Credence Bcbs Prior Authorization Form
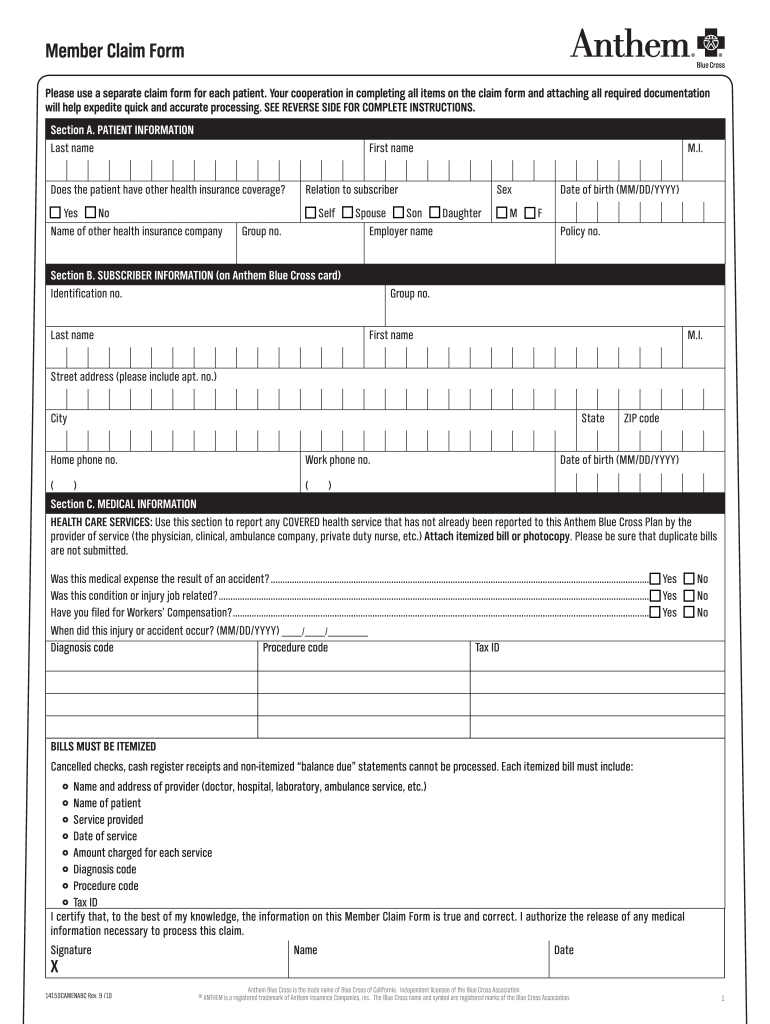
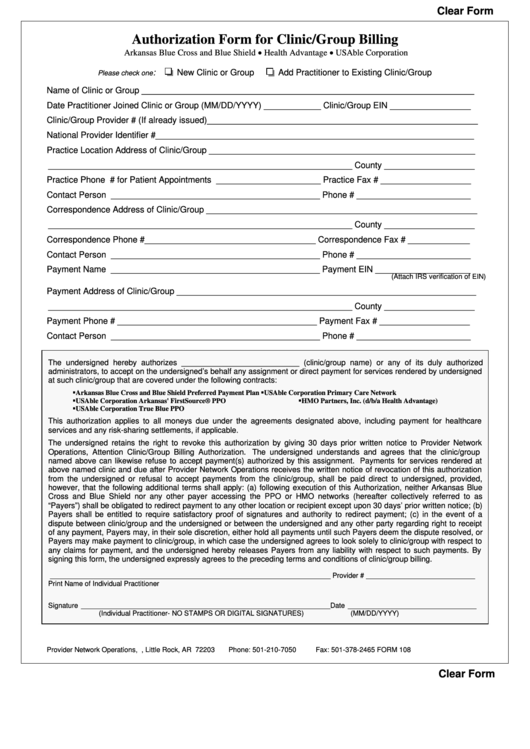
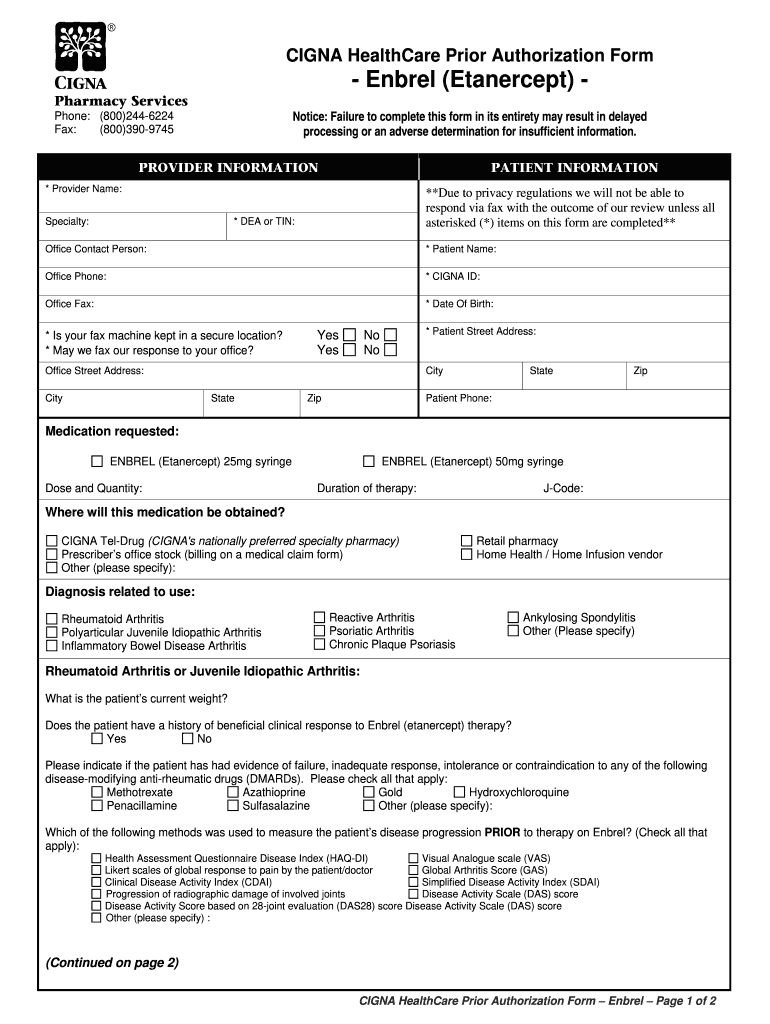
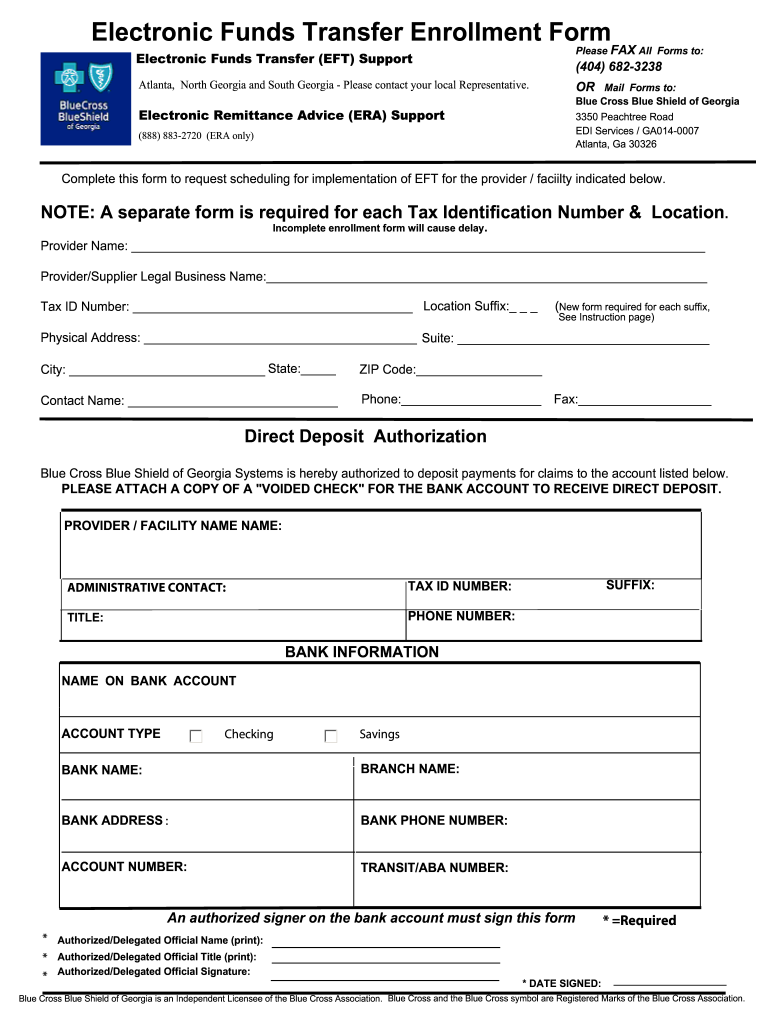
Credence Bcbs Prior Authorization Form - Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Complete our online policy feedback form. Web an independent licensee of the blue cross and blue shield association ii. If you do not see your plan, please login to your online account to view your. Together we look for ways to help our members get the medication they need to feel better and live well, while. Web click on the appropriate link below to print the form to request prior authorization for these drugs: Web please select your designated plan from the dropdown below and then search your specific drug list. Web prime therapeutics serves as credence's pharmacy benefit manager. Below is the list of specific. Web general equipment see the sections on the back of the form for oxygen and ippb 12. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. Web click on the appropriate link below to print the form to request prior authorization. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. General equipment selected for patient a. Send comments with supporting documentation by mail. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval. Some medications allow a certain quantity of. To submit a prior authorization online, please click the button below to use the web form. Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. Web ask your provider to go to prior authorization requests to get forms and information on services that. Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. Select the type of information requested. Below is the list of specific. Credence offers health insurance, including medical, dental and prescription drug. Use the navigation on the left to locate specific policy information or search using the policy title, policy number. Web download prior approval documents. Send comments with supporting documentation by mail or fax. Complete our medical policy feedback form online, or. Web make sure your voice is heard by providing feedback directly to us: Web an independent licensee of the blue cross and blue shield association ii. Use the navigation on the left to locate specific policy information or search using the policy title, policy number or keywords. To submit a prior authorization online, please click the button below to use the web form. Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. Buprenorphine and buprenorphine/naloxone prior. Web prime therapeutics serves as credence's pharmacy benefit manager. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. 1 file (s) 135.52 kb. If you do not see your plan, please login to your online account to view your. Web an independent licensee. General equipment selected for patient a. Web 90 degree benefits prior authorization request form. Web click on the appropriate link below to print the form to request prior authorization for these drugs: Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. Treating provider information provider name phone number fax number. Web please select your designated plan from the dropdown below and then search your specific drug list. If you do not see your plan, please login to your online account to view your. Credence offers health insurance, including medical, dental and prescription drug. Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other. Web make sure your voice is heard by providing feedback directly to us: General equipment selected for patient a. Complete our online policy feedback form. Web an independent licensee of the blue cross and blue shield association ii. Below is the list of specific. Select the type of information requested. Treating provider information provider name phone number fax number mailing address city. Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. 1 file (s) 135.52 kb. Web get helpful tips and insights on the topics that are most important to you. To submit a prior authorization online, please click the button below to use the web form. Web download prior approval documents. Web please select your designated plan from the dropdown below and then search your specific drug list. General equipment selected for patient a. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. Web prime therapeutics serves as credence's pharmacy benefit manager. Together we look for ways to help our members get the medication they need to feel better and live well, while. Credence offers health insurance, including medical, dental and prescription drug. Use the navigation on the left to locate specific policy information or search using the policy title, policy number or keywords. Below is the list of specific. Send comments with supporting documentation by mail. Web precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered services. Buprenorphine and buprenorphine/naloxone prior authorization form. Send comments with supporting documentation by mail or fax.Anthem Claim Action Request Form Fill Out and Sign Printable PDF
Bcbs Prior Auth Forms To Print Fill Online, Printable, Fillable
Fillable Bcbs Authorization Form For Clinic/group Billing printable pdf
Beautiful Bcbs Centennial Care Prior Authorization form
TN BCBS 19PED504697 2019 Fill and Sign Printable Template Online US
20152023 Blue Advantage BCBS Medicare Part D Prescription Drug
Prior Authorization Form Fill Out and Sign Printable PDF Template
Bcbs Prior Authorization Form PDF Fill Out and Sign Printable PDF
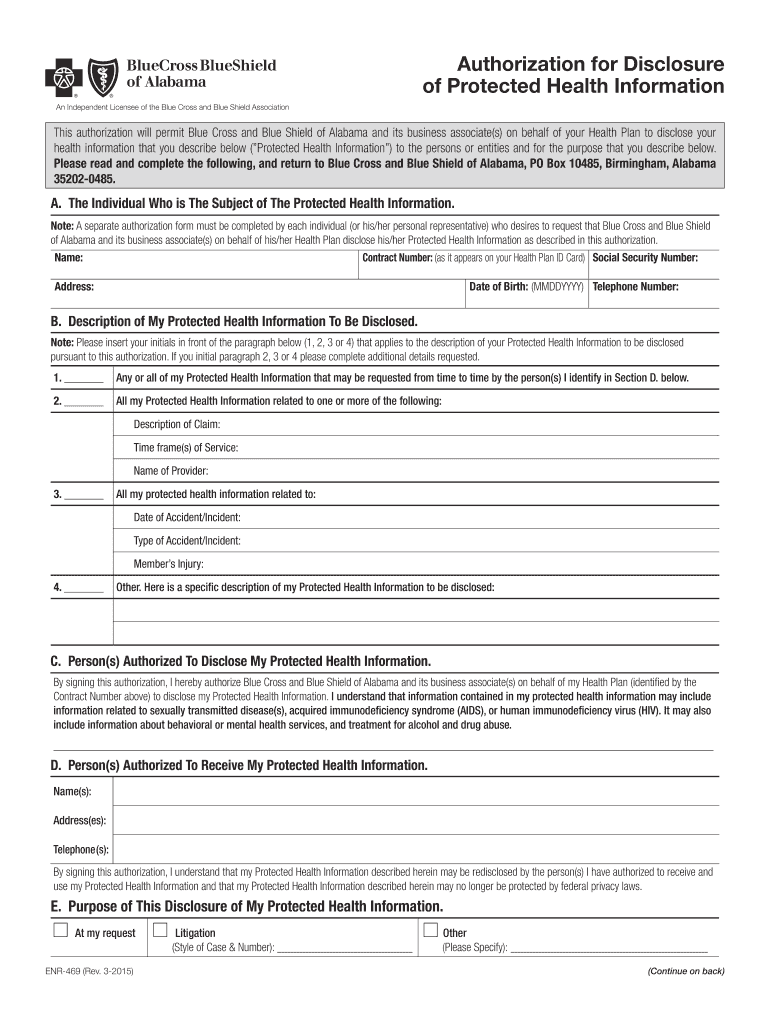
Bcbs alabama authorization form Fill out & sign online DocHub
Bcbs Prior Authorization Form Maryland Form Resume Examples Yqlkmob5aj
Related Post: