your care setting's unique needs Wellcare by health net medicare advantage (ma) ppo and hmo direct network1. Verify member eligibility and beneit coverage. Web. Use this form to request prior authorization for hmo, medicare advantage, pos, ppo, epo, flex net, cal. Web initial approval is for 6 months, renewal of prior authorization may be given for up to 12 months following documentation of the following: To initiate the prior authorization process, pcps and specialists must: This means that members must receive approval from health. Web submit your request online. Go beyond generic softwares to truly improve outcomes for your care setting's unique needs Web you, your representative, or your network primary care provider (pcp), or the provider that furnishes or intends to furnish the services to you, may request a prior. Health net is contracted with medicare for hmo, hmo snp and ppo plans,. Wellcare by health net medicare advantage (ma) ppo and hmo direct network1. Web health net access prior authorization request available in the forms section on the health net access provider website at www.healthnetaccess.com behavioral health. Web health net’s request for prior authorization form. Ad net health isn't just an ehr software, it's specialized to the needs of your care setting.. Find information about health net's criteria regarding prior drug authorizations, step therapy and drug quantity limits. Web some drugs require prior authorization. Verify member eligibility and beneit coverage. In the secure portal, click on submit authorization request to access careaffiliate. Ad net health isn't just an ehr software, it's specialized to the needs of your care setting. O documentation of therapy meeting. Web a health net prior authorization form is a document that medical offices will use when requesting coverage of a patient's prescription. This means that members must receive approval from health net before a drug will be covered. In the secure portal, click on submit authorization request to access careaffiliate. Web health net’s request for. Use this form to request prior authorization for hmo, medicare advantage, pos, ppo, epo, flex net, cal. Form must be fully completed to avoid a processing delay. Web initial approval is for 6 months, renewal of prior authorization may be given for up to 12 months following documentation of the following: Web provider.healthnet.com > working with health net > services. Use this form to request prior authorization for employer group medicare advantage (ma) hmo, hmo, ppo,. O documentation of therapy meeting. Health net is contracted with medicare for hmo, hmo snp and ppo plans, and with some. Find information about health net's criteria regarding prior drug authorizations, step therapy and drug quantity limits. Web health net request for prior authorization. Web medicare prior authorization / formulary exception request fax form. Use this form to request prior authorization for employer group medicare advantage (ma) hmo, hmo, ppo,. Ad net health isn't just an ehr software, it's specialized to the needs of your care setting. Verify member eligibility and beneit coverage. Web this disclosure form (including any applicable disclosure form rider) and. Web health net’s request for prior authorization form. In the secure portal, click on submit authorization request to access careaffiliate. View health net prior authorization requirements per plan that may apply to a particular procedure, medication, service or supply. Use this form to request prior authorization for employer group medicare advantage (ma) hmo, hmo, ppo,. Web health net access prior authorization request available in the forms section on the health net access provider website at www.healthnetaccess.com behavioral health. Web submit your request online. Complete the prior authorization form (link provided. Web this disclosure form (including any applicable disclosure form rider) and the summary of benefits and coverage (sbc) document provide a summary of your health plan.the. Web health net’s request for prior authorization. Use this form to request prior authorization for hmo, medicare advantage, pos, ppo, epo, flex net, cal. Ad net health isn't just an ehr software, it's specialized to the needs of your care setting. Web you, your representative, or your network primary care provider (pcp), or the provider that furnishes or intends to furnish the services to you, may request a prior. Web health net’s request for prior authorization instructions: Go beyond generic softwares to truly improve outcomes for your care setting's unique needs Determination within 5 business days. Health net providers can view and download files including prior authorization forms, hospice forms, covered dme and more. Web some drugs require prior authorization. Verify member eligibility and beneit coverage. Wellcare by health net medicare advantage (ma) ppo and hmo direct network1. Web provider.healthnet.com > working with health net > services requiring prior authorization.Banner Health Prior Authorization Form 20202021 Fill and Sign
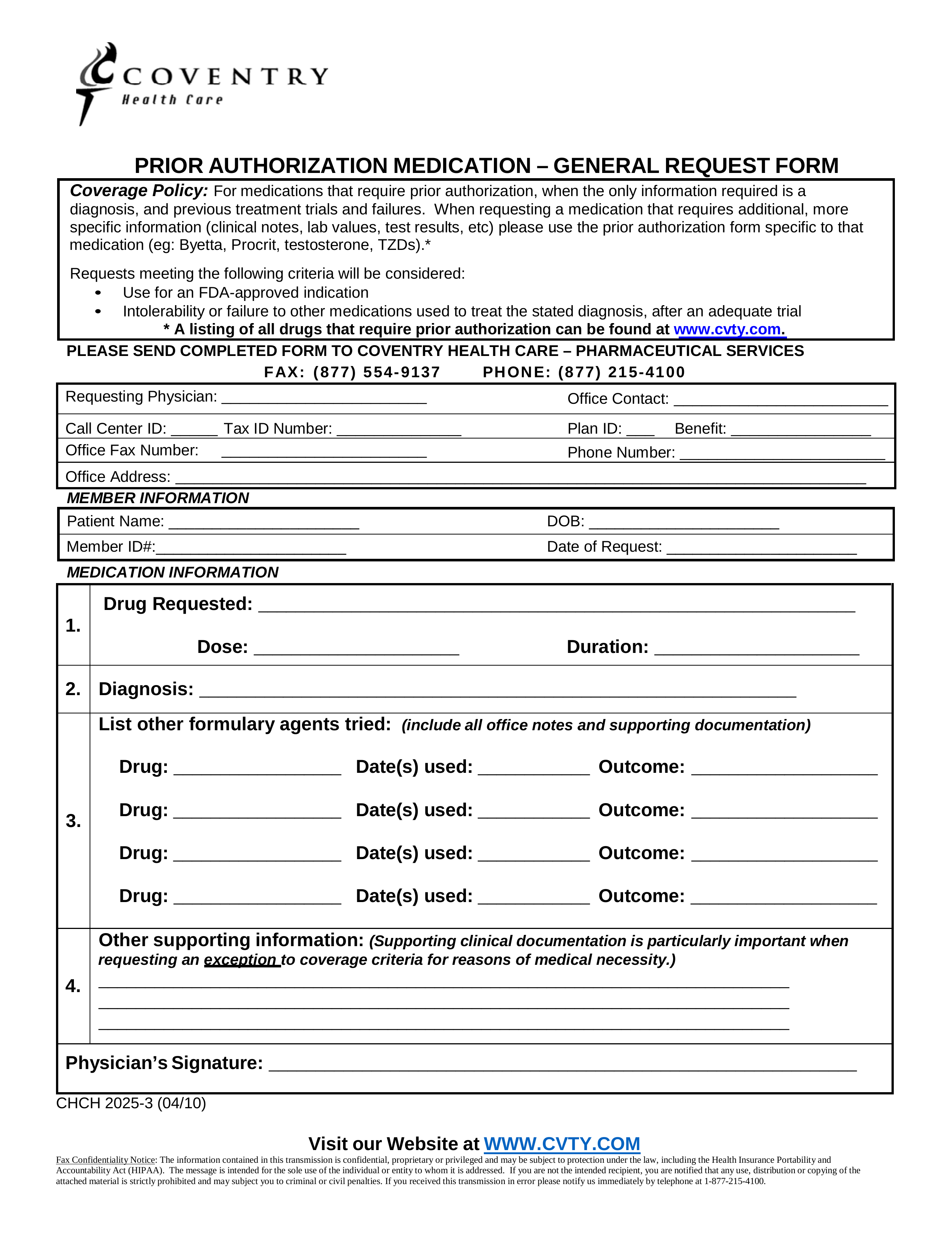
Free Coventry Health Care Prior (Rx) Authorization Form PDF eForms
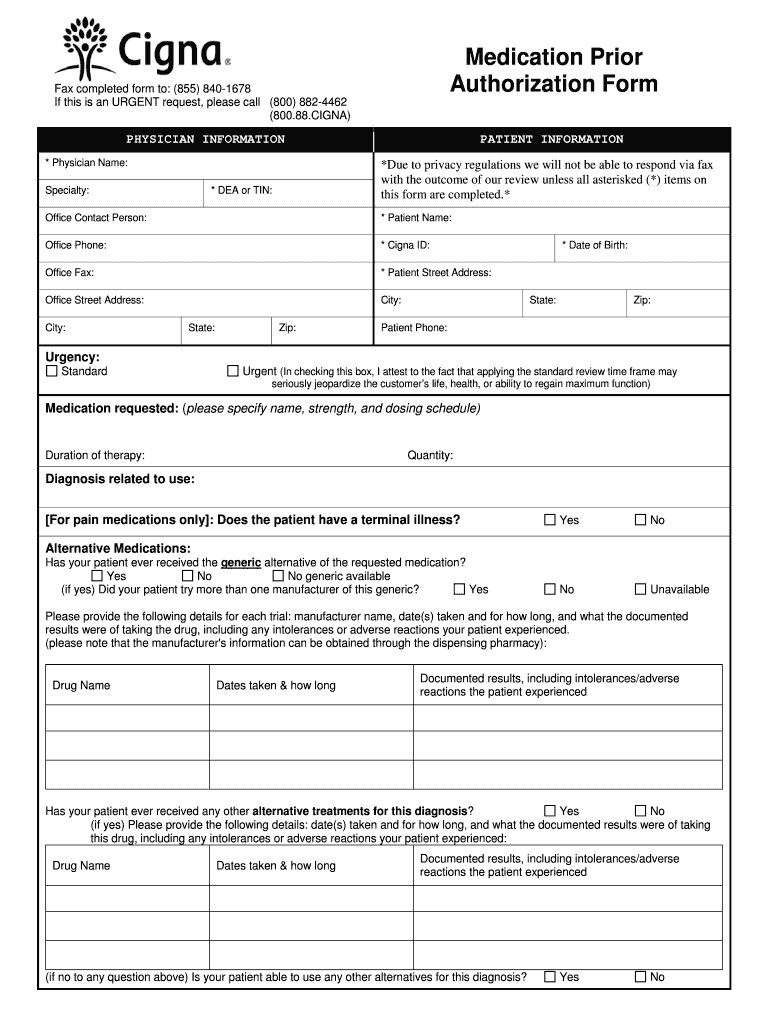
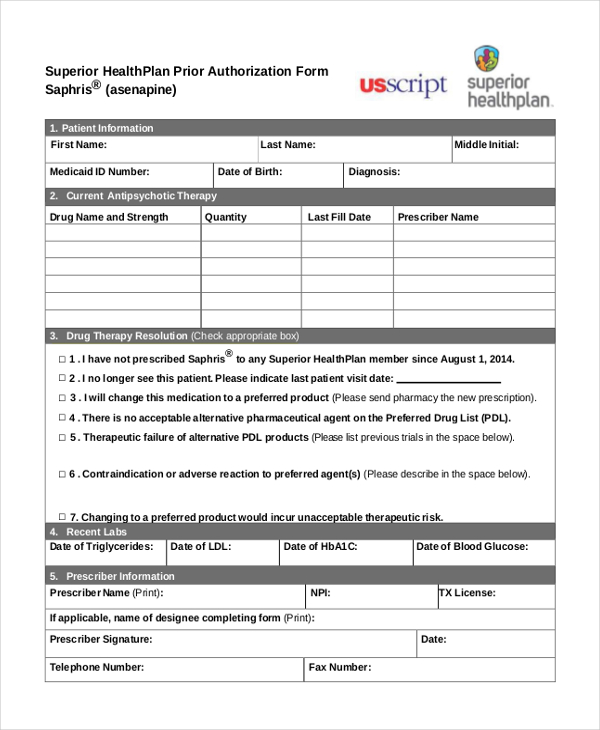
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
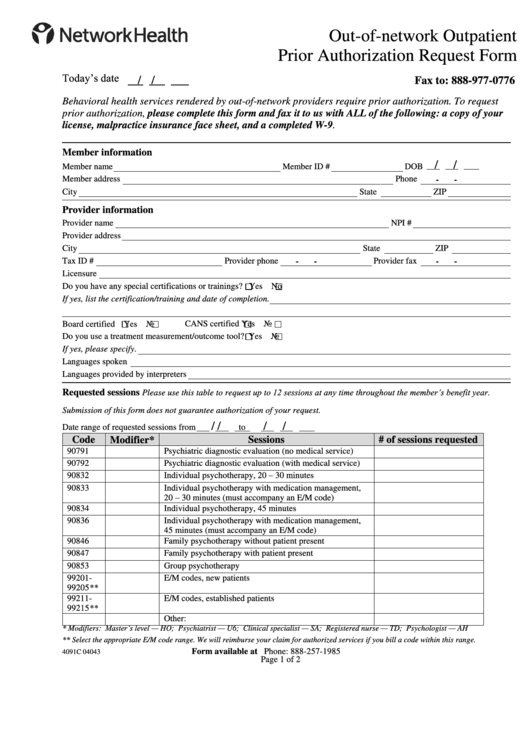
Top Network Health Prior Authorization Form Templates free to download
Health Plan of San Mateo Prior Authorization Form Fill Out and Sign
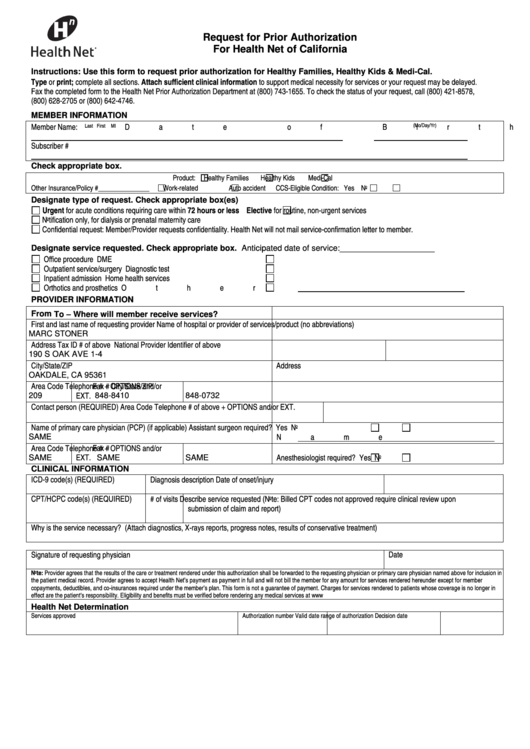
Free Health Net Prior (Rx) Authorization Form PDF eForms
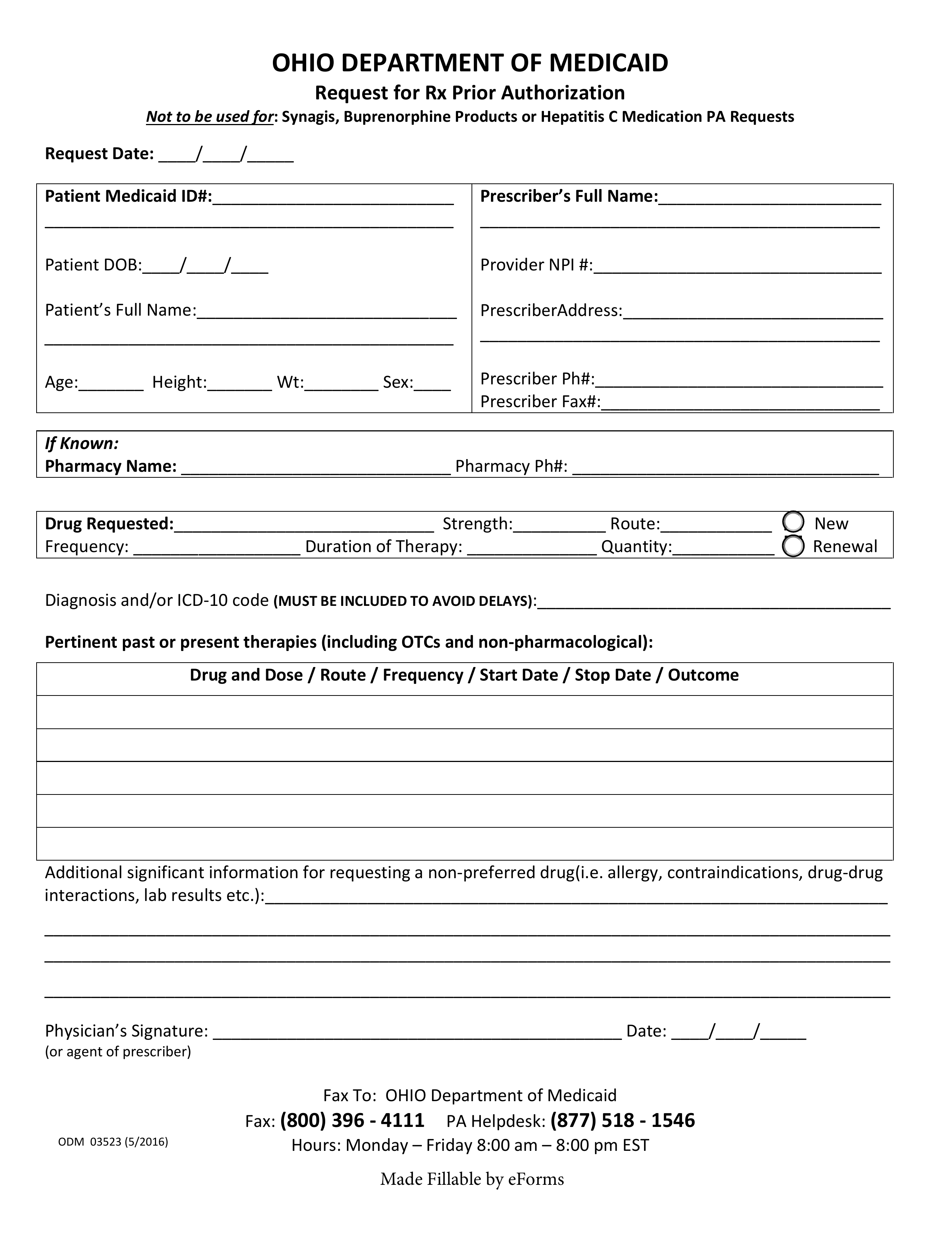
Free Ohio Medicaid Prior Authorization Form PDF eForms
Fillable Request For Prior Authorization For Health Net Of California
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
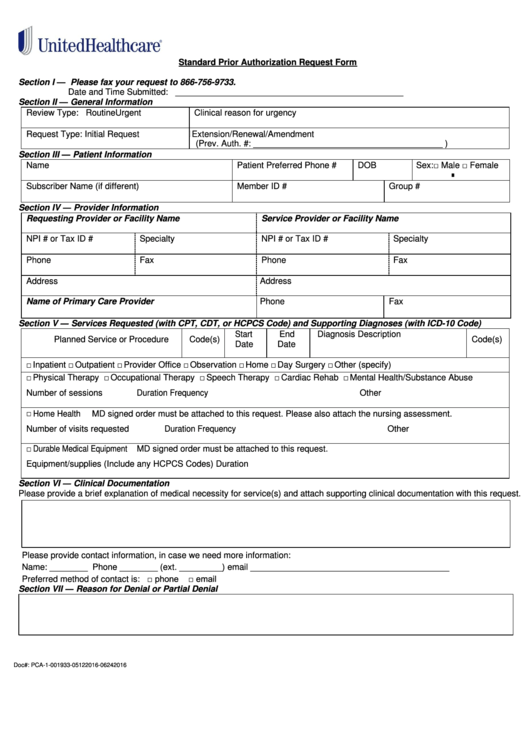
Fillable Standard Prior Authorization Request Form United Healthcare
Related Post: