Federal Employee Program Fep Prior Authorization Form
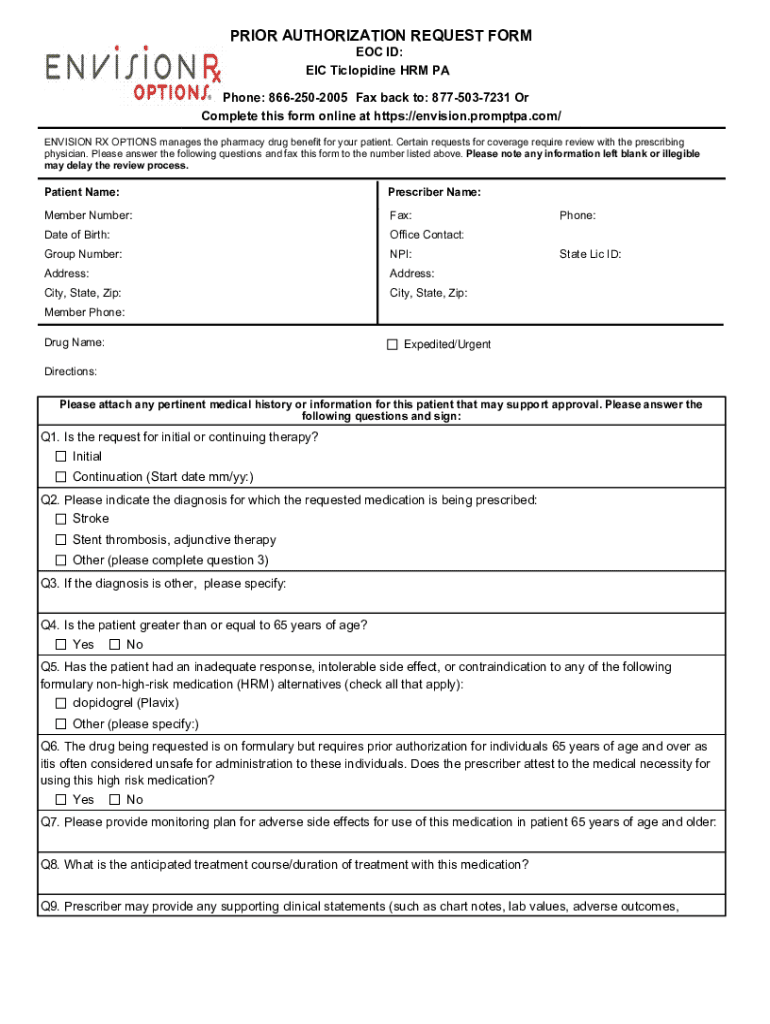
Federal Employee Program Fep Prior Authorization Form - Eastern time (excluding holidays) call the national information center for information about your benefits and services,. Web the following medical benefit medications require prior approval for blue cross and blue shield federal employee program® (bcbs fep®) members on standard option,. Web prior approval lists by plan. Blue cross and blue shield of texas (bcbstx) is continuing to make enhancements to its behavioral health (bh) prior. Web federal employee program (fep) services requiring prior authorization or notification. Web then, you will have to file a retail prescription drug claim form for reimbursement. See what's new for 2024 check out your new prescription benefits available to eligible. Web learn how we manage prior authorization & medical necessity determination requests for certain orthopedic and cardiac services for our fep members. Web now available for commercial and federal employee program (fep) members since april 2021, carefirst bluecross blueshield and carefirst bluechoice,. Basic option members and fep blue focus members cannot use their pharmacy benefit at. Web 2022 federal employee program. Effective 1/1/2022, our blue cross and blue shield of texas. Web posted 8/3/2023 updated 10/19/23. Web federal employee program (fep) blue focus is a new plan that requires prior authorization on more services than other fep plans typically require. Blue cross and blue shield of texas (bcbstx) is continuing to make enhancements to its behavioral. Web retired federal employee with bcbs fep we'd suggest starting in one of these areas: Standard and basic option prior approval list fep blue focus prior approval list. Web 2022 federal employee program. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web. Web federal employee program (fep) medical authorizations. Standard and basic option prior approval list fep blue focus prior approval list. Blue cross and blue shield of texas (bcbstx) is continuing to make enhancements to its behavioral health (bh) prior. Prior authorization forms claim forms view and download our medical, pharmacy and overseas claim forms find. Web retired federal employee with. Web view these quick reference guides to learn more about our health and wellness programs. Service benefit plan prior approval p.o. See what's new for 2024 check out your new prescription benefits available to eligible. Web posted 8/3/2023 updated 10/19/23. Web prior authorization is required from bcbstx for all inpatient, partial hospitalization and outpatient behavioral health services. See what's new for 2024 check out your new prescription benefits available to eligible. Web retired federal employee with bcbs fep we'd suggest starting in one of these areas: If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. A prior approval, or pa,. Standard and basic option prior approval list fep blue focus prior approval list. Effective 1/1/2022, our blue cross and blue shield of texas. See what's new for 2024 check out your new prescription benefits available to eligible. Web federal employee program (fep) medical authorizations. Basic option members and fep blue focus members cannot use their pharmacy benefit at. Web coverage & care help center 1 results found for search term : Web learn how we manage prior authorization & medical necessity determination requests for certain orthopedic and cardiac services for our fep members. Basic option members and fep blue focus members cannot use their pharmacy benefit at. Download a claim form for medical services, pharmacy services or overseas. Web coverage & care help center 1 results found for search term : Prior authorization and benefit updates. Web retired federal employee with bcbs fep we'd suggest starting in one of these areas: Web posted 8/3/2023 updated 10/19/23. Web view these quick reference guides to learn more about our health and wellness programs. Web then, you will have to file a retail prescription drug claim form for reimbursement. Web prior approval lists by plan. See what's new for 2024 check out your new prescription benefits available to eligible. Web prior authorization is required from bcbstx for all inpatient, partial hospitalization and outpatient behavioral health services. Prior authorization forms claim forms view and download. Web federal employee program (fep) medical authorizations. Web then, you will have to file a retail prescription drug claim form for reimbursement. Web coverage & care help center 1 results found for search term : Web prior authorization is required from bcbstx for all inpatient, partial hospitalization and outpatient behavioral health services. Web learn how we manage prior authorization &. Web 2022 federal employee program. Effective 1/1/2022, our blue cross and blue shield of texas. Basic option members and fep blue focus members cannot use their pharmacy benefit at. Prior authorization and benefit updates. Prior authorization forms claim forms view and download our medical, pharmacy and overseas claim forms find. Web coverage & care help center 1 results found for search term : Download a claim form for medical services, pharmacy services or overseas care. To obtain prior authorization, call: Web federal employee program (fep) medical authorizations. Web posted 8/3/2023 updated 10/19/23. Web then, you will have to file a retail prescription drug claim form for reimbursement. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Standard and basic option prior approval list fep blue focus prior approval list. Web federal employee program (fep) blue focus is a new plan that requires prior authorization on more services than other fep plans typically require. Service benefit plan prior approval p.o. Web retired federal employee with bcbs fep we'd suggest starting in one of these areas: A prior approval, or pa, review determines medical necessity and considers fep benefits before a treatment,. Web learn how we manage prior authorization & medical necessity determination requests for certain orthopedic and cardiac services for our fep members. Web prior approval lists by plan. Web now available for commercial and federal employee program (fep) members since april 2021, carefirst bluecross blueshield and carefirst bluechoice,.EnvisionRxOptions Prior Authorization Request Form Fill and Sign
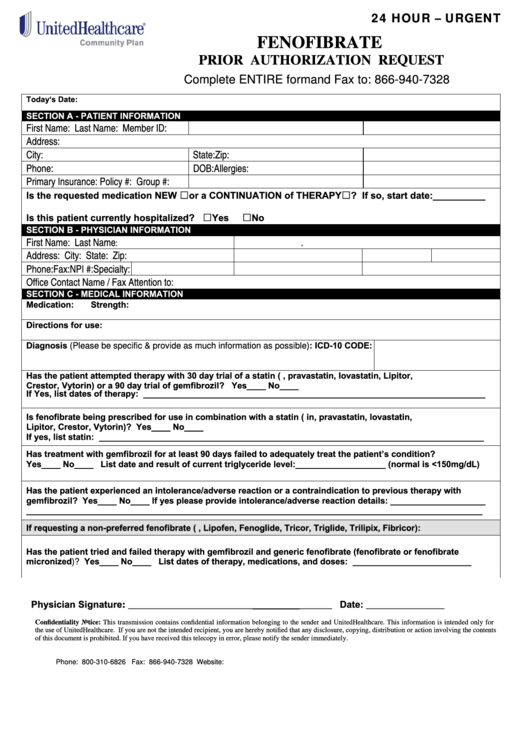
Fillable Unitedhealthcare Prior Authorization Request Form
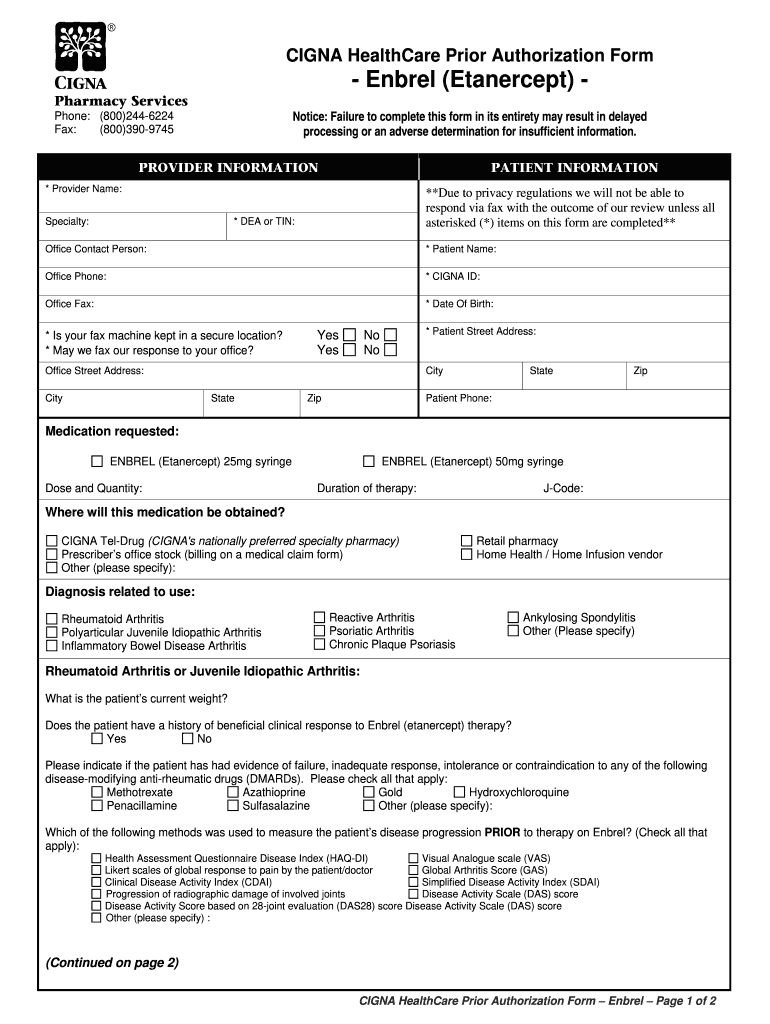
Federal Employee Program Fep Prior Authorization Form
Prior Authorization Form Fill Out and Sign Printable PDF Template
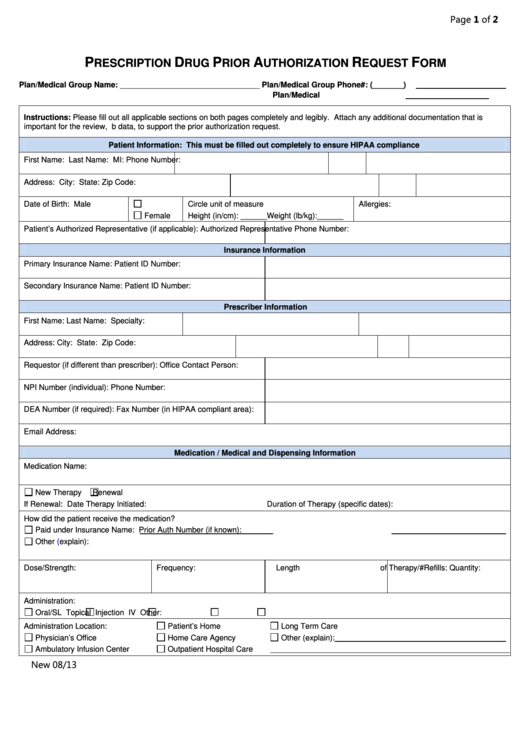
Fillable Prescription Drug Prior Authorization Request Form printable
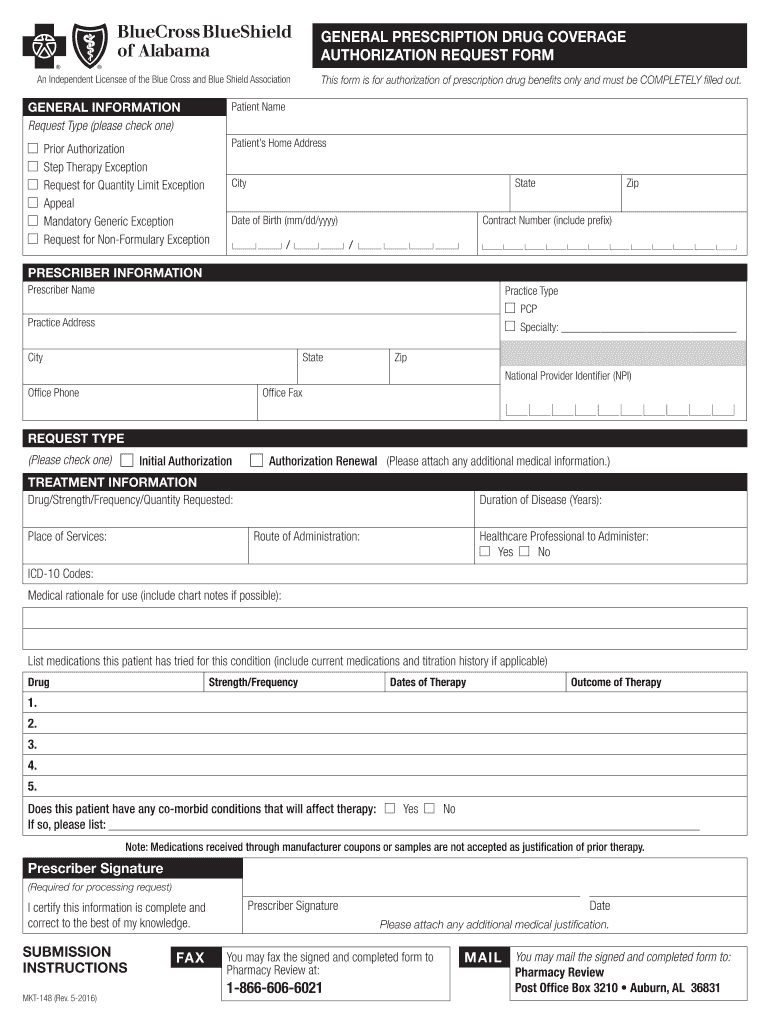
Bcbs Alabama Prior Authorization Fill Out and Sign Printable PDF
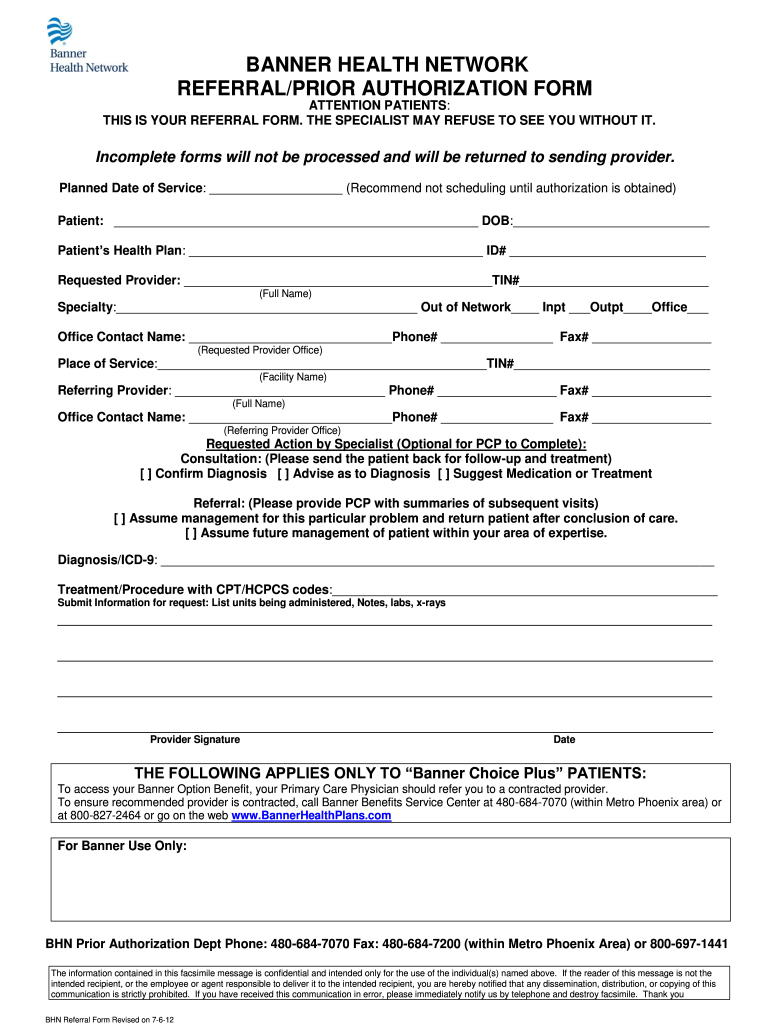
Banner Aetna Prior Authorization Form Fill Out and Sign Printable PDF
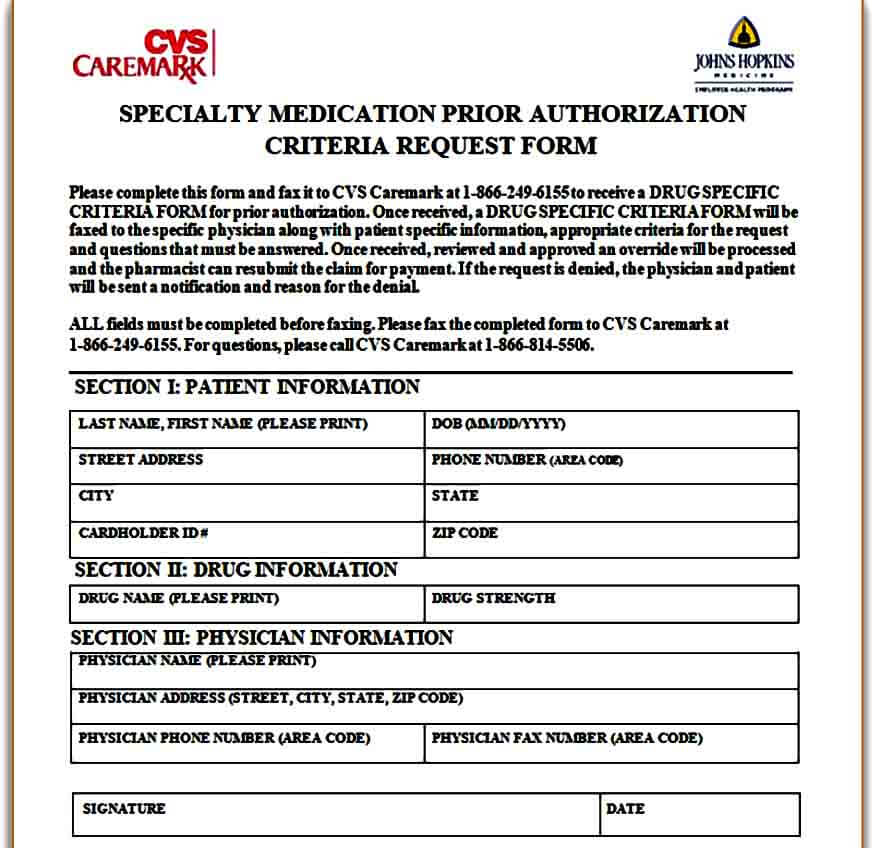
Template Caremark Prior Authorization Form Mous Syusa
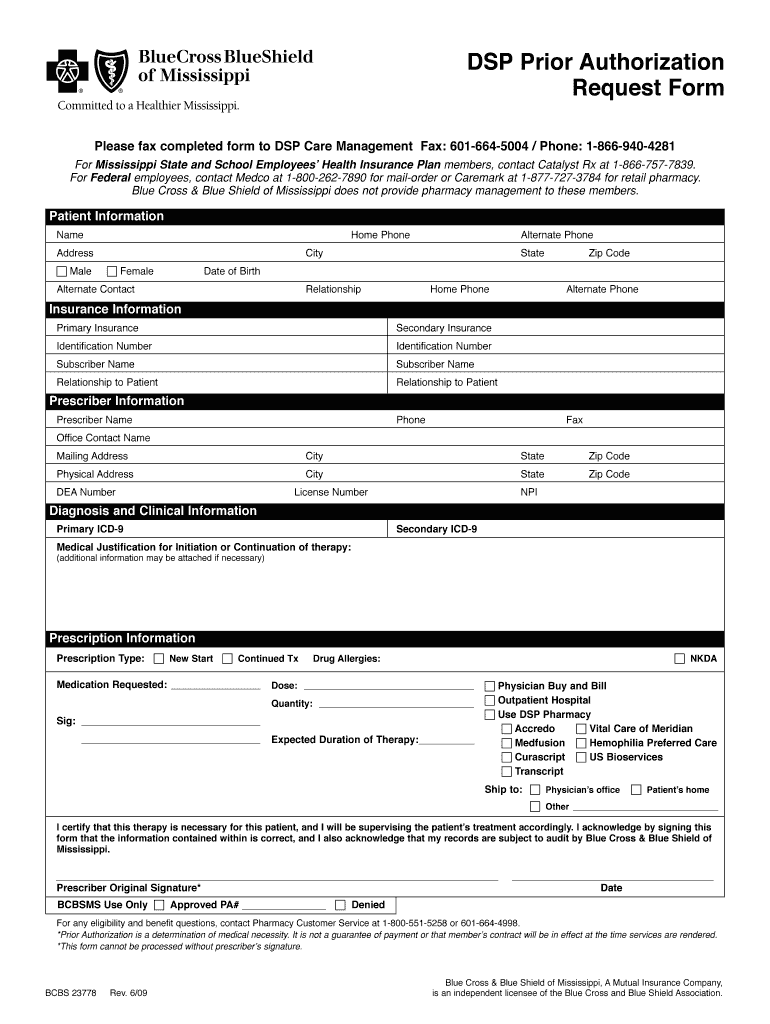
Bcbs Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Fep blue dental Fill out & sign online DocHub
Related Post: