Fep Prior Authorization Fax Form
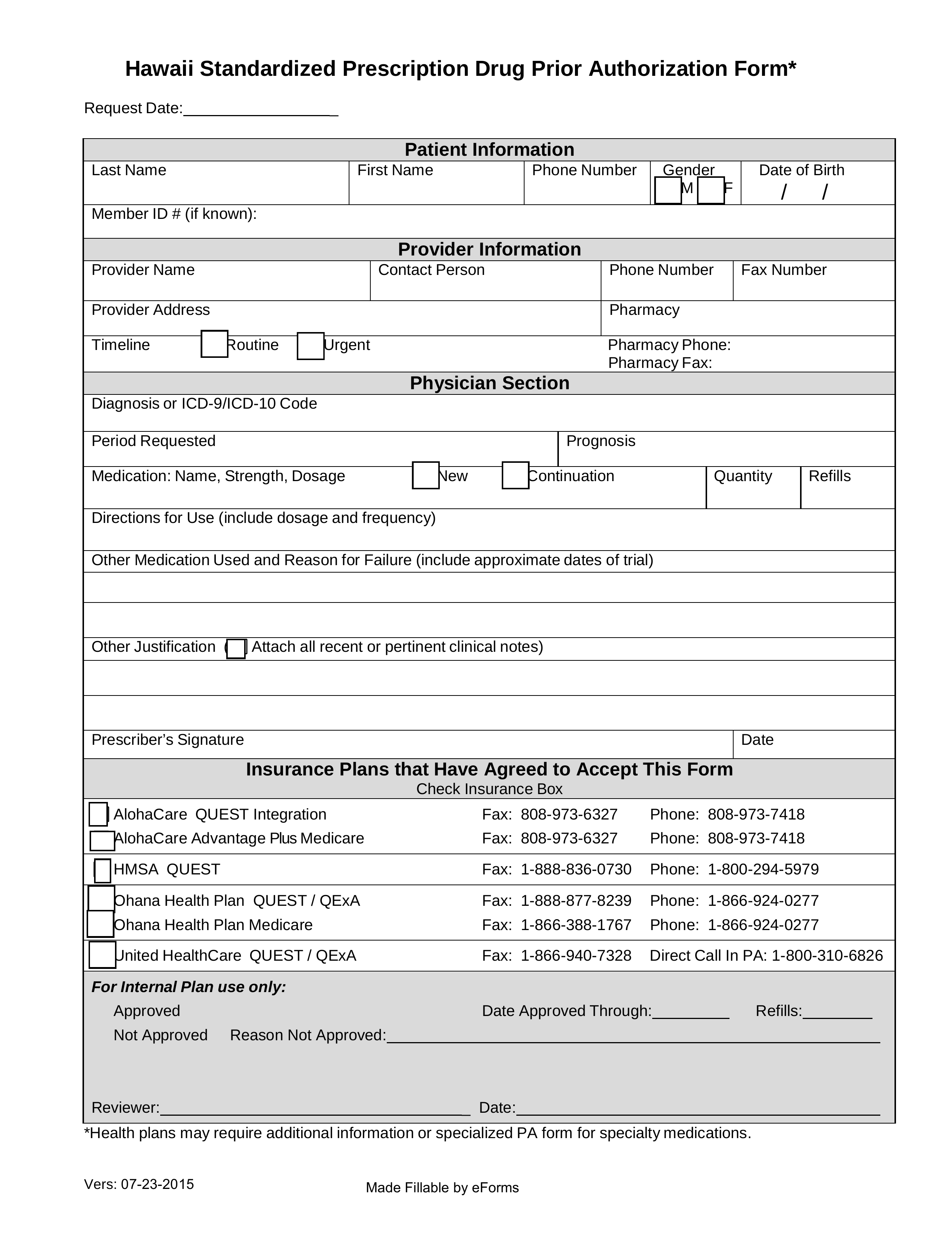
Fep Prior Authorization Fax Form - Get a faster response using availity for online submission you can now access online prior authorizations for premera members. Prior authorization forms claim forms view and download our medical, pharmacy and overseas claim forms find what you need by. Edit, sign and save svc requiring preauth form. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web select the appropriate fep form to get started. Please complete this form and submit it to wellmark to the fax number given below. Download a claim form for medical services, pharmacy services or overseas care. We have a network of over 55,000 preferred retail pharmacies nationwide to fill your prescriptions. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Web the following medical benefit medications require prior approval for blue cross and blue shield federal employee program® (bcbs fep®) members on standard option, basic. Get a faster response using availity for online submission you can now access online prior authorizations for premera members. Web all forms must be signed, then either faxed or mailed. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web get access to. Web help center 1 results found for search term : However, some select drugs require your doctor to provide information about your prescription to determine coverage. Submitting the request before the service helps premera pay claims faster with no surprise costs. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web prior. Write to you and maintain our denial; Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web most drugs are covered without requiring prior approval. Web prior authorization forms may be found at: Web select the appropriate fep form to get started. Prior authorization forms claim forms view and download our medical, pharmacy and overseas claim forms find what you need by. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). We have a network of over 55,000 preferred retail pharmacies nationwide to fill your prescriptions. Web your request for prior approval for the. Web provided herein is not sufficient to make a benefit determination or requires clarification and i agree to provide any such information to the insurer. Web get all the complete details below. Ask you or your provider for more information. We have a network of over 55,000 preferred retail pharmacies nationwide to fill your prescriptions. Web many services require prior. Ask you or your provider for more information. However, some select drugs require your doctor to provide information about your prescription to determine coverage. Web all forms must be signed, then either faxed or mailed. Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. Submitting the request before the service helps premera pay claims faster with no. Write to you and maintain our denial; Download a claim form for medical services, pharmacy services or overseas care. Web help center 1 results found for search term : Web most drugs are covered without requiring prior approval. Web get access to over 55,000 retail pharmacies nationwide. Ad register and subscribe now to work on your simply healthcare svc requiring pre auth form. Web help center 1 results found for search term : However, some select drugs require your doctor to provide information about your prescription to determine coverage. Web get access to over 55,000 retail pharmacies nationwide. Web your request for prior approval for the service,. Ask you or your provider for more information. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Edit, sign and save svc requiring preauth form. Web if the drug/procedure/service is not found in the lists of procedures requiring prior approval below or the. Get a faster response using availity for online submission you can now access online prior authorizations for premera members. Web your request for prior approval for the service, drug or supply; If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web provided herein. Explore prior approval topics learn about prior. Web get all the complete details below. Please complete this form and submit it to wellmark to the fax number given below. Web prior authorization forms may be found at: Web help center 1 results found for search term : However, some select drugs require your doctor to provide information about your prescription to determine coverage. For members enrolled in standard option: Web most drugs are covered without requiring prior approval. Submitting the request before the service helps premera pay claims faster with no surprise costs. Web all forms must be signed, then either faxed or mailed. Covermymeds is fep prior authorization forms’s preferred method for receiving epa requests. Ask you or your provider for more information. Get a faster response using availity for online submission you can now access online prior authorizations for premera members. Web the following medical benefit medications require prior approval for blue cross and blue shield federal employee program® (bcbs fep®) members on standard option, basic. Web provided herein is not sufficient to make a benefit determination or requires clarification and i agree to provide any such information to the insurer. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. Web get access to over 55,000 retail pharmacies nationwide. Ad register and subscribe now to work on your simply healthcare svc requiring pre auth form. Edit, sign and save svc requiring preauth form. Web your request for prior approval for the service, drug or supply;Free Hawaii Medicaid Prior (Rx) Authorization Form PDF eForms
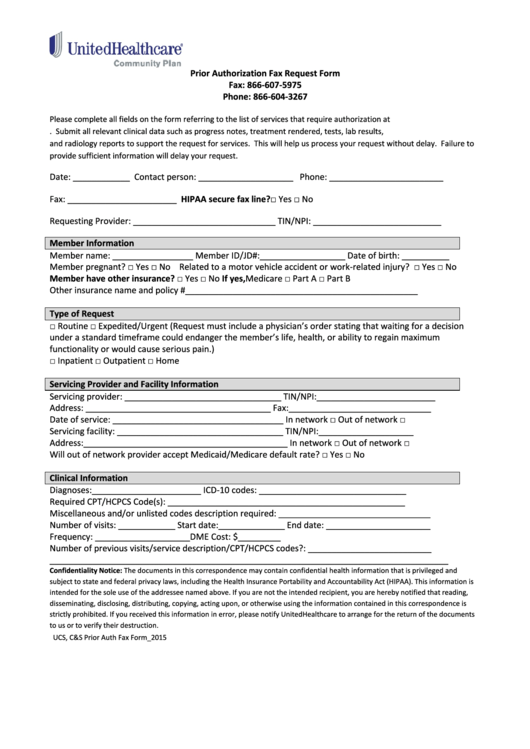
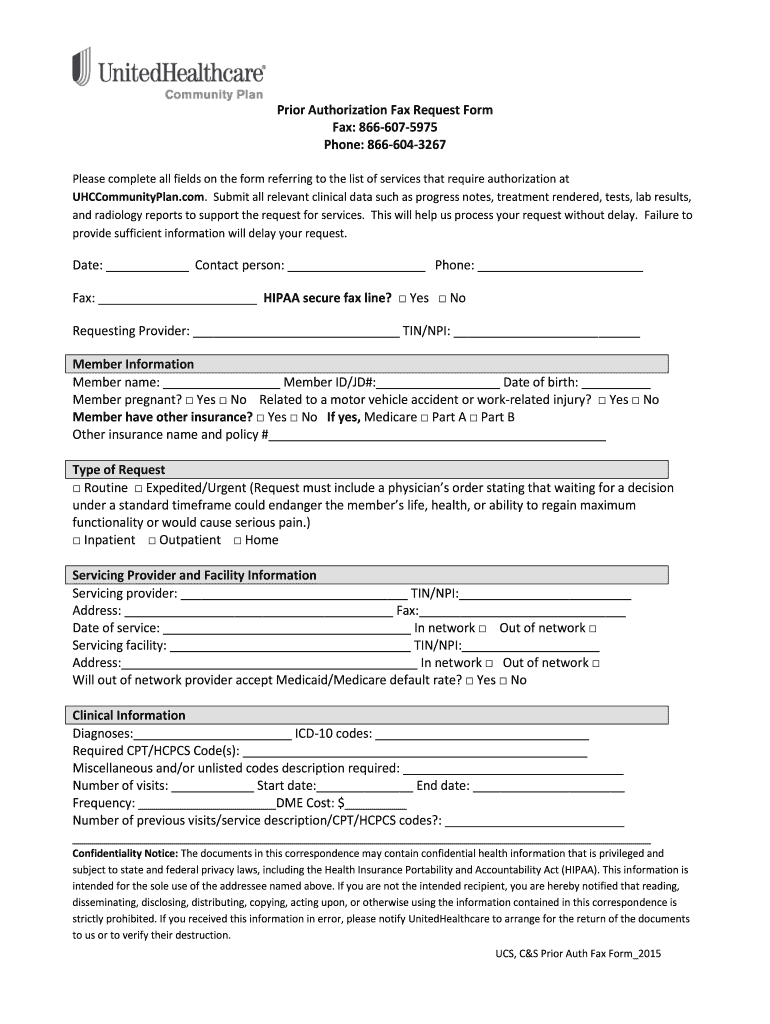
Prior Authorization Fax Request Form printable pdf download
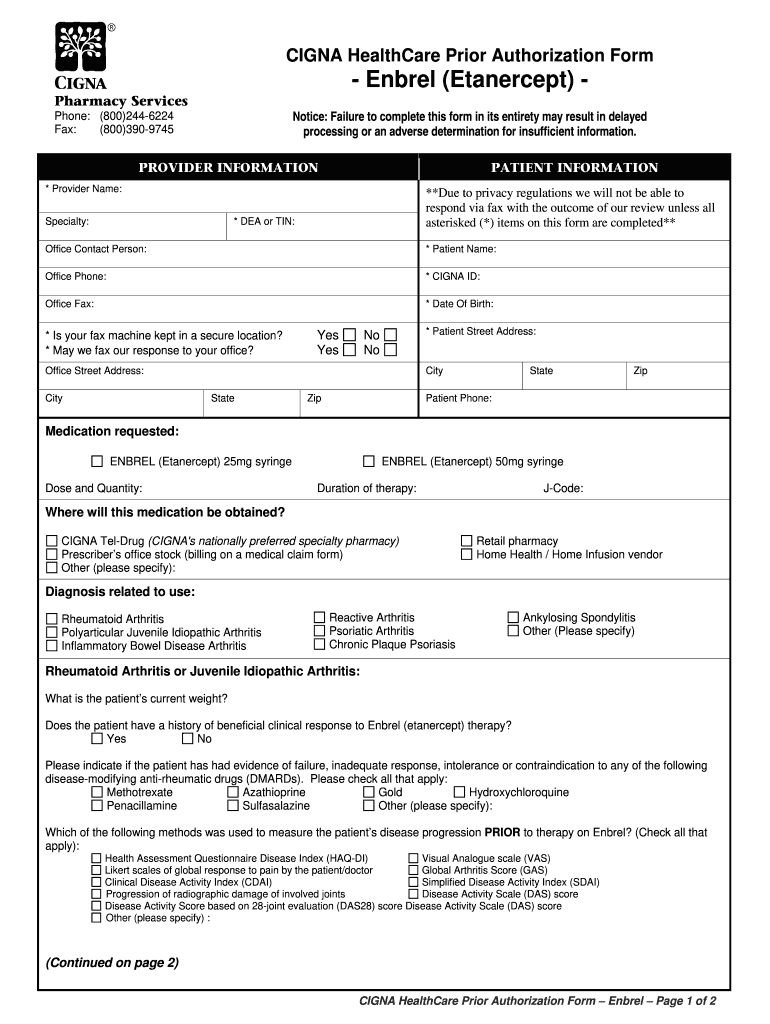
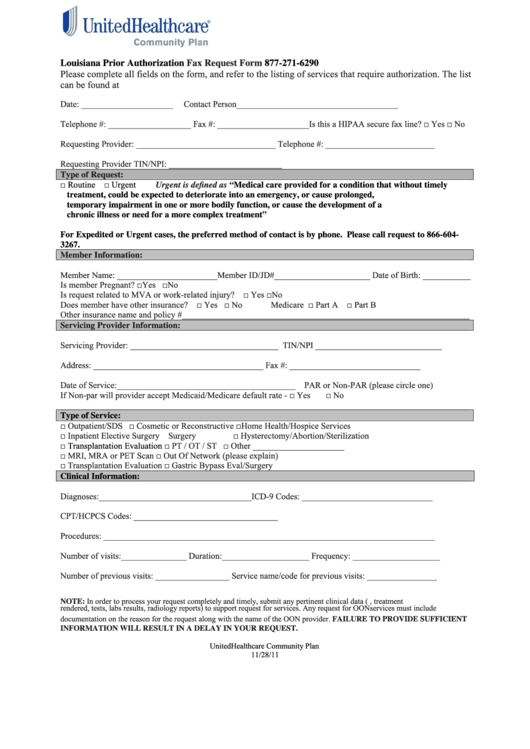
Prior Authorization Form Fill Out and Sign Printable PDF Template
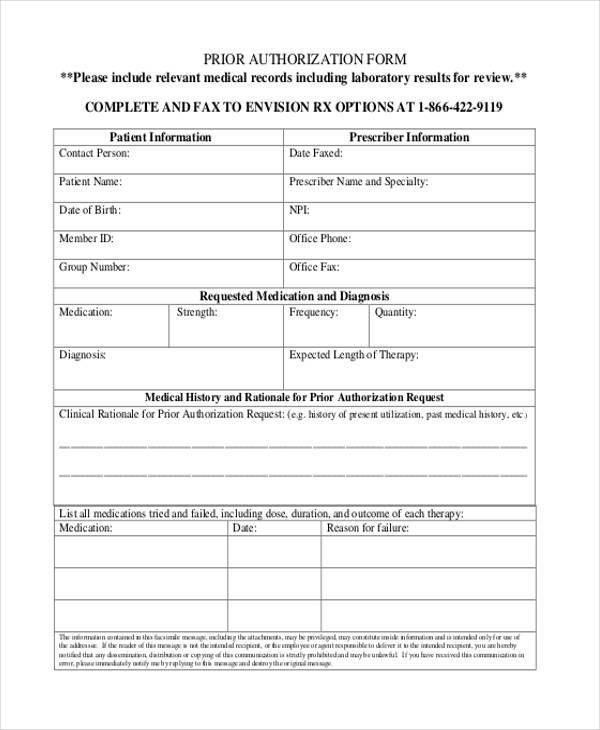
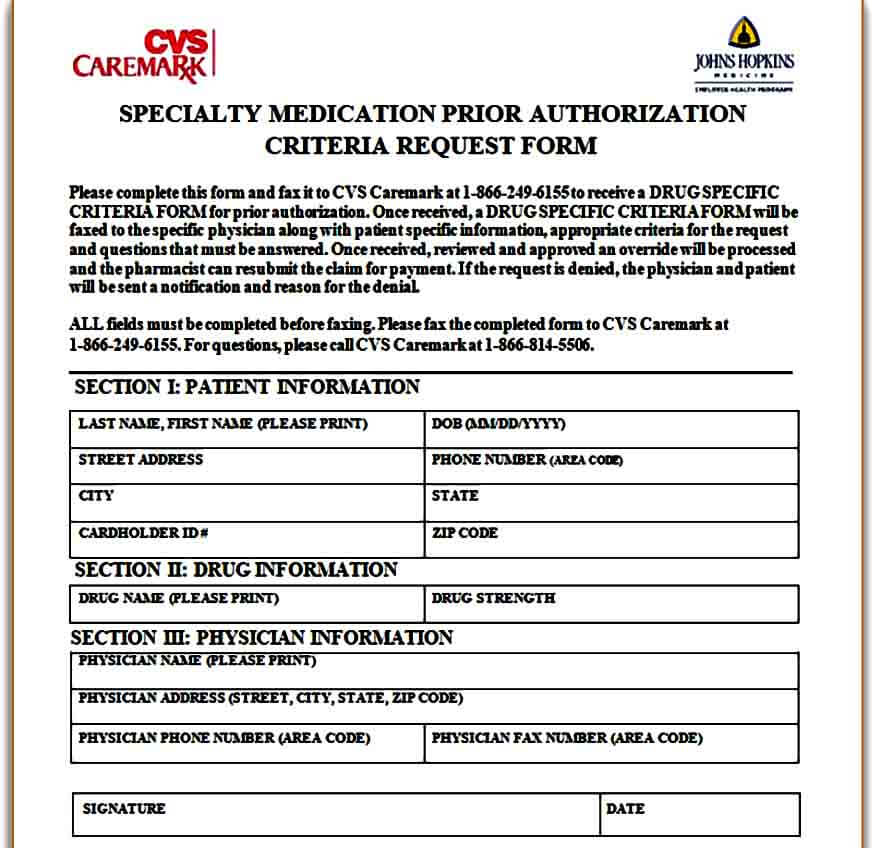
FREE 35+ Sample Authorization Forms in PDF
Authorization Fax Request Form Fill Online, Printable, Fillable
FREE 42+ Blank Authorization Forms in PDF Excel MS Word
Fillable Louisiana Prior Authorization Fax Request Form printable pdf
Prior Authorization Preferred Drug List Printable Pdf Download
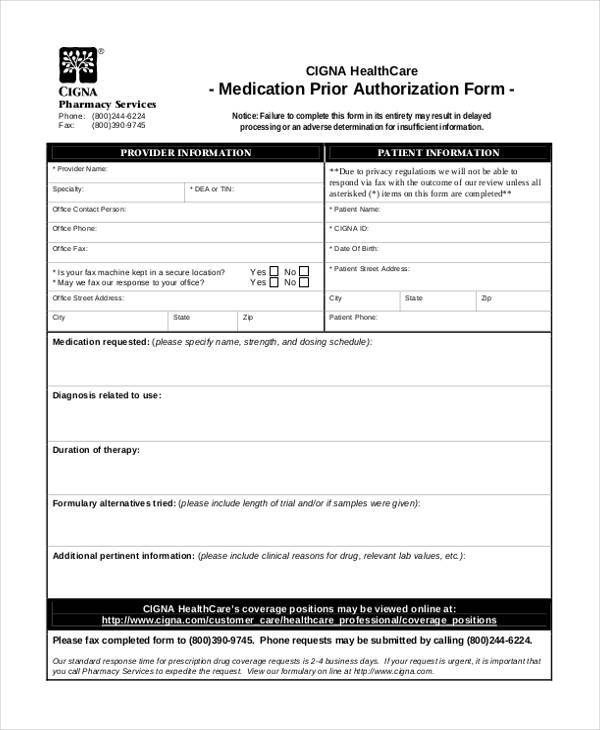
Prior Authorization Form Complete And Fax To Catalyst Rx At 888852
Template Caremark Prior Authorization Form Mous Syusa
Related Post: