Aetna Botox Prior Authorization Form
Aetna Botox Prior Authorization Form - Prior authorization criteria is available. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. For medicare advantage part b: The services that need prior authorization. Web online you can ask for pa through our secure provider portal. Download and fill out the form with the required information and fax it to the number. Aetna specialty precertification forms abatacept (orencia ® ) precertification request form (pdf,. Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Web the basics of prior authorization. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. Aetna specialty precertification forms abatacept (orencia ® ) precertification request form (pdf,. In these cases, your doctor can submit a request on your behalf to get that. Web online you can ask for pa through our secure provider portal. Web medicare form botulinum toxins injectable medication precertification request page 2 of 3 (all fields must be completed and legible for. Web attach supporting documentation if covered services and those requiring prior authorization change, we will notify you at least 60 days in advance via the provider. Pharmacy specialty drug prior authorization. Aetna specialty precertification forms abatacept (orencia ® ) precertification request form (pdf,. Please use medicare request form fax: By fax download our pa. Prior authorization criteria is available. The services that need prior authorization. Start date / / aetna precertification. Web find the documents and forms you need to request specialty medications. Pharmacy specialty drug prior authorization. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. Download and fill out the form with the required information and fax it to the number. Participating providers can now check for codes that require prior. Web online you can ask for pa through our. Please use medicare request form fax: Download and fill out the form with the required information and fax it to the number. Check out this section to learn what it is and why it’s important. By fax download our pa. Pharmacy specialty drug prior authorization. Check out this section to learn what it is and why it’s important. Web medicare form botulinum toxins injectable medication precertification request page 2 of 3 (all fields must be completed and legible for precertification review.) for medicare. Please use medicare request form fax: Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible. Web the basics of prior authorization. Pharmacy specialty drug prior authorization. Continued on next page botox® (onabotulinumtoxina). In these cases, your doctor can submit a request on your behalf to get that. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. By fax download our pa. Web the basics of prior authorization. Download and fill out the form with the required information and fax it to the number. Web attach supporting documentation if covered services and those requiring prior authorization change, we will notify you at least 60 days in advance via the provider. Web specialty medication precertification request page 1. Check out this section to learn what it is and why it’s important. The services that need prior authorization. For medicare advantage part b: Prior authorization criteria is available. Web medicare form botulinum toxins injectable medication precertification request page 2 of 3 (all fields must be completed and legible for precertification review.) for medicare. Web attach supporting documentation if covered services and those requiring prior authorization change, we will notify you at least 60 days in advance via the provider. Pharmacy specialty drug prior authorization. Aetna specialty precertification forms abatacept (orencia ® ) precertification request form (pdf,. Web find out how to request precertification for botox injections for your patients with aetna. Web specialty. Web the basics of prior authorization. Pharmacy specialty drug prior authorization. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Start date / / aetna precertification. Web find the documents and forms you need to request specialty medications. Prior authorization criteria is available. By fax download our pa. Web find out how to request precertification for botox injections for your patients with aetna. For medicare advantage part b: Download and fill out the form with the required information and fax it to the number. Web please call us at 800.753.2851 to submit a verbal prior authorization request if you are unable to use electronic prior authorization. Please use medicare request form fax: Web aetna considers botulinum toxin [botox (onabotulinumtoxina); Web attach supporting documentation if covered services and those requiring prior authorization change, we will notify you at least 60 days in advance via the provider. Aetna specialty precertification forms abatacept (orencia ® ) precertification request form (pdf,. Participating providers can now check for codes that require prior. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. In these cases, your doctor can submit a request on your behalf to get that. Web member complaint and appeal (pdf) pharmacy claim form (pdf) request for protected health information (phi) (pdf) revocation of authorization previously given to aetna. The services that need prior authorization.Free Aetna Prior (Rx) Authorization Form PDF eForms
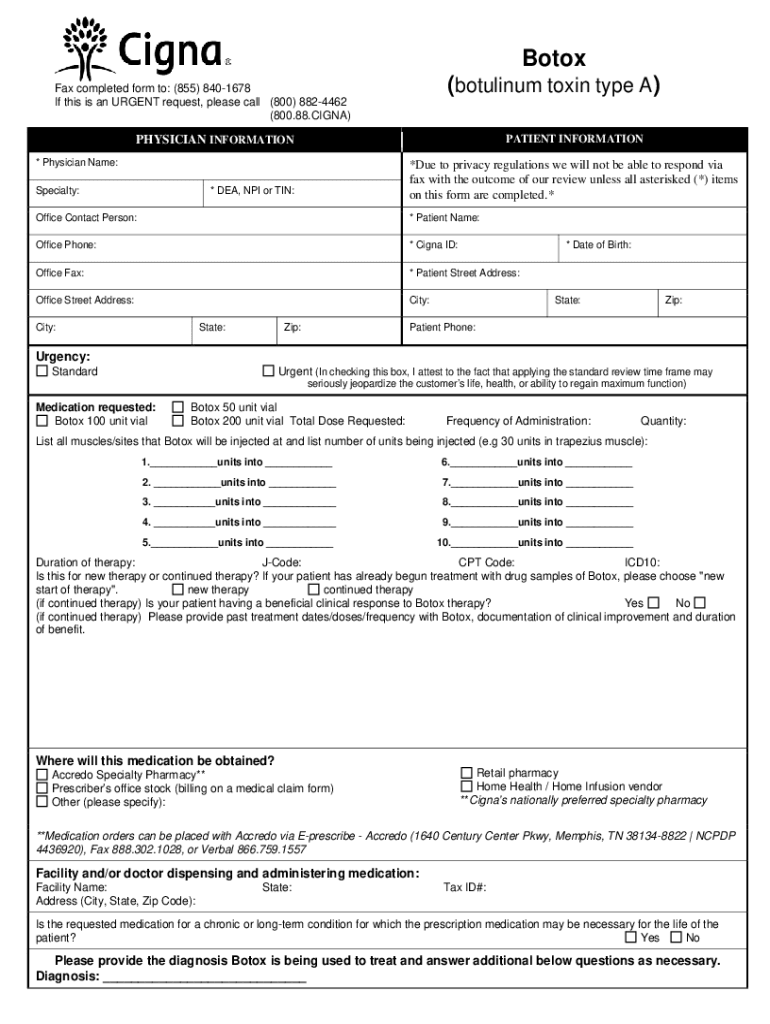
Cigna Botox Prior Authorization Form Fill Out and Sign Printable PDF
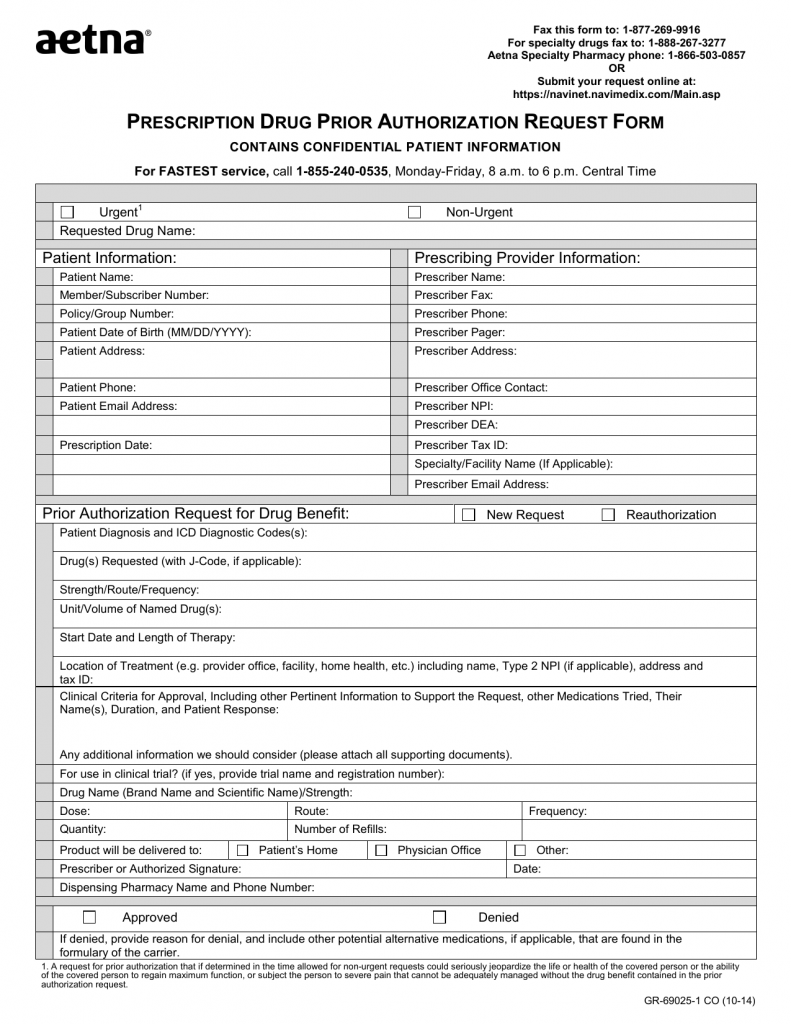
Download AETNA Prescription Drug Authorization Request Form PDF RTF
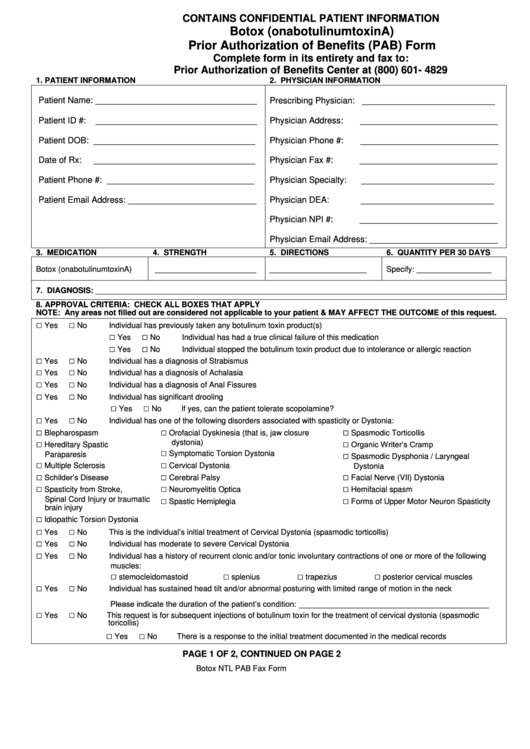
Botox (Onabotulinumtoxina) Prior Authorization Of Benefits (Pab) Form
Aetna Drug Plan Prior Authorization Form
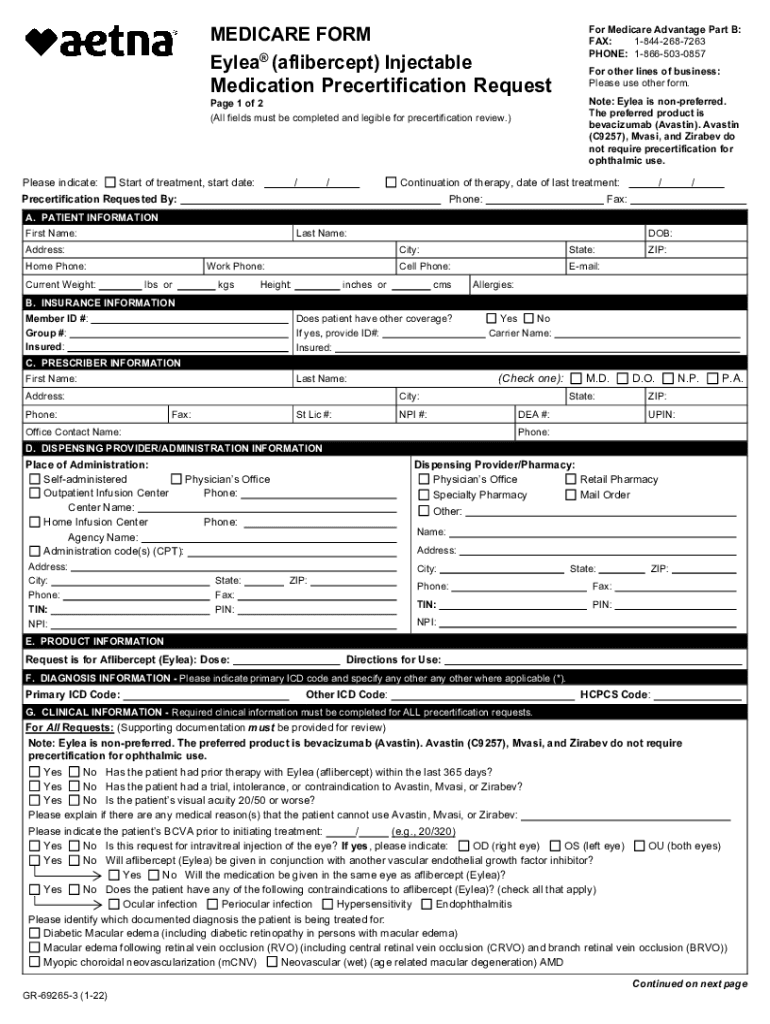
2022 Form Aetna GR69265 Fill Online, Printable, Fillable, Blank
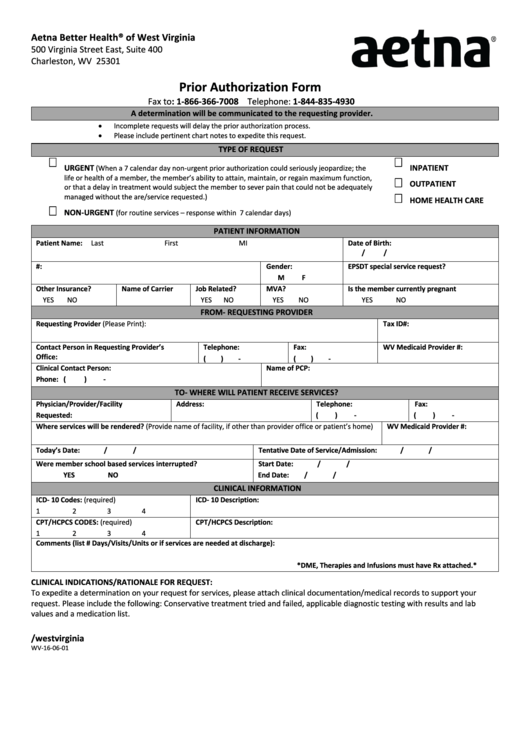
From Wv160601 Aetna Prior Authorization Form printable pdf download
Aetna Prior Authorization Form Medical Record Health Sciences
06/04/2013 Prior Authorization AETNA BETTER HEALTH OF PENNSYLVANIA Non
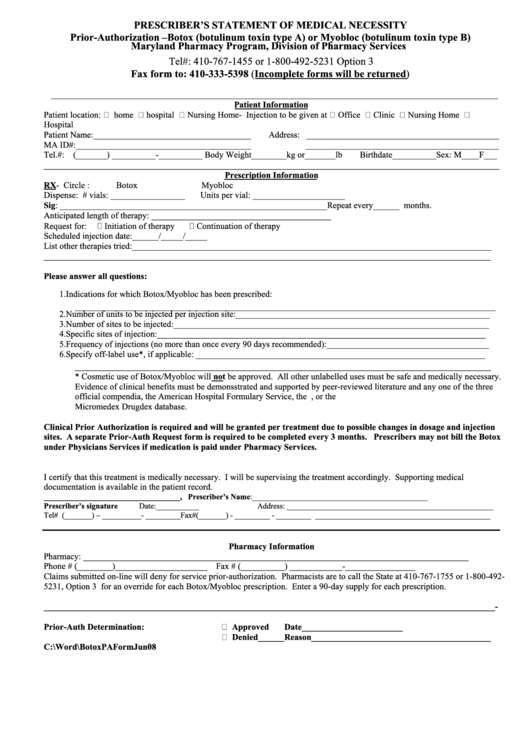
Botox Or Myobioc Prior Authorization Form Prescriber'S Statement Of
Related Post: