Availity Prior Authorization Form
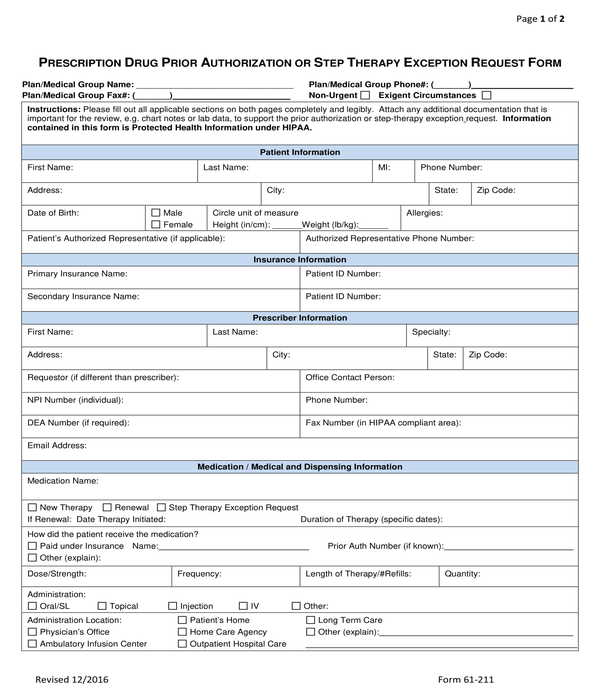
Availity Prior Authorization Form - Claims—professional and facility, even dental! Web the availity provider portal is now humana’s preferred method for medical and behavioral health providers to check eligibility and benefits, submit referrals and authorizations,. Upload clinical documents for previously submitted authorizations. Web form or electronic data interchange (edi) claim. Jacksonville, fla.—march 13, 2018— availity, the nation’s. Web * availity, llc is an independent company providing administrative support services on behalf of anthem blue cross and blue shield. Every day, health plans and providers are working to improve health. Web availity bridges this gap by making it easier for health plans and providers to collaborate and share data. A large part of the problem is the manual nature. Web the availity essentials portal provides access to all portal functions. Web the availity provider portal is now humana’s preferred method for medical and behavioral health providers to check eligibility and benefits, submit referrals and authorizations,. Web * availity, llc is an independent company providing administrative support services on behalf of anthem blue cross and blue shield. Web availity bridges this gap by making it easier for health plans and providers. A large part of the problem is the manual nature. Web effective december 1, 2020, prior authorization (pa) requirements will change for e0482. Availity ® provider portal to submit preservice prior authorization requests. First name last name business email phone company title state i am. Web prior authorization form premera prior authorizations now available on availity top 3 reminders for. Claims—professional and facility, even dental! Every day, health plans and providers are working to improve health. Web if you already have an availity essentials account and need support, please click login below and submit a ticket. Web the availity provider portal is now humana’s preferred method for medical and behavioral health providers to check eligibility and benefits, submit referrals and. This step confirms important details, including prior authorization. Claims—professional and facility, even dental! Web form or electronic data interchange (edi) claim. Web availity’s aligned with the healthcare industry’s goal of providing safe, timely and affordable patient care. Web prior authorization form premera prior authorizations now available on availity top 3 reminders for premera prior authorizations 1. Claims—professional and facility, even dental! Always check eligibility and benefits first through availity or your preferred web vendor. Form to support your request. Web prior authorizations and referrals. Every day, health plans and providers are working to improve health. Web prior authorization form premera prior authorizations now available on availity top 3 reminders for premera prior authorizations 1. Web there is a lot to do to fix the prior authorizations process, but availity's work with payers and their provider networks has started yielding results. Faxes and phone calls for these requests will no longer be. Claims—professional and facility, even. Web form or electronic data interchange (edi) claim. (24 hours a day, 7 days a week) or call availity client. Always check eligibility and benefits first through availity or your preferred web vendor. Web blue cross and blue shield of texas (bcbstx) is continuing to make enhancements to its behavioral health (bh) prior authorization review process for some. Jacksonville, fla.—march. Web the aetna provider portal on availity helps you spend less time on administration so you can focus more on patient care. Every day, health plans and providers are working to improve health. Web effective december 1, 2020, prior authorization (pa) requirements will change for e0482. Web the availity provider portal is now humana’s preferred method for medical and behavioral. Web the availity provider portal is now humana’s preferred method for medical and behavioral health providers to check eligibility and benefits, submit referrals and authorizations,. (24 hours a day, 7 days a week) or call availity client. Web 8.31.2023 by availity. Web the aetna provider portal on availity helps you spend less time on administration so you can focus more. The medical codes listed below will require pa by amerigroup community care. Web * availity, llc is an independent company providing administrative support services on behalf of anthem blue cross and blue shield. Submit your initial request on availity with the authorization (precertification) add. Web if you already have an availity essentials account and need support, please click login below. Jacksonville, fla.—march 13, 2018— availity, the nation’s. Web the aetna provider portal on availity helps you spend less time on administration so you can focus more on patient care. Web form or electronic data interchange (edi) claim. Form to support your request. Web how to register for the availity portal. Web fill out the form below to see how authorization services helps you manage prior authorizations. This step confirms important details, including prior authorization. (24 hours a day, 7 days a week) or call availity client. Web if you already have an availity essentials account and need support, please click login below and submit a ticket. Web availity bridges this gap by making it easier for health plans and providers to collaborate and share data. Web effective december 1, 2020, prior authorization (pa) requirements will change for e0482. Web * availity, llc is an independent company providing administrative support services on behalf of anthem blue cross and blue shield. Claims—professional and facility, even dental! A large part of the problem is the manual nature. Web the availity provider portal is now humana’s preferred method for medical and behavioral health providers to check eligibility and benefits, submit referrals and authorizations,. Submit your initial request on availity with the authorization (precertification) add. Blue cross and blue shield of texas (bcbstx) is excited to announce a convenient new way to submit claim reconsideration requests online for situational. Web there is a lot to do to fix the prior authorizations process, but availity's work with payers and their provider networks has started yielding results. Every day, health plans and providers are working to improve health. Web 8.31.2023 by availity.Free UnitedHealthcare Prior (Rx) Authorization Form PDF eForms
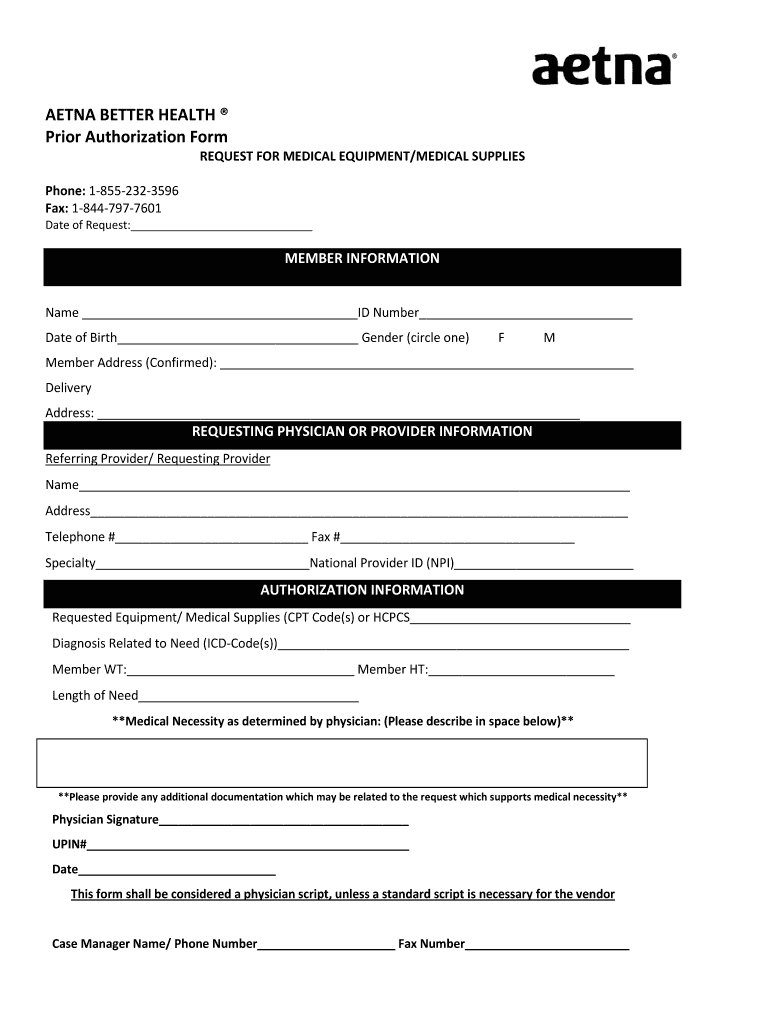
Aetna better health prior authorization form Fill out & sign online
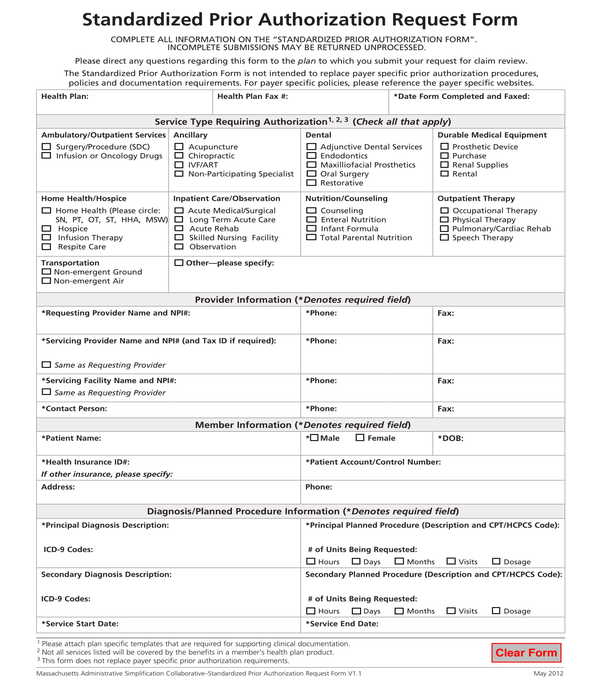
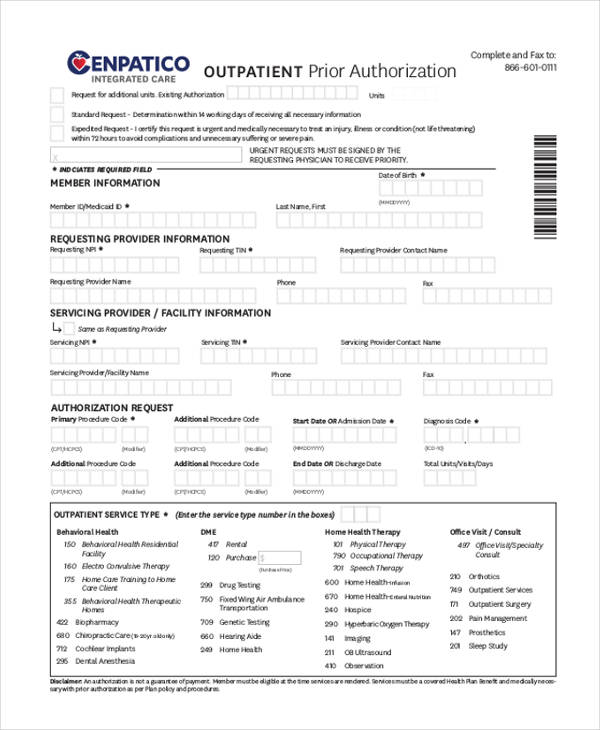
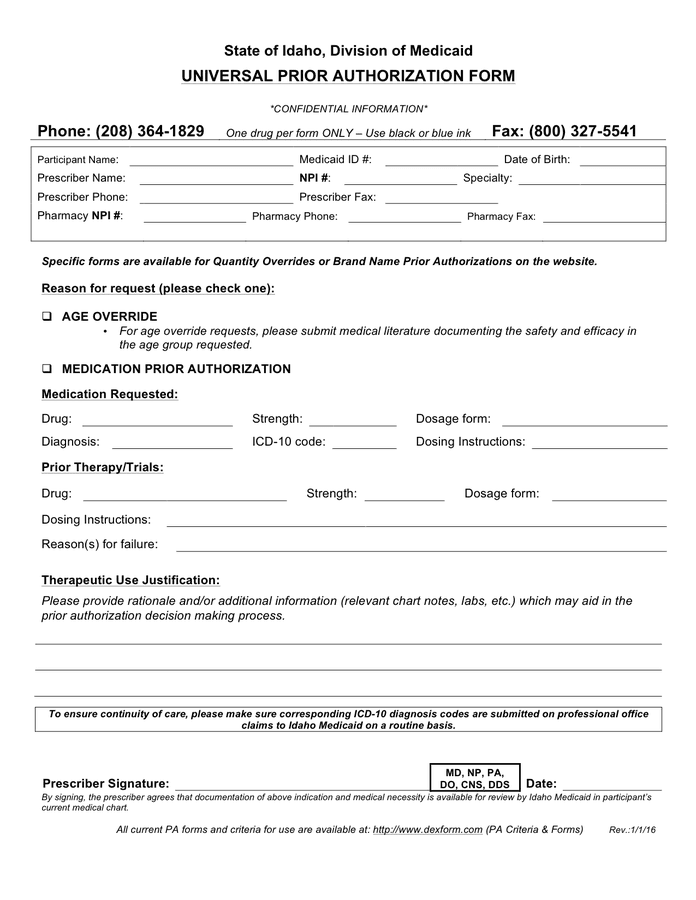
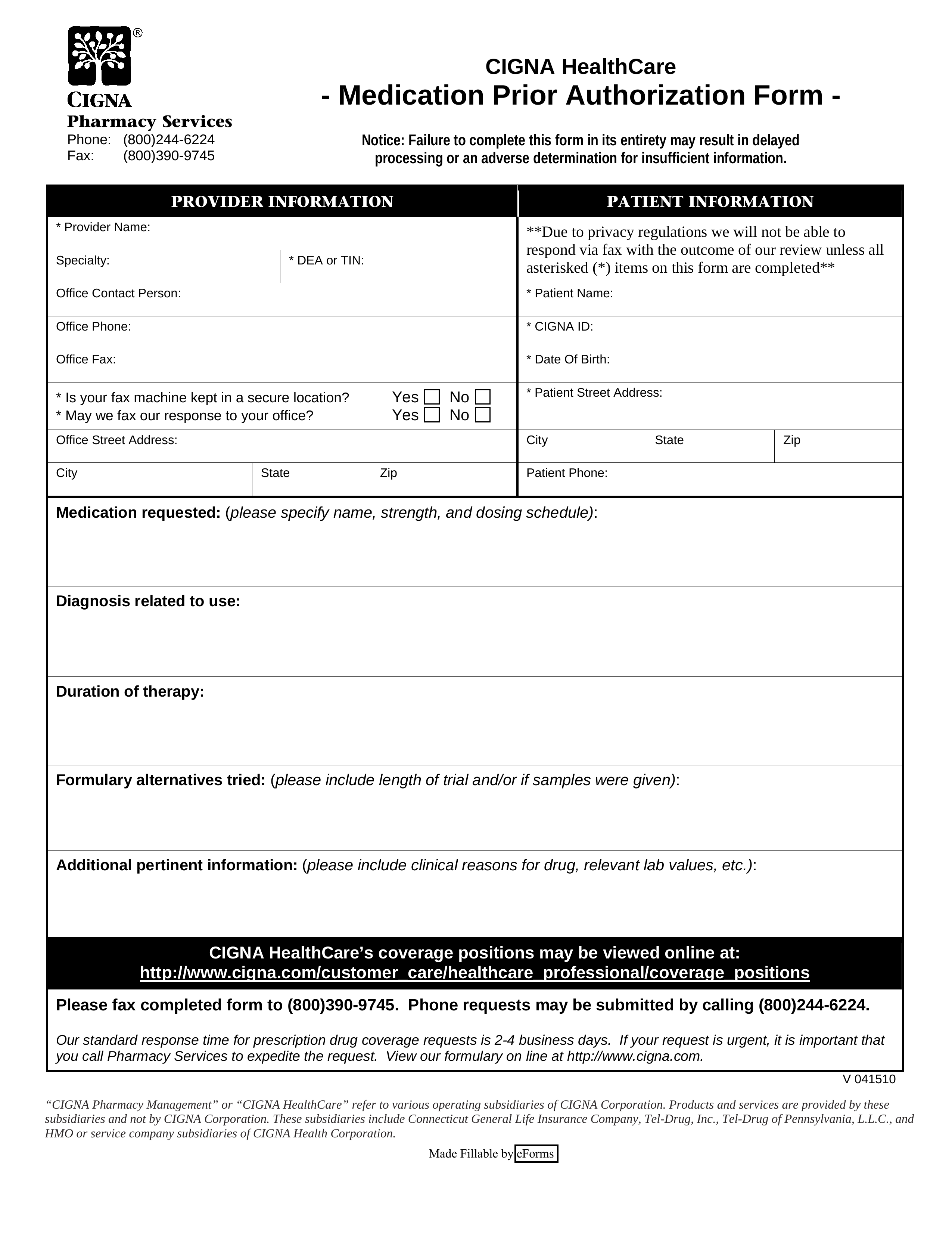
FREE 11+ Prior Authorization Forms in PDF MS Word
xray request form fill online printable fillable blank pdffiller x
FREE 11+ Prior Authorization Forms in PDF MS Word
Fill Free fillable Availity Providers PDF forms
FREE 11+ Prior Authorization Forms in PDF MS Word
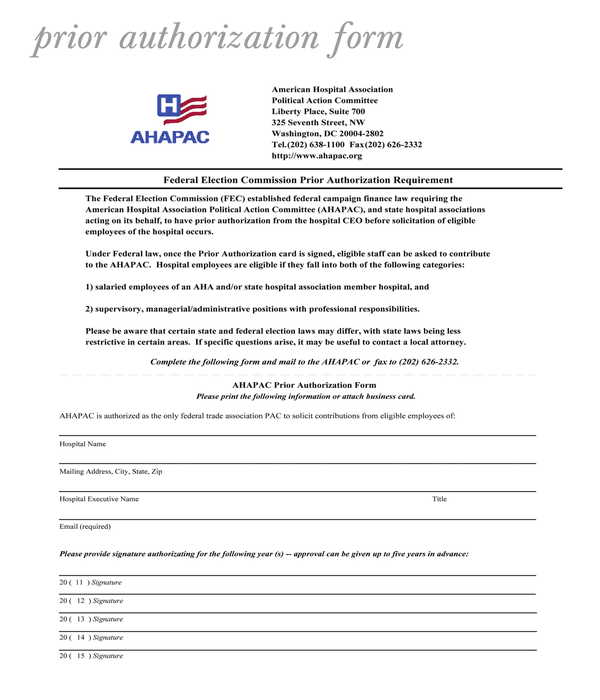
FREE 13+ Prior Authorization Forms in PDF MS Word
Universal prior authorization form in Word and Pdf formats
Free Cigna Prior (Rx) Authorization Form PDF eForms
Related Post: