Amerigroup Authorization Form
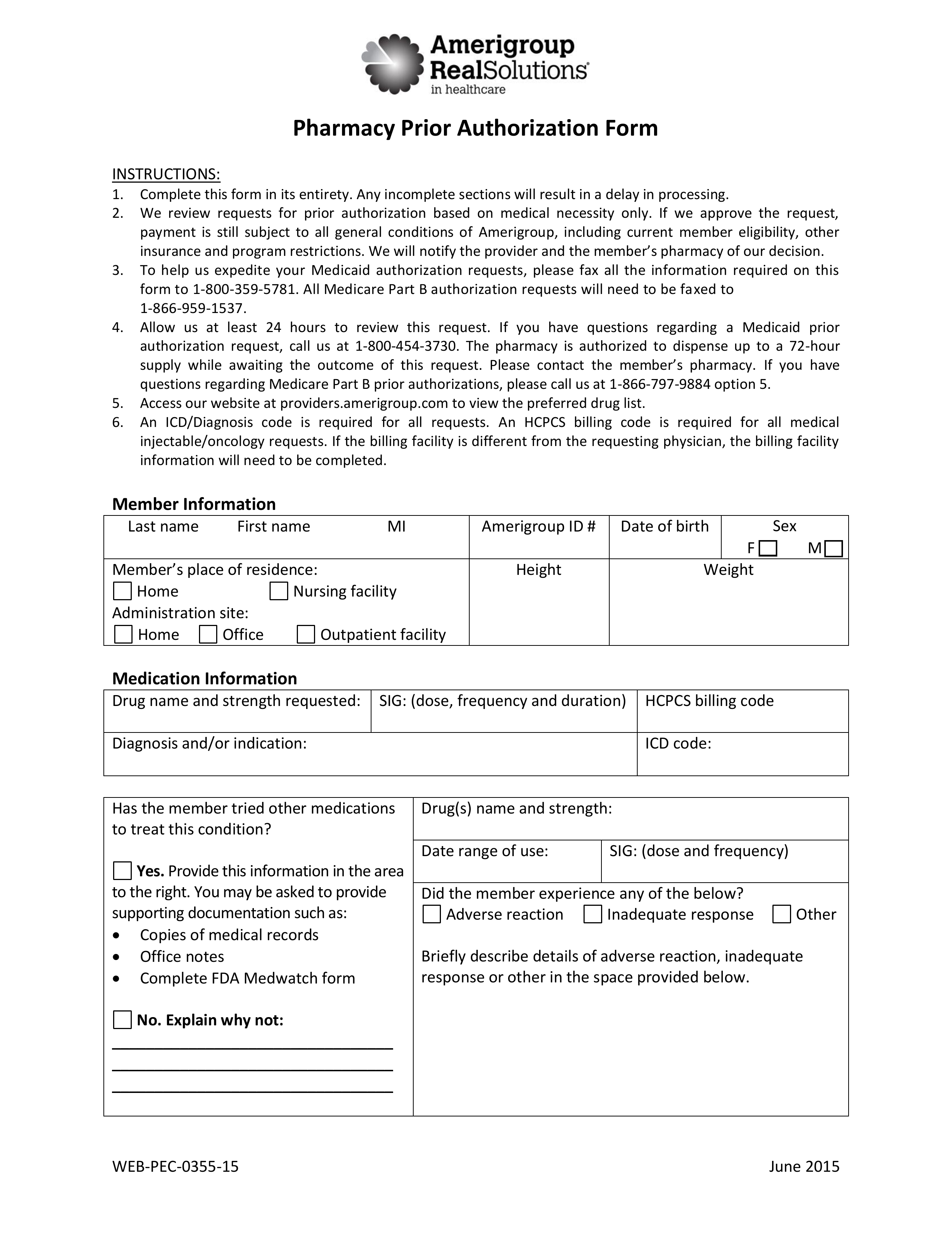
Amerigroup Authorization Form - Ad uslegalforms.com has been visited by 100k+ users in the past month There’s no more critical person on this team than you, the provider. Improving the patient experience cme; Web prior authorization lookup tool ; You’ll still get the same comprehensive care and. Web prior authorization request form. Clinical requirements — qualifies for. To prevent delay in processing your request, please fill out form in its entirety with. If you prefer to fax, please utilize the forms listed. Providing care for those who need it most requires a team effort. An amerigroup prior authorization form is the document that should be used by patients insured by amerigroup in order to receive approval for the. Improving the patient experience cme; Amerigroup, iowa total care subject: If you have any questions, please feel free to call us at the customer service number on your member identification. Providers may use the amerigroup prior. 18009643627 form promptly and with excellent accuracy. Web here to help you. To prevent delay in processing your request, please fill out form in its entirety with. Providing care for those who need it most requires a team effort. Member eligibility & pharmacy overview ; Web amerigroup is becoming wellpoint in select markets (az, ia, nj, tn, tx, and wa). This new name won’t impact your coverage. 18009643627 form promptly and with excellent accuracy. Financial requirements — including monthly income and assets. If you prefer to fax, please utilize the forms listed. Ad pdffiller.com has been visited by 1m+ users in the past month Web prior authorization lookup tool ; Specified event or time frame: Web here to help you. There’s no more critical person on this team than you, the provider. Ad uslegalforms.com has been visited by 100k+ users in the past month This new name won’t impact your coverage. Web instructions for completing the member authorization form. Providing care for those who need it most requires a team effort. Sign and mail this form to: Providing care for those who need it most requires a team effort. Web prior authorization lookup tool ; Learn more about financial eligibility. To prevent any delays in processing your request, please. Customer services for medicare prescription drug plans (part d). Provider manual and guides ; Web here to help you. To prevent delay in processing your request, please fill out form in its entirety with. Improving the patient experience cme; Web amerigroup nonemergency ambulance prior authorization request for physical health/medical services, submit completed form by fax to: Provider manual and guides ; There’s no more critical person on this team than you, the provider. This new name won’t impact your coverage. Web here to help you. Web * availity, llc is an independent company providing administrative support services on behalf of amerigroup community care. Web amerigroup is becoming wellpoint in select markets (az, ia, nj, tn, tx, and wa). 18009643627 form promptly and with excellent accuracy. Sign and mail this form to: This new name won’t impact your coverage. If you have any questions, please feel free to call us at the customer service number on your member identification. Web before you get certain services, you may need a referral or prior authorization. To prevent any delays in processing your request, please. Looking for a form, but don’t see it here? If you have any questions, please feel free to call us at the customer service number on your member identification. Addiional codes will be provided on supplemental informaion. Looking for a form but don’t see it here? Looking for a form, but don’t see it here? An amerigroup prior authorization form is the document that should be used by patients insured by amerigroup in order to receive approval for the. Web amerigroup nonemergency ambulance prior authorization request for physical health/medical services, submit completed form by fax to: 18009643627 form promptly and with excellent accuracy. To get a referral or prior authorization, talk to your primary care provider (pcp). Web before you get certain services, you may need a referral or prior authorization. Learn more about financial eligibility. Web prior authorization is not required for physician evaluation and management services for members of the amerigroup amerivantage (medicare advantage). To prevent delay in processing your request, please fill out form in its entirety with. If you have any questions, please feel free to call us at the customer service number on your member identification. You’ll still get the same comprehensive care and. Web mltss is for individuals who meet: Provider manual and guides ; Web here to help you. Web up to $40 cash back amerigroup auth req form typically needs to be filed by healthcare providers, such as doctors, hospitals, and other medical professionals. Financial requirements — including monthly income and assets. Web prior authorization request form. Web updated june 02, 2022. Amerigroup, iowa total care subject:Free Amerigroup Prior (Rx) Authorization Form PDF eForms
Amerigroup Medicare Advantage Prior Authorization Forms Form Resume
Fillable Online Amerigroup Prior Authorization Request Form. Amerigroup
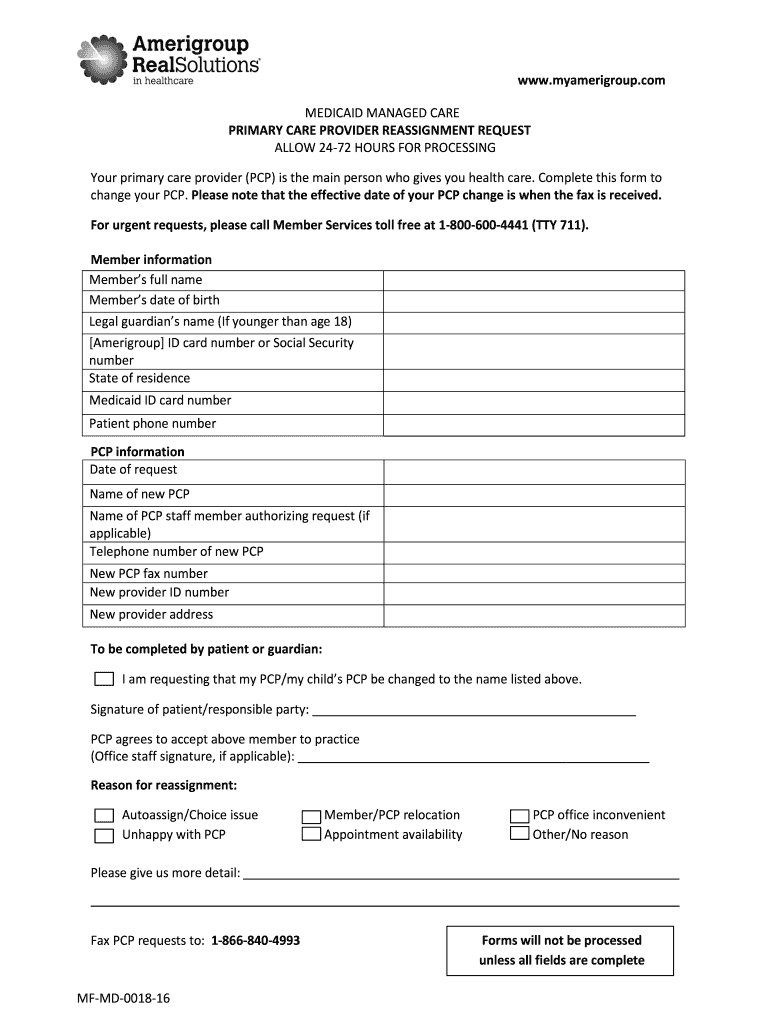
Amerigroup Pcp Change Form Fill and Sign Printable Template Online
Amerigroup Authorization Request PDF Form FormsPal
Amerigroup Nj Prior Authorization Form Form Resume Examples EY39YQGn32
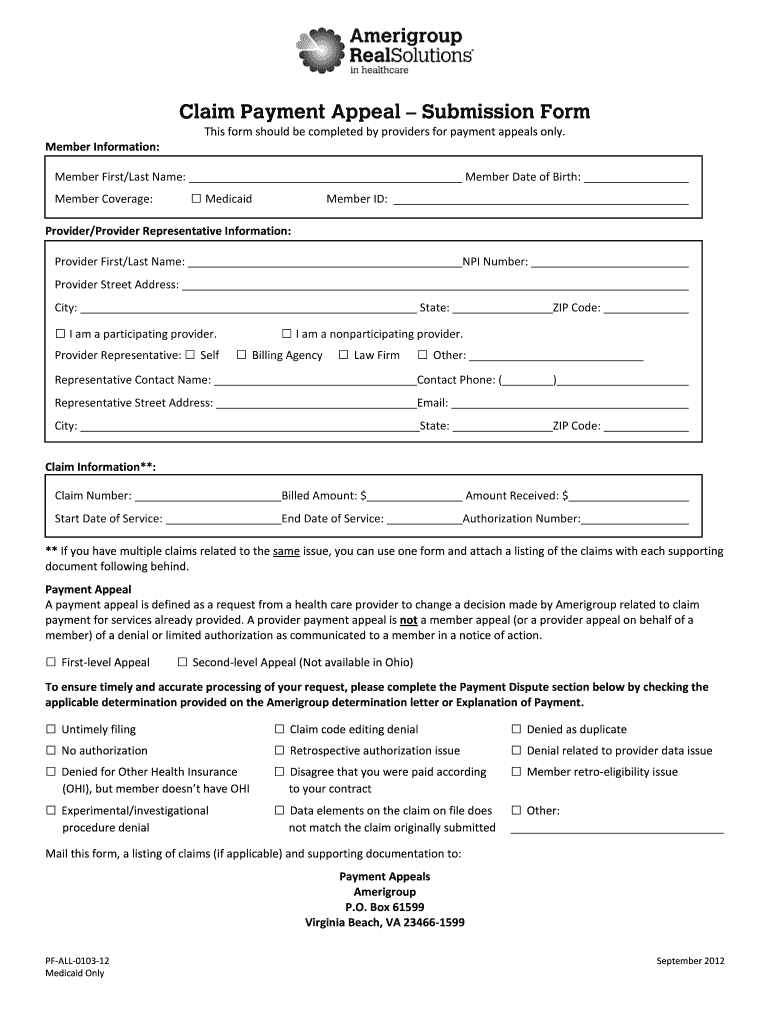
Amerigroup Appeal Form Fill Out and Sign Printable PDF Template signNow
Kansas amerigroup formulary
Amerigroup TXPEC154515 20162021 Fill and Sign Printable Template
Covermymeds Humana Prior Auth Form / Amerigroup Prior Authorization
Related Post: