Bcbs Highmark Prior Authorization Form
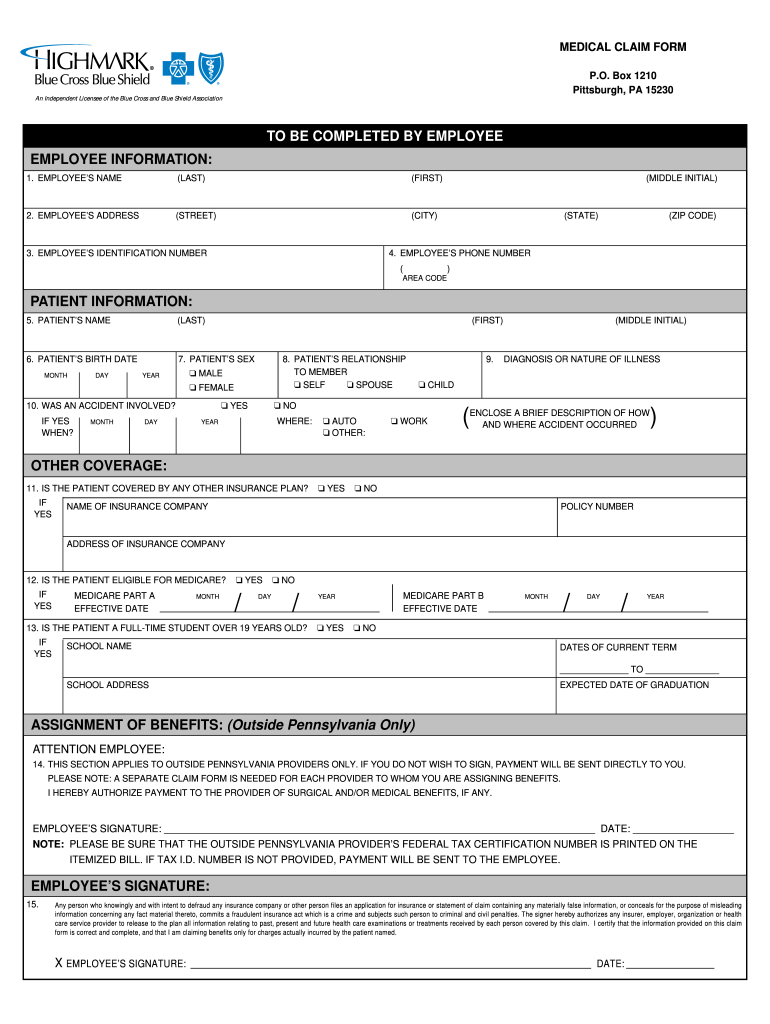
Bcbs Highmark Prior Authorization Form - Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional. † agents used for fibromyalgia (e.g. Web medical specialty drug authorization outpatient chemotherapy outpatient chemotherapy aloxi (j1469) outpatient chemotherapy avastin outpatient. Your ppo plan covers vaccinations in most cases. However, if your employer purchased your plan before the affordable care act was enacted, you may. Testosterone product prior authorization form. Covermymeds is highmark blue shield prior authorization forms’s preferred. Web requiring authorization pharmacy policy search miscellaneous forms on this page, you will find some recommended forms that providers may use when. Complete and fax all requested information below including any supporting documentation as applicable to. Web medicare part d hospice prior authorization information. Testosterone product prior authorization form. Web prior authorization code lookup. Web durable medical equipment (dme) prior authorization request form. Web forms and reports picture_as_pdf abortion consent form picture_as_pdf advance directive form picture_as_pdf applied behavioral analysis (aba) prior authorization. Covermymeds is highmark blue shield prior authorization forms’s preferred. Web pharmacy prior authorization forms addyi prior authorization form armodafinil prior authorization form blood disorders medication request form cgrp inhibitors. Complete and fax all requested information below including any supporting documentation as applicable to. Web durable medical equipment (dme) prior authorization request form. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization:. Pcsk9 inhibitor prior authorization form; Complete and fax all requested information below including any supporting documentation as applicable to. Web prior authorization code lookup. Testosterone product prior authorization form. Find out if prior authorization from highmark health options is required for medical procedures and services. † agents used for fibromyalgia (e.g. Web pharmacy prior authorization forms addyi prior authorization form armodafinil prior authorization form blood disorders medication request form cgrp inhibitors. Web prior authorization code lookup. Web medicare part d hospice prior authorization information. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization: Covermymeds is highmark blue shield prior authorization forms’s preferred. Web outpatient therapy services prior authorization request form use this form for all physical, occupational, speech, and feeding therapies, pulmonary and cardiac. † agents used for fibromyalgia (e.g. Web medical specialty drug authorization outpatient chemotherapy outpatient chemotherapy aloxi (j1469) outpatient chemotherapy avastin outpatient. Pcsk9 inhibitor prior authorization form; Web forms and reference material; Web requiring authorization pharmacy policy search miscellaneous forms on this page, you will find some recommended forms that providers may use when. Web pharmacy prior authorization forms addyi prior authorization form armodafinil prior authorization form blood disorders medication request form cgrp inhibitors. Web medical specialty drug authorization outpatient chemotherapy outpatient chemotherapy aloxi (j1469) outpatient chemotherapy. Pcsk9 inhibitor prior authorization form; Web pharmacy prior authorization forms addyi prior authorization form armodafinil prior authorization form blood disorders medication request form cgrp inhibitors. Web medicare part d hospice prior authorization information. Web for other helpful information, please visit the highmark web site at: Web medical specialty drug authorization outpatient chemotherapy outpatient chemotherapy aloxi (j1469) outpatient chemotherapy avastin outpatient. Web prior authorization code lookup. Web for a complete list of services requiring authorization, please access the authorization requirements page on the highmark provider resource center under claims, payment. Web outpatient therapy services prior authorization request form use this form for all physical, occupational, speech, and feeding therapies, pulmonary and cardiac. † agents used for fibromyalgia (e.g. Use this form. Web specialty drugs requiring prior authorization for specialty drugs within the therapeutic categories listed below, the diagnosis, applicable lab data, and additional. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional. Web modafinil and armodafinil pa form; Web for a complete list of services requiring authorization,. Transition and continuity of care; Complete and fax all requested information below including any supporting documentation as applicable to. Testosterone product prior authorization form. Use this form to request coverage/prior authorization of medications for individuals in hospice care. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus. Your ppo plan covers vaccinations in most cases. Use this form to request coverage/prior authorization of medications for individuals in hospice care. Web specialty drugs requiring prior authorization for specialty drugs within the therapeutic categories listed below, the diagnosis, applicable lab data, and additional. Find out if prior authorization from highmark health options is required for medical procedures and services. Web prior authorization below is a list of common drugs and/or therapeutic categories that require prior authorization: Pcsk9 inhibitor prior authorization form; Web for other helpful information, please visit the highmark web site at: Web durable medical equipment (dme) prior authorization request form. Complete and fax all requested information below including any supporting documentation as applicable to. Web forms and reference material; Covermymeds is highmark blue shield prior authorization forms’s preferred. Web prior authorization for the following drugs and/or therapeutic categories, the diagnosis, applicable lab data, and involvement of specialists are required, plus additional. Web pharmacy prior authorization forms addyi prior authorization form armodafinil prior authorization form blood disorders medication request form cgrp inhibitors. Transition and continuity of care; Web medicare part d hospice prior authorization information. Web prior authorization code lookup. Testosterone product prior authorization form. However, if your employer purchased your plan before the affordable care act was enacted, you may. Web for a complete list of services requiring authorization, please access the authorization requirements page on the highmark provider resource center under claims, payment. Web medical specialty drug authorization outpatient chemotherapy outpatient chemotherapy aloxi (j1469) outpatient chemotherapy avastin outpatient.Highmark BCBS CLM038 2000 Fill and Sign Printable Template Online
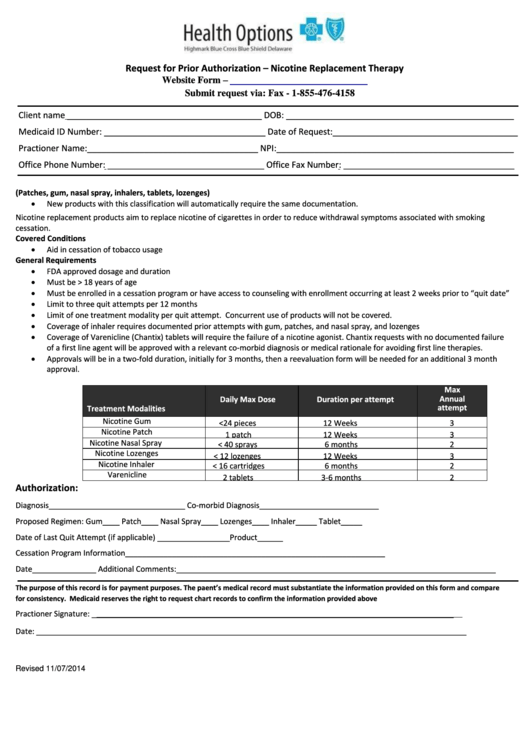
Request For Prior Authorization Form Highmark Blue Cross Blue Shield
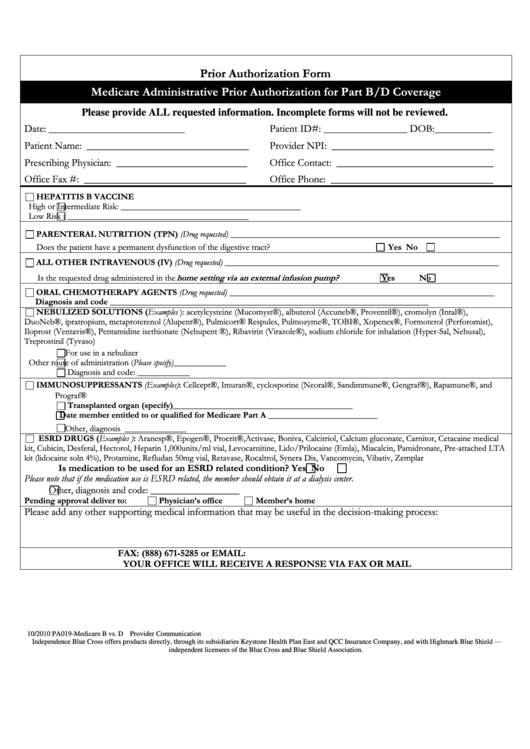
Medicare Administrative Prior Authorization For Part B/d Coverage
Free Prior (Rx) Authorization Forms PDF eForms
Covermymeds Humana Prior Auth Form Humana Prior Authorization Form
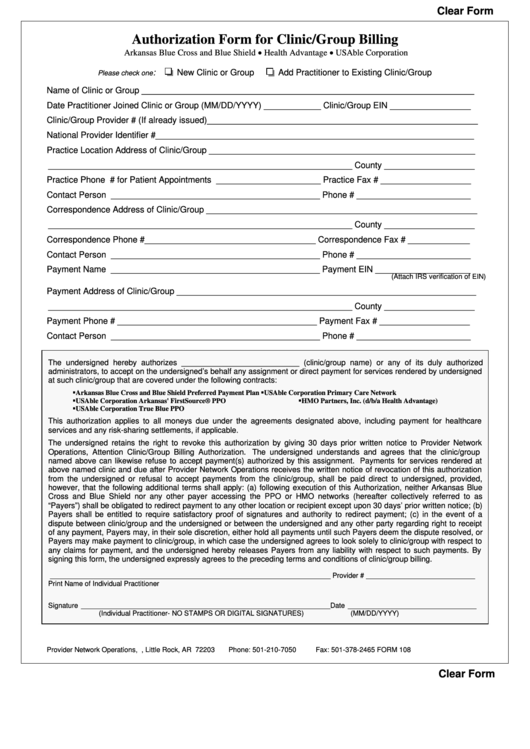
Fillable Bcbs Authorization Form For Clinic/group Billing printable pdf
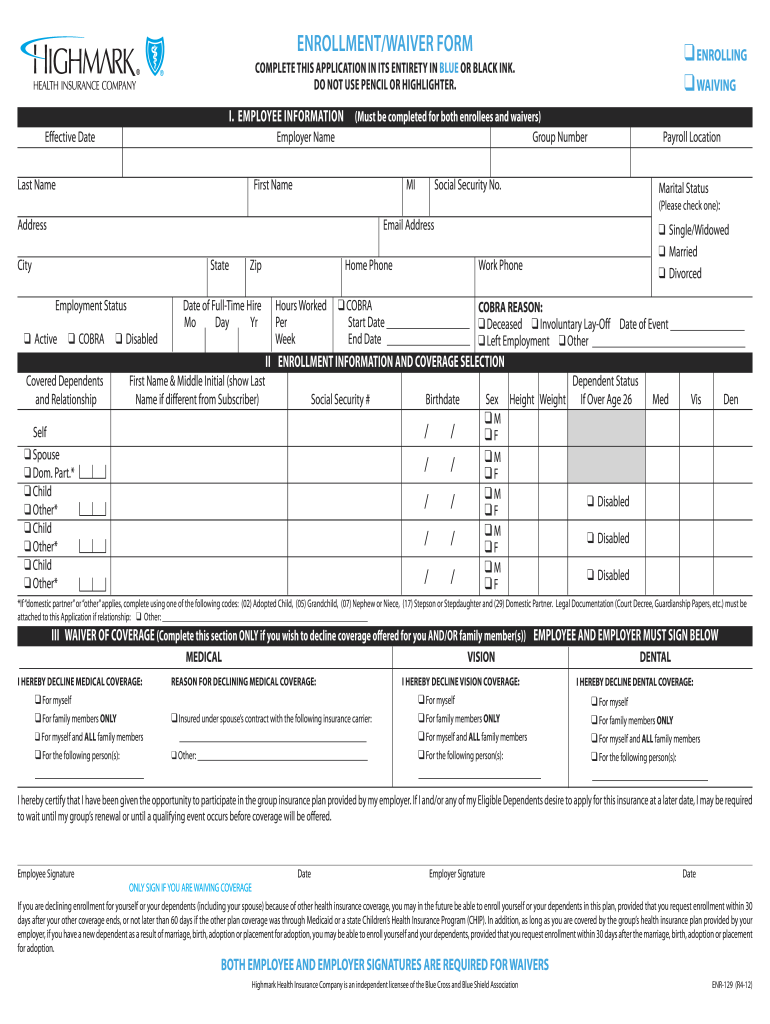
Highmark enrollment form Fill out & sign online DocHub
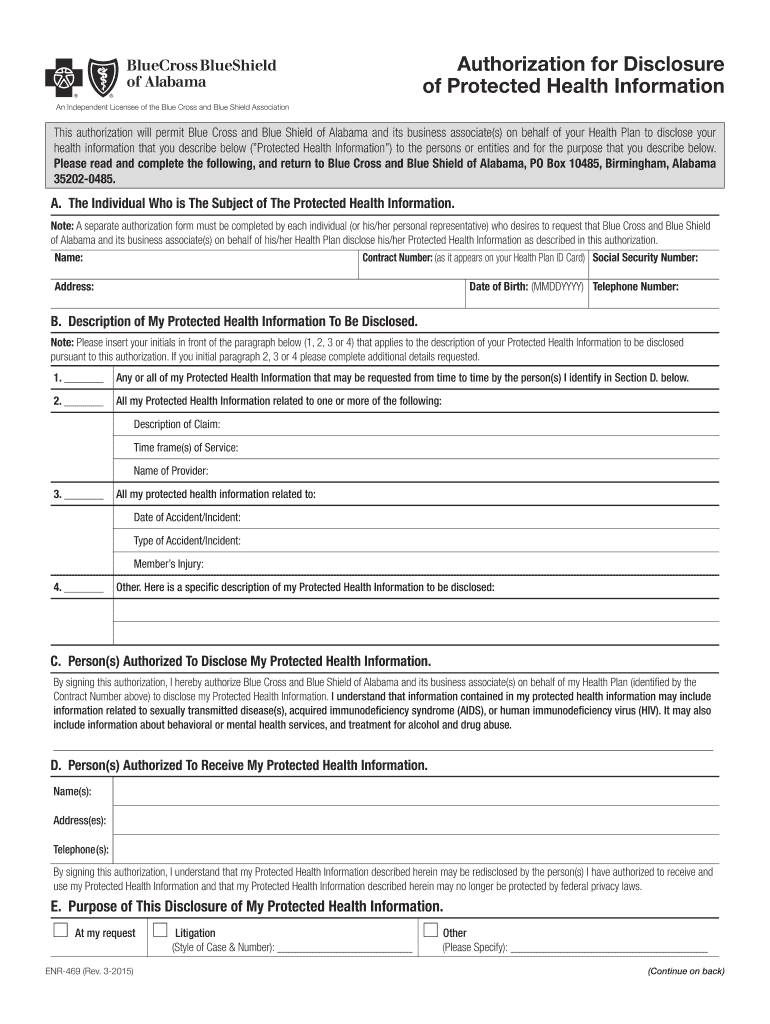
Paforms Alabama Com Fill Out and Sign Printable PDF Template signNow
Free Highmark Prior (Rx) Authorization Form PDF eForms
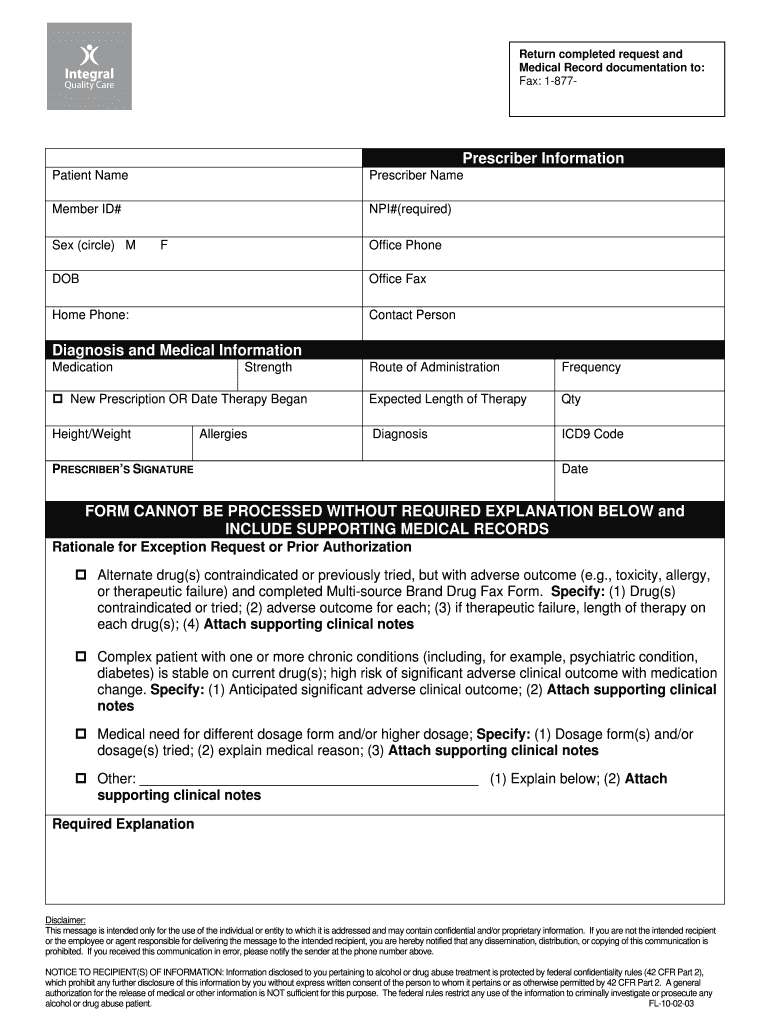
Pharmacy Coverage Request Fill Online, Printable, Fillable, Blank
Related Post: