Ascension Personalized Care Prior Authorization Form
Ascension Personalized Care Prior Authorization Form - Web medical specialty precertification/prior authorization request. View the status of an authorization by visiting the clinician portal. * to process request, all required fields with asterisks. Web effective january 1, 2022, the program will expand its prior authorization program to include hmo members in the state of texas to require prior authorization from nia. Fax a completed prior authorization form to: Web a prior authorization is an approval that a member must receive from their health plan before receiving certain treatment, medications or services. Web surgeons at ascension sites of care deliver leading surgical care that starts with working together on a personalized care plan. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. For standard (elective admission) requests, complete. Web authorization form expedited requests: Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Hours of operation are 8:00am to 8:00pm (et) monday to friday, excluding holidays. Web ascension personalized care health plans are easy to understand and use so you can focus on your health. Web authorization form expedited requests: * to process request, all required fields. Web ascension’s care management teams work in partnership with your doctors and multidisciplinary team members to better manage your medical, behavioral, and social. Ascension personalized care offers a variety of flexible, affordable aca health. Hours of operation are 8:00am to 8:00pm (et) monday to friday, excluding holidays. Web authorization is based on medical necessity determination and is not a guarantee. Web ascension personalized care health plans are easy to understand and use so you can focus on your health. Please verify eligibility and benefits prior to rendering services for all members. Web information on 24/7 care including virtual, mental health and our employee assistance plan (eap). Web ascension care teams start by understanding you, your health and your life to. The compassionate, personalized care you’ve come to expect is. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Web effective january 1, 2022, the program will expand its prior authorization program to include hmo members in the. Please verify eligibility and benefits prior to rendering services for all members. * to process request, all required fields with asterisks. Web information on 24/7 care including virtual, mental health and our employee assistance plan (eap). Web ascension care teams start by understanding you, your health and your life to deliver care that’s right for you. Web authorization is based. Web medical specialty precertification/prior authorization request. Web ascension care teams start by understanding you, your health and your life to deliver care that’s right for you. The compassionate, personalized care you’ve come to expect is. View the status of an authorization by visiting the clinician portal. Hours of operation are 8:00am to 8:00pm (et) monday to friday, excluding holidays. Web effective january 1, 2022, the program will expand its prior authorization program to include hmo members in the state of texas to require prior authorization from nia. * to process request, all required fields with asterisks. Web a prior authorization is an approval that a member must receive from their health plan before receiving certain treatment, medications or services.. * to process request, all required fields with asterisks. Please submit all inquiries for prior authorization requests via the eqsuite® provider portal at. Please verify eligibility and benefits prior to rendering services for all members. Web ascension care teams start by understanding you, your health and your life to deliver care that’s right for you. The compassionate, personalized care you’ve. * to process request, all required fields with asterisks. Web ascension care teams start by understanding you, your health and your life to deliver care that’s right for you. Submit prior authorization by fax: Hours of operation are 8:00am to 8:00pm (et) monday to friday, excluding holidays. This means that our website. Submit prior authorization by fax: Hours of operation are 8:00am to 8:00pm (et) monday to friday, excluding holidays. Ascension personalized care offers a variety of flexible, affordable aca health. Web effective january 1st, 2021, prior authorization will be required for the following services: Web medical specialty precertification/prior authorization request. Submit prior authorization by fax: Fax a completed prior authorization form to: Web ascension personalized care health plans are easy to understand and use so you can focus on your health. Please verify eligibility and benefits prior to rendering services for all members. The compassionate, personalized care you’ve come to expect is. View the status of an authorization by visiting the clinician portal. Ascension personalized care offers a variety of flexible, affordable aca health. For standard (elective admission) requests, complete. Web physical therapy available in different settings. Web effective january 1, 2022, the program will expand its prior authorization program to include hmo members in the state of texas to require prior authorization from nia. Web medical specialty precertification/prior authorization request. Web a prior authorization is an approval that a member must receive from their health plan before receiving certain treatment, medications or services. Web information on 24/7 care including virtual, mental health and our employee assistance plan (eap). Web clinicians can submit requests: Web a new name for ascension complete. Web authorization form expedited requests: This means that our website. Hours of operation are 8:00am to 8:00pm (et) monday to friday, excluding holidays. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage.Banner Aetna Prior Authorization Form Fill Out and Sign Printable PDF
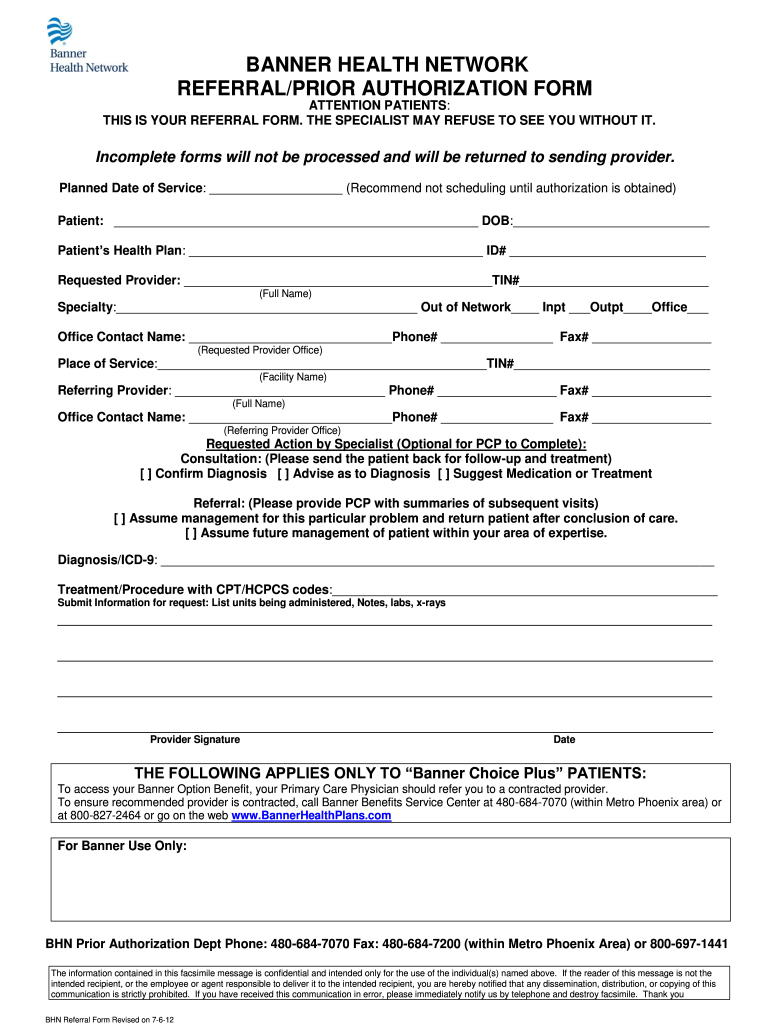
FREE 11+ Prior Authorization Forms in PDF MS Word
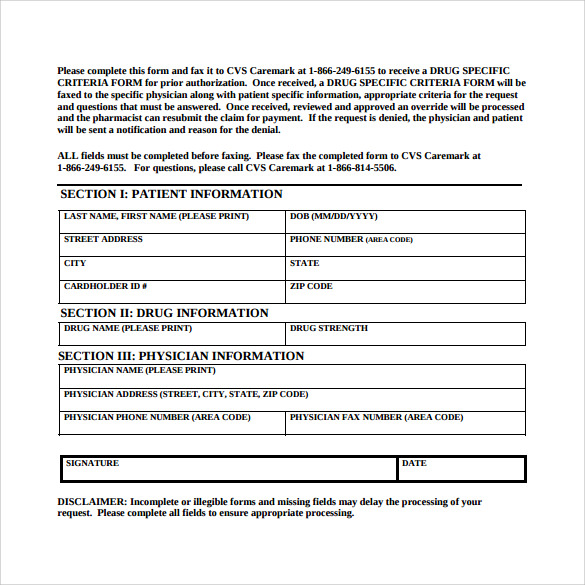
9+ Sample Caremark Prior Authorization Forms Sample Templates
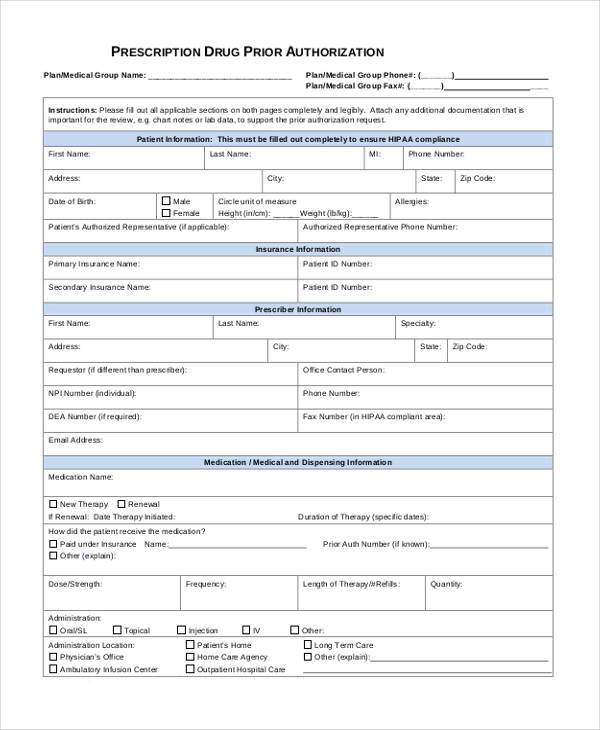
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
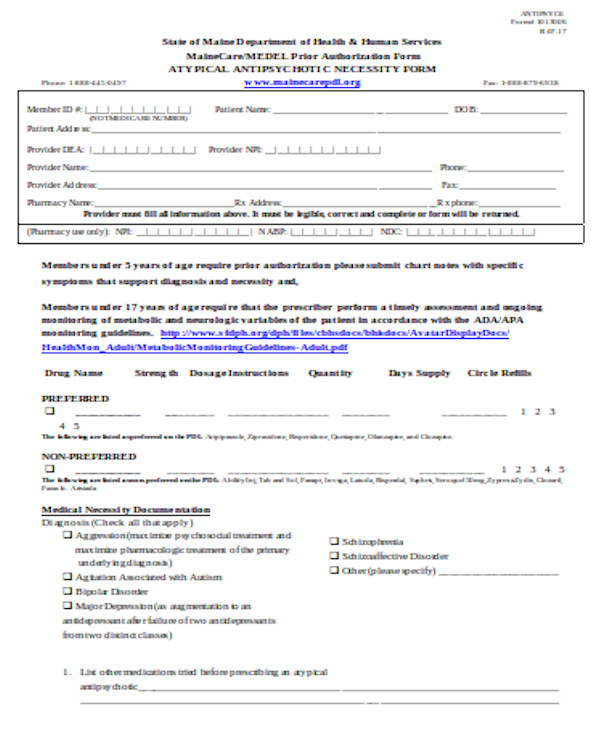
FREE 13+ Prior Authorization Forms in PDF MS Word
Medicare Part D Medco Prior Authorization Form Printable
wellcare prior authorization form Fill out & sign online DocHub
Prior Authorization Form Template Classles Democracy
Fillable Online Ascension Personalized Care SelfReimbursement Claim
Blue Cross Managed Care Prior Authorization Form Form Resume
Related Post: