Aetna Prior Authorization Form For Prolia
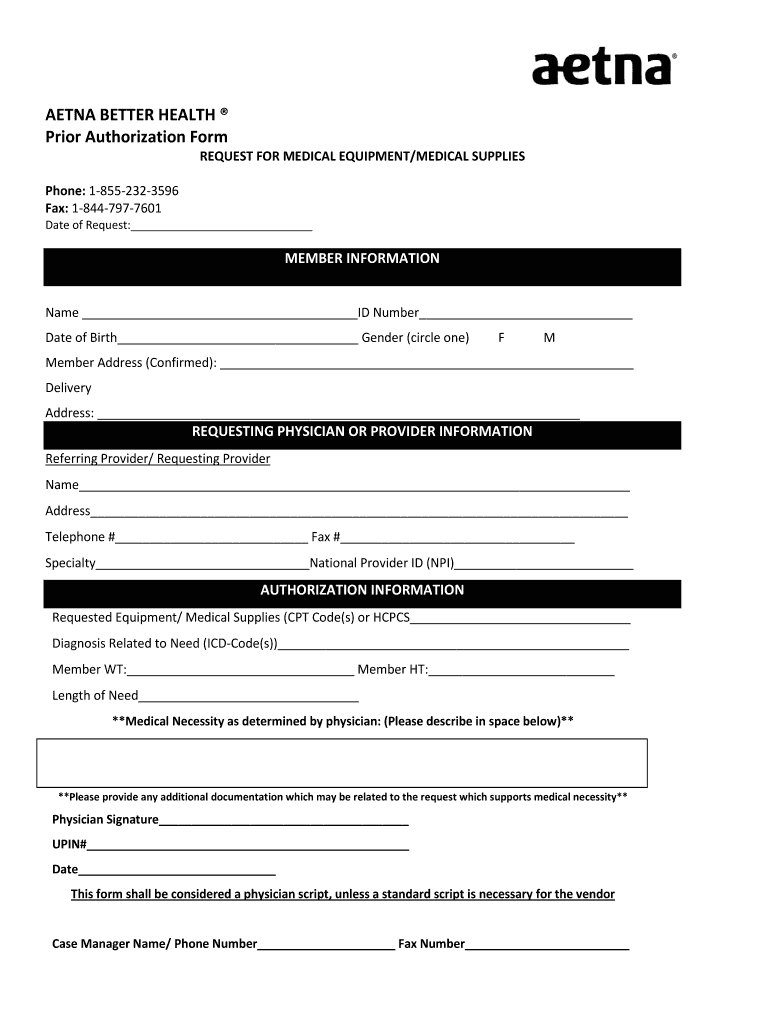
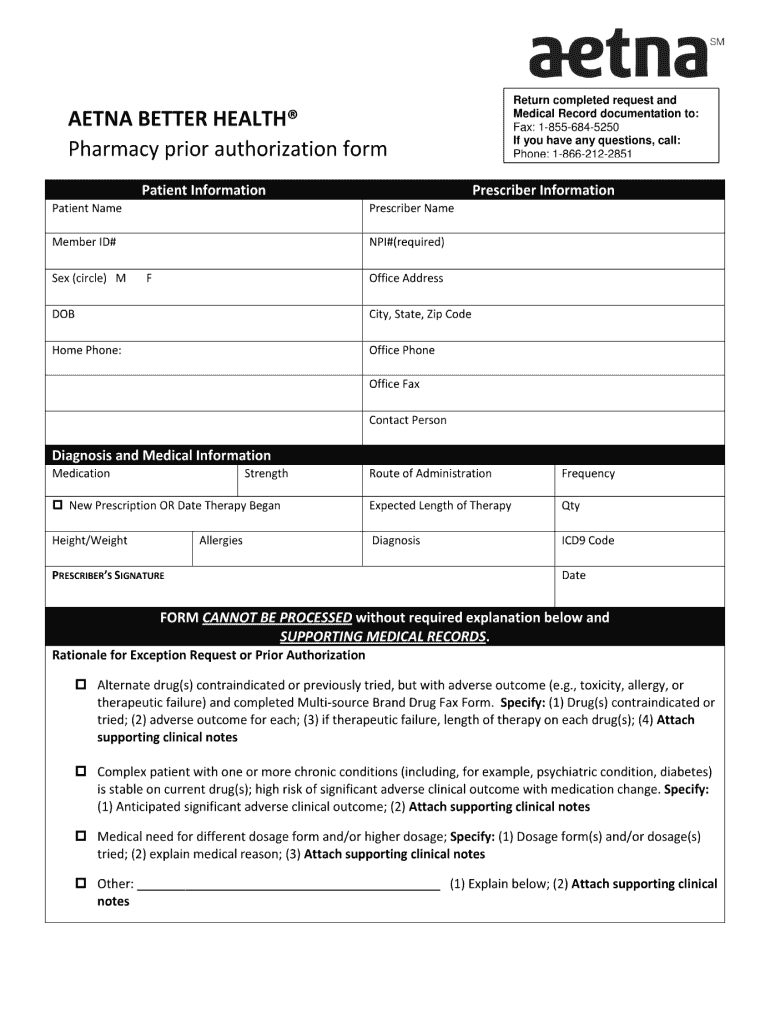
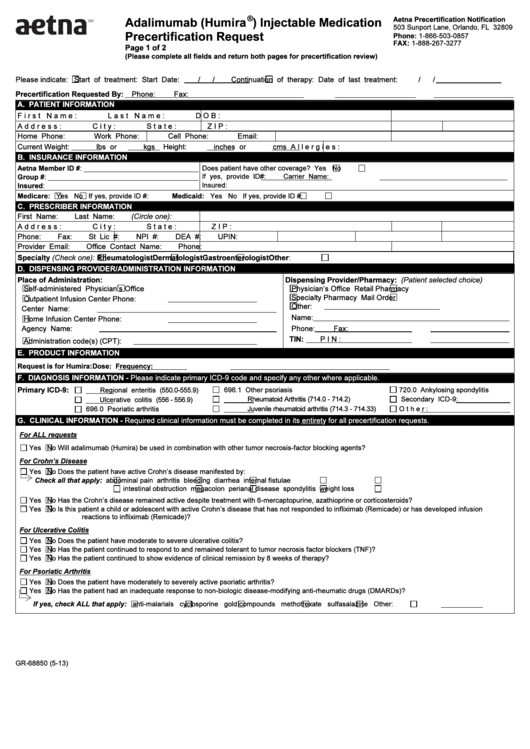
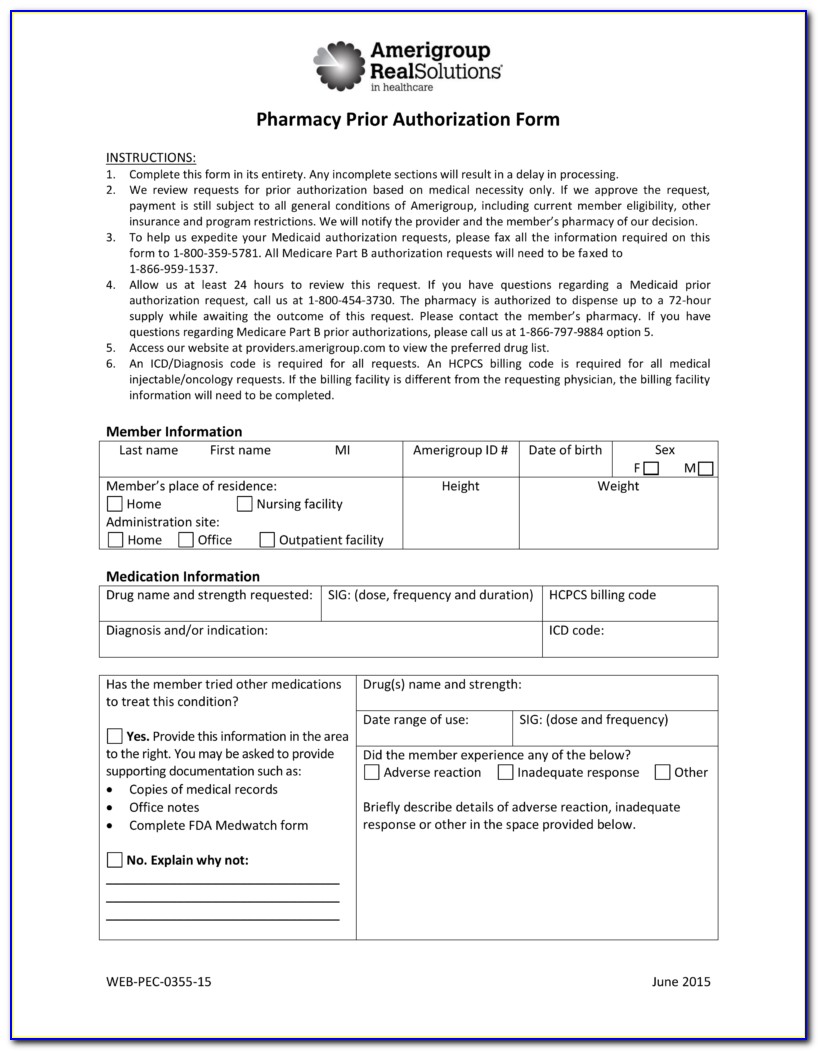
Aetna Prior Authorization Form For Prolia - Click on the get form. Ad find product information by visiting the official product site. This process is called prior authorization or preapproval. Use get form or simply click on the template preview to open it in the editor. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. Web get information about aetna’s precertification requirements, including precertification lists and criteria for patient insurance preauthorization. Web submit your initial request on availity with the authorization (precertification) add transaction. Ad find product information by visiting the official product site. Web execute aetna prior authorization form within a few minutes following the instructions below: Prolia is proven to treat patients at high risk for fracture receiving adjuvant aromatase inhibitor therapy for breast cancer. Web find documents and resources for patients with osteoporosis at high risk for fracture currently on treatment with prolia® (denosumab). Web submit your initial request on availity with the authorization (precertification) add transaction. Prolia is proven to treat patients at high risk for fracture receiving adjuvant aromatase inhibitor therapy for breast cancer. Ad find product information by visiting the official. Web (prior authorization needed for the drug and site of care): Ad find product information by visiting the official product site. Web insurance verification and prior authorization form insurance verification and prior authorization form fax with copies of insurance card(s), front and back, to amgen. Web aetna specialty precertification forms abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab. Use get form or simply click on the template preview to open it in the editor. Web what is prior authorization? This process is called prior authorization or preapproval. Web get information about aetna’s precertification requirements, including precertification lists and criteria for patient insurance preauthorization. Some care will require your doctor to get our approval first. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. Web find documents and resources for patients with osteoporosis at high risk for fracture currently on treatment with prolia® (denosumab). Ad find product information by visiting the official product site. Web specialty medication precertification request. See full prescribing & safety info. Web o authorization is for no more than 12 months. Web specialty medication precertification request please indicate: To submit a request, call our precertification. Web what is prior authorization? Web find documents and resources for patients with osteoporosis at high risk for fracture currently on treatment with prolia® (denosumab). Click on the get form. Find answers to frequently asked questions. Web prolia (denosumab) physician information patient information * physician name: Web 93 % of medicare part b patients have access to prolia® as initial therapy 1, * ,† no. Web prolia (denosumab) physician information patient information * physician name: Find the template you want in the collection of legal forms. Web execute aetna prior authorization form within a few minutes following the instructions below: This process is called prior authorization or preapproval. For statement of medical necessity (smn) precertification forms, see specialty. Web specialty medication precertification request please indicate: Click on the get form. *due to privacy regulations w e will not be able to respond via fax with the. Web execute aetna prior authorization form within a few minutes following the instructions below: For statement of medical necessity (smn) precertification forms, see specialty. Then complete a short questionnaire, if asked, to give us more clinical. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web medication precertification request page 1 of 3 phone: Web prolia (denosumab) physician information patient information * physician name: Web find documents and resources for patients with osteoporosis at high risk for. Then complete a short questionnaire, if asked, to give us more clinical. Find answers to frequently asked questions. Web 93 % of medicare part b patients have access to prolia® as initial therapy 1, * ,† no step edit required no prior authorization required 73 % of medicare part b patients pay $ 0. Click on the get form. Specialty. See full prescribing & safety info. Find answers to frequently asked questions. Click on the get form. Find answers to frequently asked questions. Some care will require your doctor to get our approval first. Web insurance verification and prior authorization form insurance verification and prior authorization form fax with copies of insurance card(s), front and back, to amgen. Web what is prior authorization? Web find documents and resources for patients with osteoporosis at high risk for fracture currently on treatment with prolia® (denosumab). Use get form or simply click on the template preview to open it in the editor. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web prolia (denosumab) physician information patient information * physician name: Find the template you want in the collection of legal forms. In these cases, your doctor can submit a request on your behalf to get that. Web specialty medication precertification request please indicate: Then complete a short questionnaire, if asked, to give us more clinical. Prolia is proven to treat patients at high risk for fracture receiving adjuvant aromatase inhibitor therapy for breast cancer. Web execute aetna prior authorization form within a few minutes following the instructions below: To submit a request, call our precertification. Web medication precertification request page 1 of 3 phone: This process is called prior authorization or preapproval.Aetna better health prior authorization form Fill out & sign online
Aetna dmo referral form Fill out & sign online DocHub
Fill Free fillable Aetna Better Health PDF forms
Aetna blank prior authorization forms Fill out & sign online DocHub
Top 6 Aetna Prior Authorization Form Templates free to download in PDF
Aetna Medicare Medication Prior Authorization Form Form Resume
Aetna Viscosupplementation Form 2022 Fill Online, Printable, Fillable
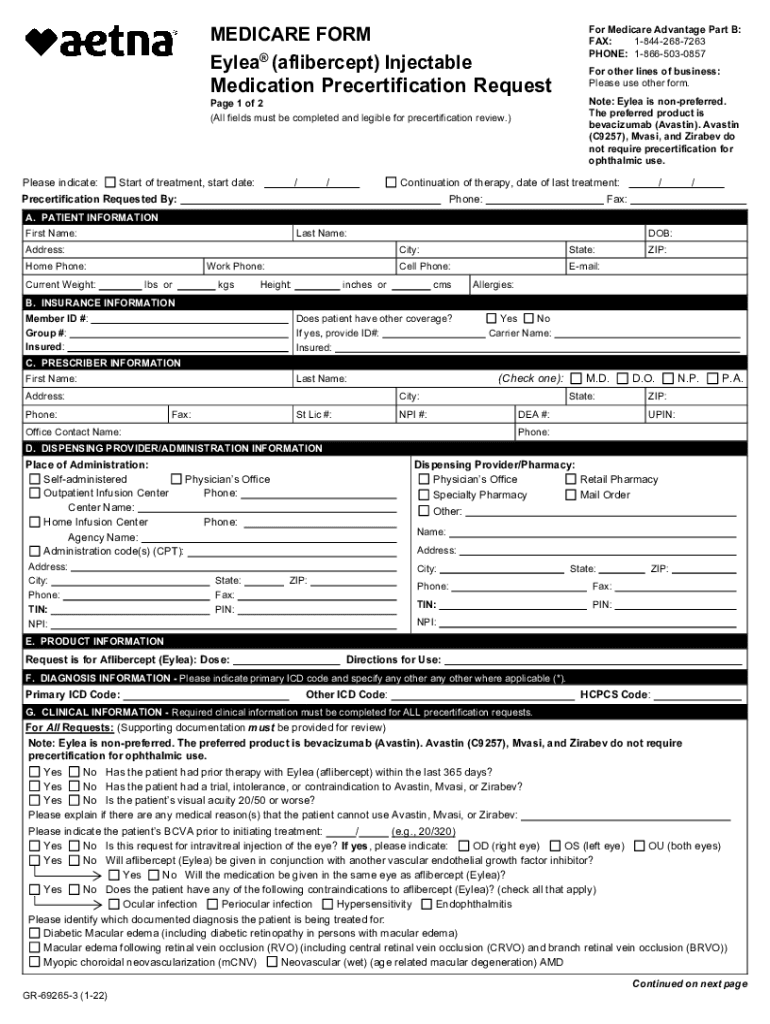
Aetna eylea prior authorization form Fill out & sign online DocHub
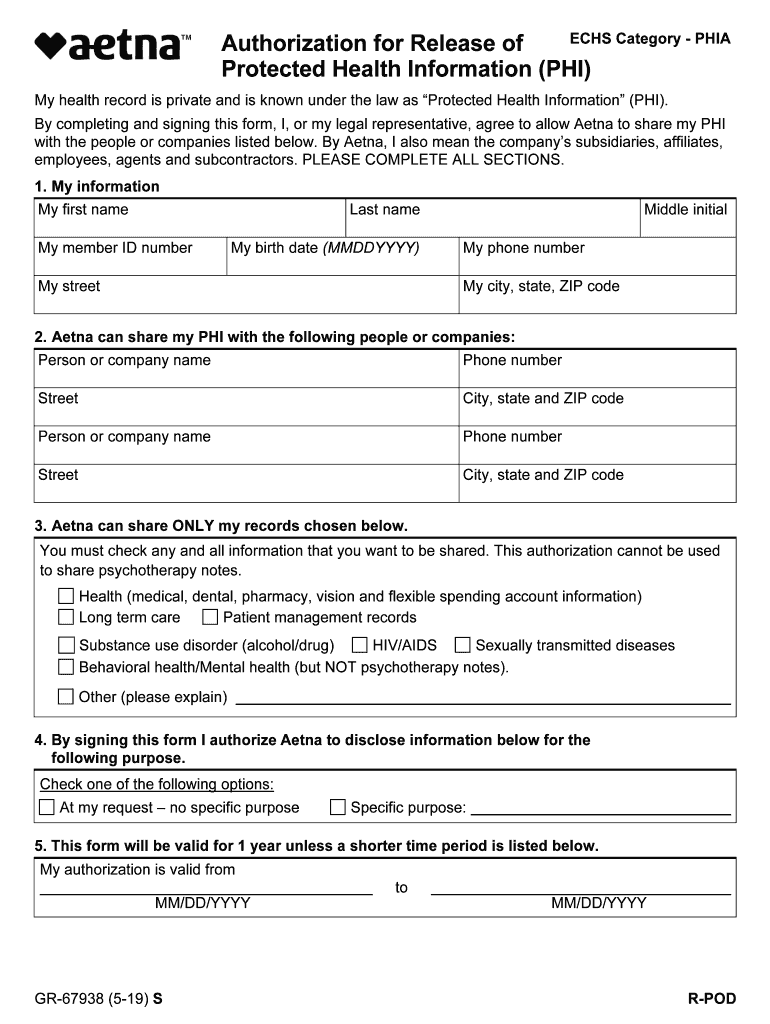
20192023 Form Aetna GR67938 SFill Online, Printable, Fillable, Blank
Aetna better health application Fill out & sign online DocHub
Related Post: