Bcbs Fep Pharmacy Prior Authorization Form
Bcbs Fep Pharmacy Prior Authorization Form - If this is a compound claim, enter the national drug. Web most drugs are covered without requiring prior approval. Web prior approval pharmacy forms. Web 1 results found for search term : Web fep prior approval documents. Web to determine if medical authorization is required for a medicare member, please consult the prior authorization list or call blue shield of california provider services at (800). Blue cross and blue shield of texas (bcbstx) is continuing to make enhancements to its behavioral health (bh) prior. Prior authorization requests must be submitted electronically through the carefirst provider portal for all drugs requiring prior authorization. 9 30 23 hyaluronate compounding powder hydrocortisone cream, lotion, ointment 1%, 2.5%+ hydromorphone lorbrena hyftor. Web 2023 fep prior approval drug list rev. Web what to include with the completed prior approval form [pdf] member information. Web view procedures requiring prior approval below and submit medical authorization. View drugs in the fep medical prior authorization drug list and submit a drug authorization. However, some select drugs require your doctor to provide information about your prescription to determine coverage. On this page you'll find. Web fep prior approval documents. Please complete a separate claim form for each patient and each pharmacy. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. View and download our medical, pharmacy and overseas claim forms. Requested service (s) name and telephone number. Web the specific effective date will be noted for each change that is posted. Web most drugs are covered without requiring prior approval. Web what to include with the completed prior approval form [pdf] member information. Each claim form must be signed. Web 2023 fep prior approval drug list rev. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web your pharmacy coverage works outside the u.s., too*. Web 2023 fep prior approval drug list rev. Web the specific effective date will be noted for each change that is posted. *cvs caremark is. View drugs in the fep medical prior authorization drug list and submit a drug authorization. Prior authorization requests must be submitted electronically through the carefirst provider portal for all drugs requiring prior authorization. Michigan providers should attach the completed form to the. Requested service (s) name and telephone number of contact person. This page provides prior approval requirements, contact information,. View drugs in the fep medical prior authorization drug list and submit a drug authorization. Each claim form must be signed. Web what to include with the completed prior approval form [pdf] member information. Web starting in 2024, members with medicare part a and/or part b will be eligible to enroll in our new medicare part d drug plan that. Find what you need by. Michigan providers should attach the completed form to the. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Blue cross and blue shield of texas (bcbstx) is continuing to make enhancements to its behavioral health (bh) prior. Prior. Requested service (s) name and telephone number of contact person. Blue cross and blue shield of texas (bcbstx) is continuing to make enhancements to its behavioral health (bh) prior. Prevent you from accessing novologix, such as a power or internet outage, use one of the following methods to. If this is a compound claim, enter the national drug. Web medication. Web what to include with the completed prior approval form [pdf] member information. Find what you need by. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral. Web 1 results found for search term : Web view procedures requiring prior approval below and submit medical authorization. For more information about pharmacy prior approval and the required forms visit the prior approval page. Find what you need by. 9 30 23 hyaluronate compounding powder hydrocortisone cream, lotion, ointment 1%, 2.5%+ hydromorphone lorbrena hyftor. Find what you need by. Web most drugs are covered without requiring prior approval. *cvs caremark is an independent company that provides pharmacy benefit. Web prior approval pharmacy forms. Web medication authorization request forms for drugs covered under the medical benefit. Web 2023 fep prior approval drug list rev. View drugs in the fep medical prior authorization drug list and submit a drug authorization. Web the specific effective date will be noted for each change that is posted. View and download our medical, pharmacy and overseas claim forms. Web what to include with the completed prior approval form [pdf] member information. Prevent you from accessing novologix, such as a power or internet outage, use one of the following methods to. Web fep prior approval documents. If this is a compound claim, enter the national drug. 9 30 23 hyaluronate compounding powder hydrocortisone cream, lotion, ointment 1%, 2.5%+ hydromorphone lorbrena hyftor. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. This page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Each claim form must be signed. Web to determine if medical authorization is required for a medicare member, please consult the prior authorization list or call blue shield of california provider services at (800). Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral health (bh) preservice request and review process for. Please complete a separate claim form for each patient and each pharmacy.Bcbs Prior Auth Forms To Print Fill Online, Printable, Fillable
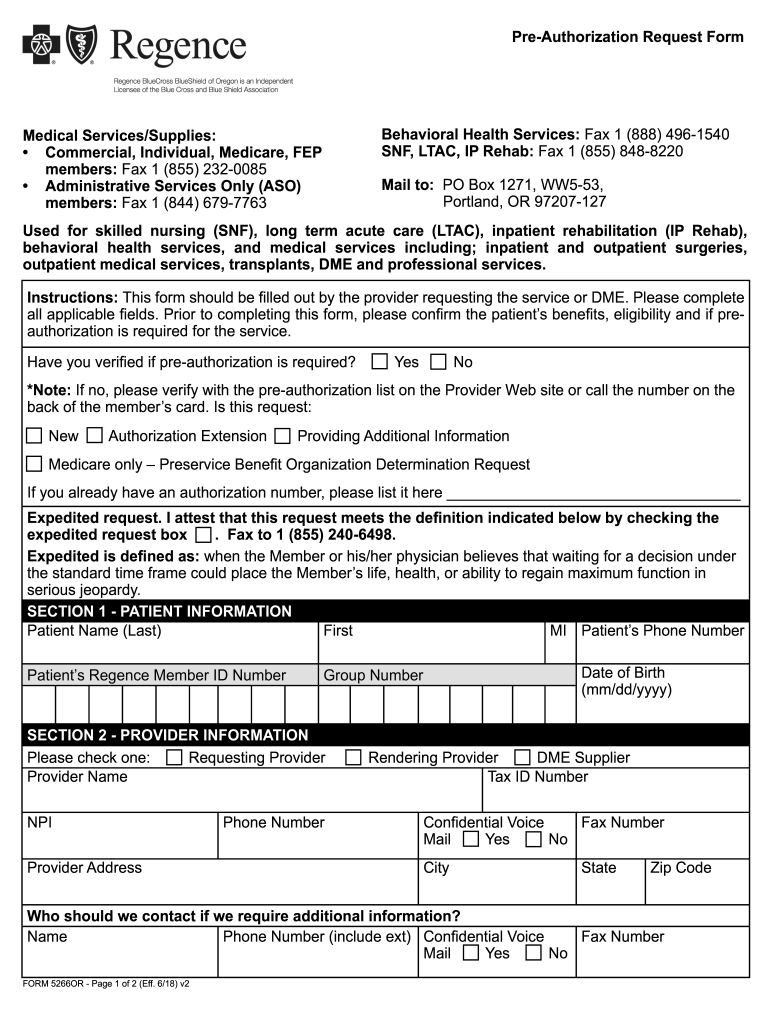
Regence preauthorization form Fill out & sign online DocHub
Bcbs Prior Authorization Form Form Resume Examples NRE34PV36x
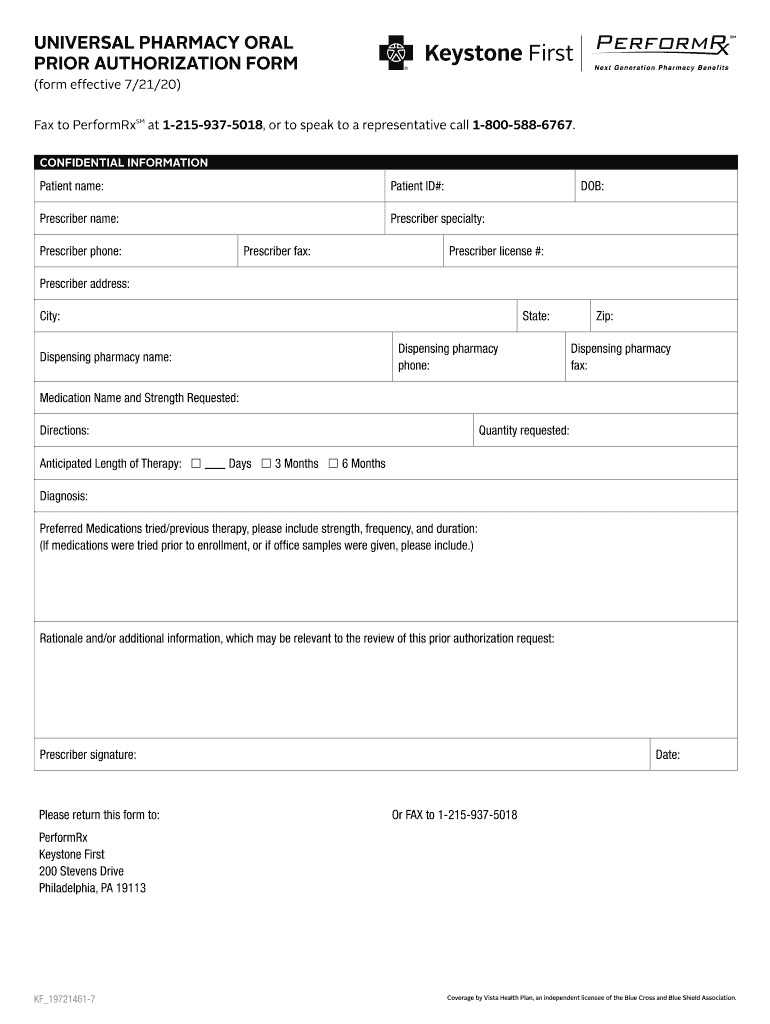
20202023 Keystone First Universal Pharmacy Oral Prior Authorization
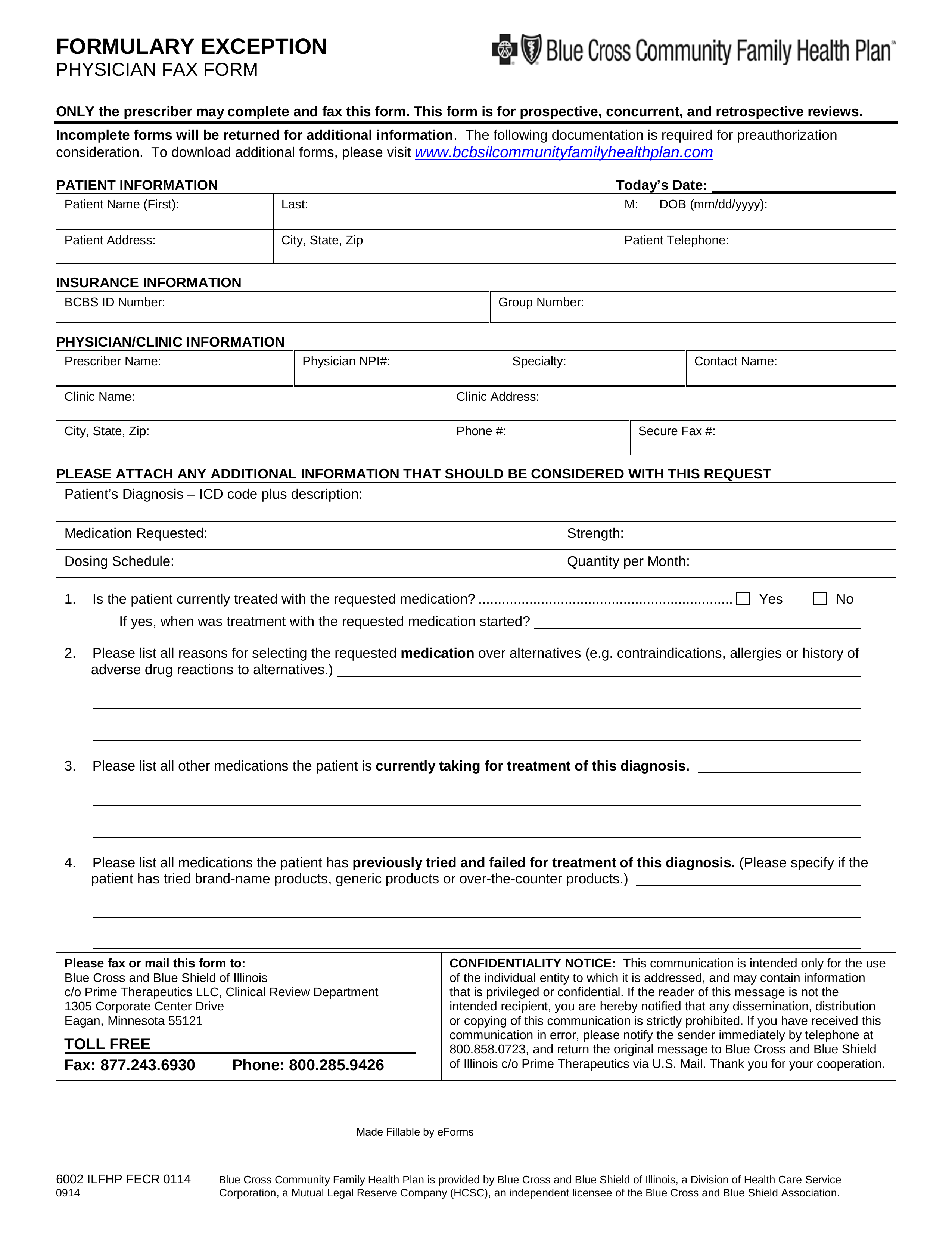
Prime Therapeutics Pharmacy Prior Authorization Form PharmacyWalls
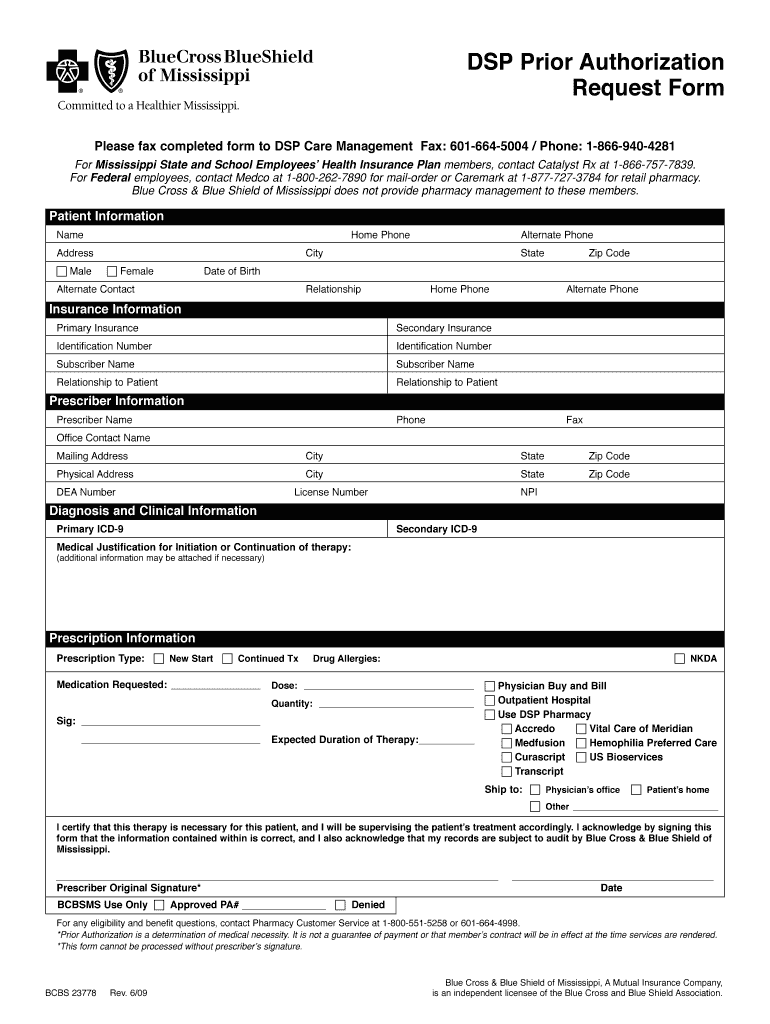
Bcbs Prior Authorization Form Pdf Fill Out and Sign Printable PDF
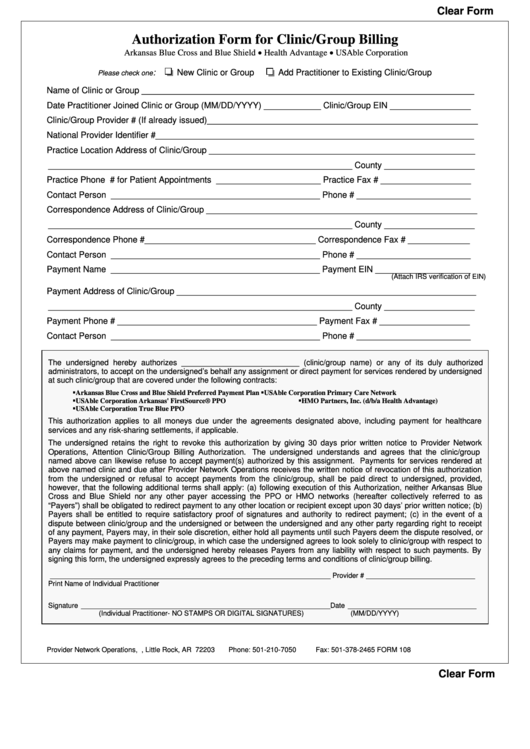
Fillable Bcbs Authorization Form For Clinic/group Billing printable pdf
Bcbs Prior Authorization Form Michigan Form Resume Examples kDp3Og030Q
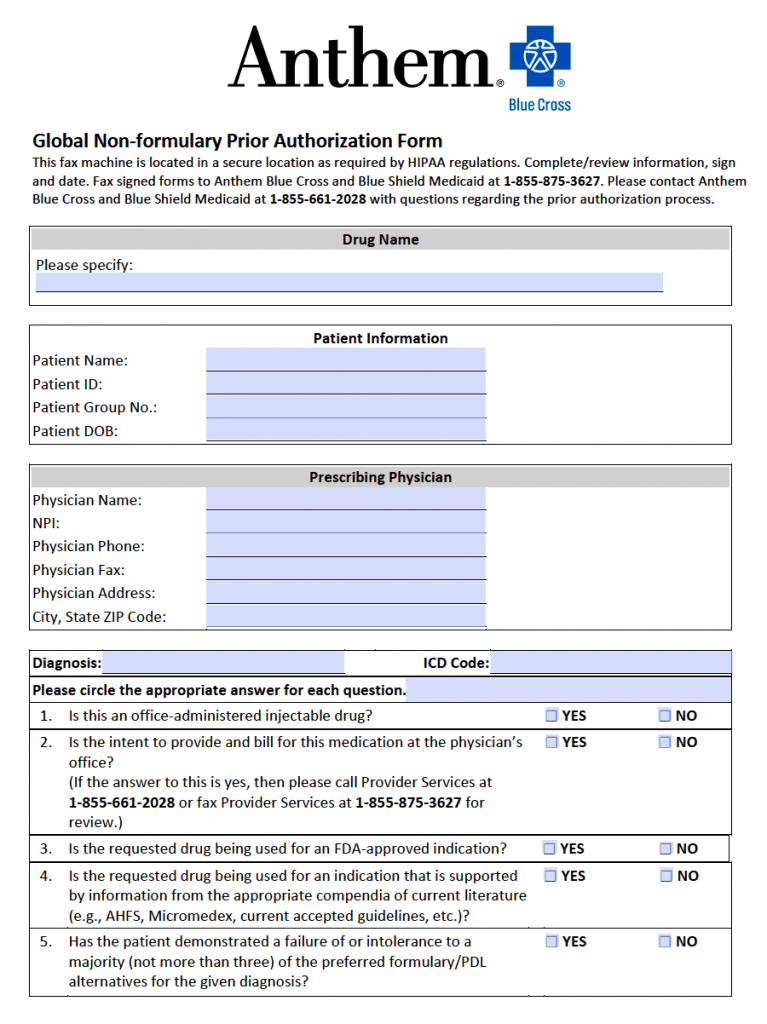
Free Anthem Blue Cross / Blue Shield Prior Prescription (Rx
Prime Therapeutics Pharmacy Prior Authorization Form PharmacyWalls
Related Post: