Aetna Better Health Prior Authorization Form
Aetna Better Health Prior Authorization Form - Web aetna better health ® of maryland requires pa for some outpatient care as well as for planned hospital admissions. Web complete form in its entirety and fax to the appropriate plan’s pa department. Upload, modify or create forms. You can’t use this form to initiate a precertification. Web this is called prior authorization. When a medication isn't listed on our preferred drug list, or has a utilization management requirement, you need to request a pharmacy prior. The medicare annual enrollment period ends in 46 days days. • always verify member eligibility prior to providing services. Web view prior authorization policy. Pa is not needed for emergency care. Web aetna providers observe prior authorization guidelines. The medicare annual enrollment period ends in 46 days days. Web view prior authorization policy. Use availity to access novologix®, our portal for drug. A current list of the. Use availity to access novologix®, our portal for drug. • complete the appropriate authorization form (medical or pharmacy). However, prior authorization is not required for. Aetna better health℠ premier plan requires prior authorization for select services. Enroll in a plan before dec 7 This extra check connects you to the right treatment, so you can. However, prior authorization is not required for. Web member complaint and appeal (pdf) pharmacy claim form (pdf) request for protected health information (phi) (pdf) revocation of authorization previously given to aetna. • complete the appropriate authorization form (medical or pharmacy). To determine if prior authorization (pa) is required,. Ad need a medicare plan that meets your health needs? Complete the texas standard prior authorization request form (pdf). Web precertiication list for aetna® efective october 1, 2023 this document is a quick guide for your oice to use for precertiication with patients enrolled in aetna health plans. Web aetna better health ® of maryland requires pa for some outpatient. Web tips for requesting authorizations. Web the new physical health standard prior authorization request form is located on our aetna better health of florida website under for providers, authorizations tab:. Pa requests received by phone will have. To submit a request, call our precertification. Web member complaint and appeal (pdf) pharmacy claim form (pdf) request for protected health information (phi). We send updates every hour. To determine if prior authorization (pa) is required, enter up to. Aetna better health℠ premier plan requires prior authorization for select services. Web the availity auth/referral dashboard. Pa requests received by phone will have. How may i obtain precertification on certain drugs? Ad need a medicare plan that meets your health needs? We send updates every hour. You can’t use this form to initiate a precertification. Upload, modify or create forms. Web the new physical health standard prior authorization request form is located on our aetna better health of florida website under for providers, authorizations tab:. • complete the appropriate authorization form (medical or pharmacy). Call to speak with a licensed agent. Get information about aetna’s precertification requirements, including. Pa is not needed for emergency care. Pa is not needed for emergency care. Web tips for requesting authorizations. Web precertiication list for aetna® efective october 1, 2023 this document is a quick guide for your oice to use for precertiication with patients enrolled in aetna health plans. Ad need a medicare plan that meets your health needs? You can’t use this form to initiate a precertification. Use availity to access novologix®, our portal for drug. Aetna better health℠ premier plan requires prior authorization for select services. Call to speak with a licensed agent. Web the availity auth/referral dashboard. Web aetna providers observe prior authorization guidelines. Web aetna providers observe prior authorization guidelines. Use availity to access novologix®, our portal for drug. To submit a request, call our precertification. When a medication isn't listed on our preferred drug list, or has a utilization management requirement, you need to request a pharmacy prior. A current list of the. Web complete form in its entirety and fax to the appropriate plan’s pa department. Web the availity auth/referral dashboard. Aetna better health premier plan mmai require prior authorization for select acute outpatient services and planned hospital admissions. • complete the appropriate authorization form (medical or pharmacy). • always verify member eligibility prior to providing services. Ad need a medicare plan that meets your health needs? Call to speak with a licensed agent. Web tips for requesting authorizations. To determine if prior authorization (pa) is required, enter up to. The medicare annual enrollment period ends in 46 days days. Web health benefits and health insurance plans contain exclusions and limitations. Ad register and subscribe now to work on your simply healthcare svc requiring pre auth form. Web the new physical health standard prior authorization request form is located on our aetna better health of florida website under for providers, authorizations tab:. You might also hear it called “preapproval” or “precertification”. Complete the texas standard prior authorization request form (pdf).Gallery of Aetna Better Health Prior Auth form Inspirational Health
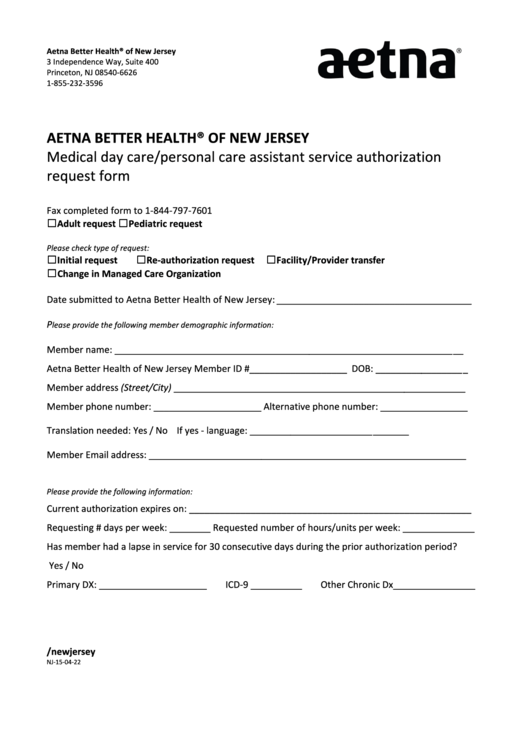
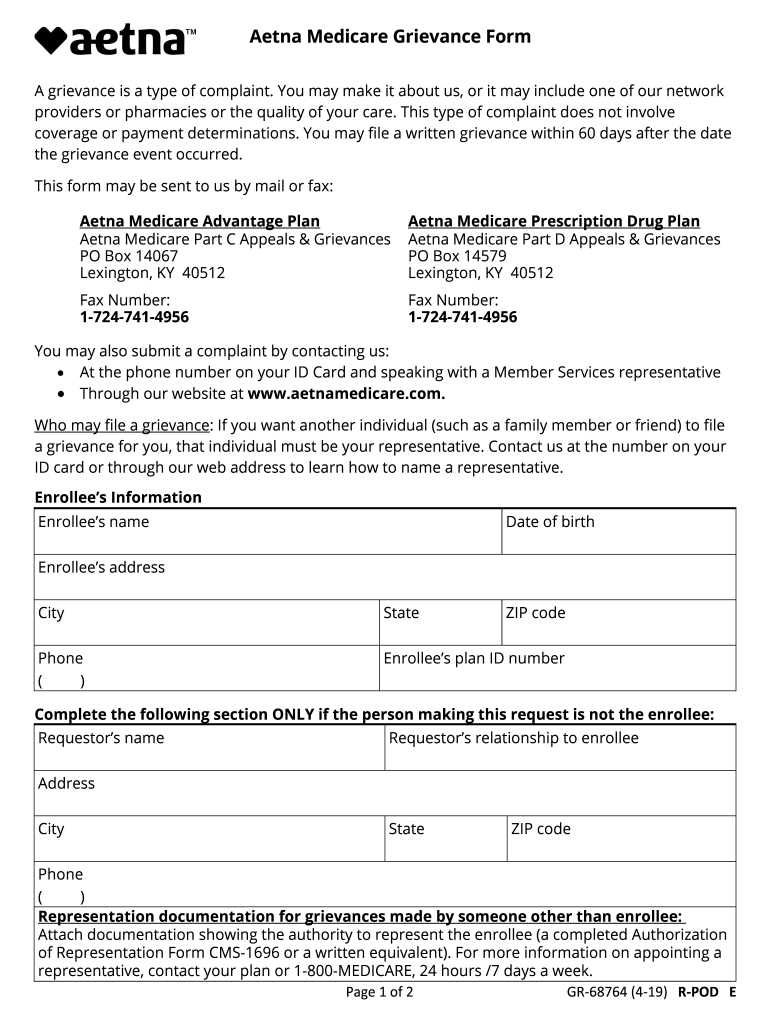
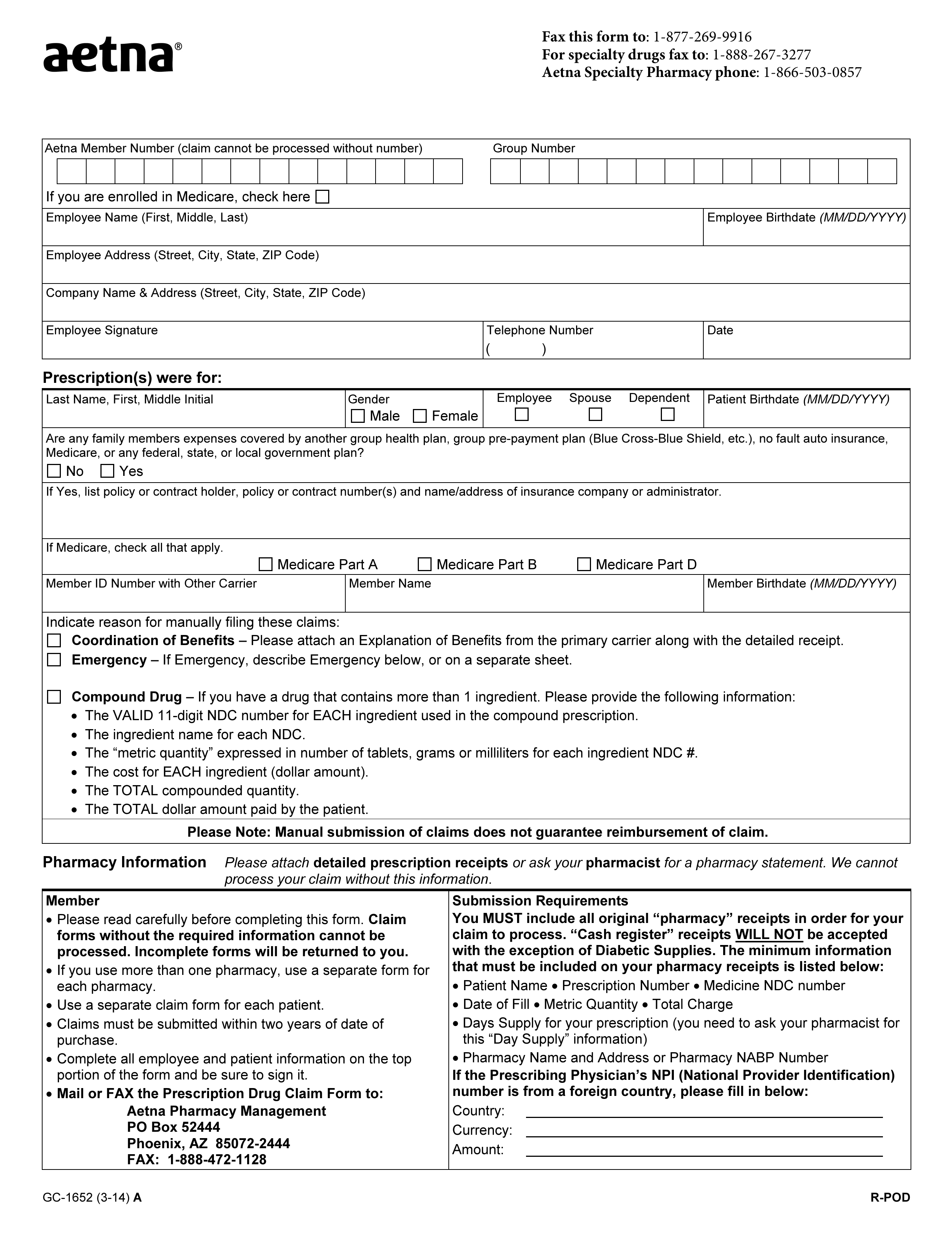
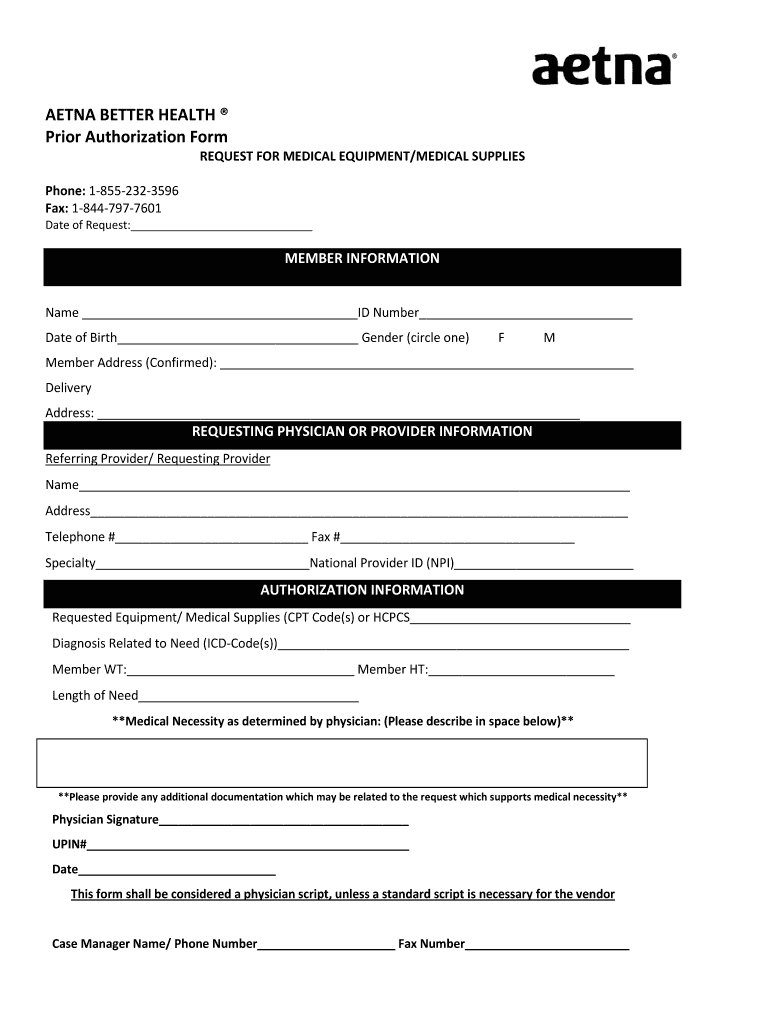
Top 6 Aetna Prior Authorization Form Templates free to download in PDF
Aetna Prior Authorization Form PDF Medical Record Health Sciences
Aetna better health application Fill out & sign online DocHub
Aetna Prior Authorization Form printable pdf download
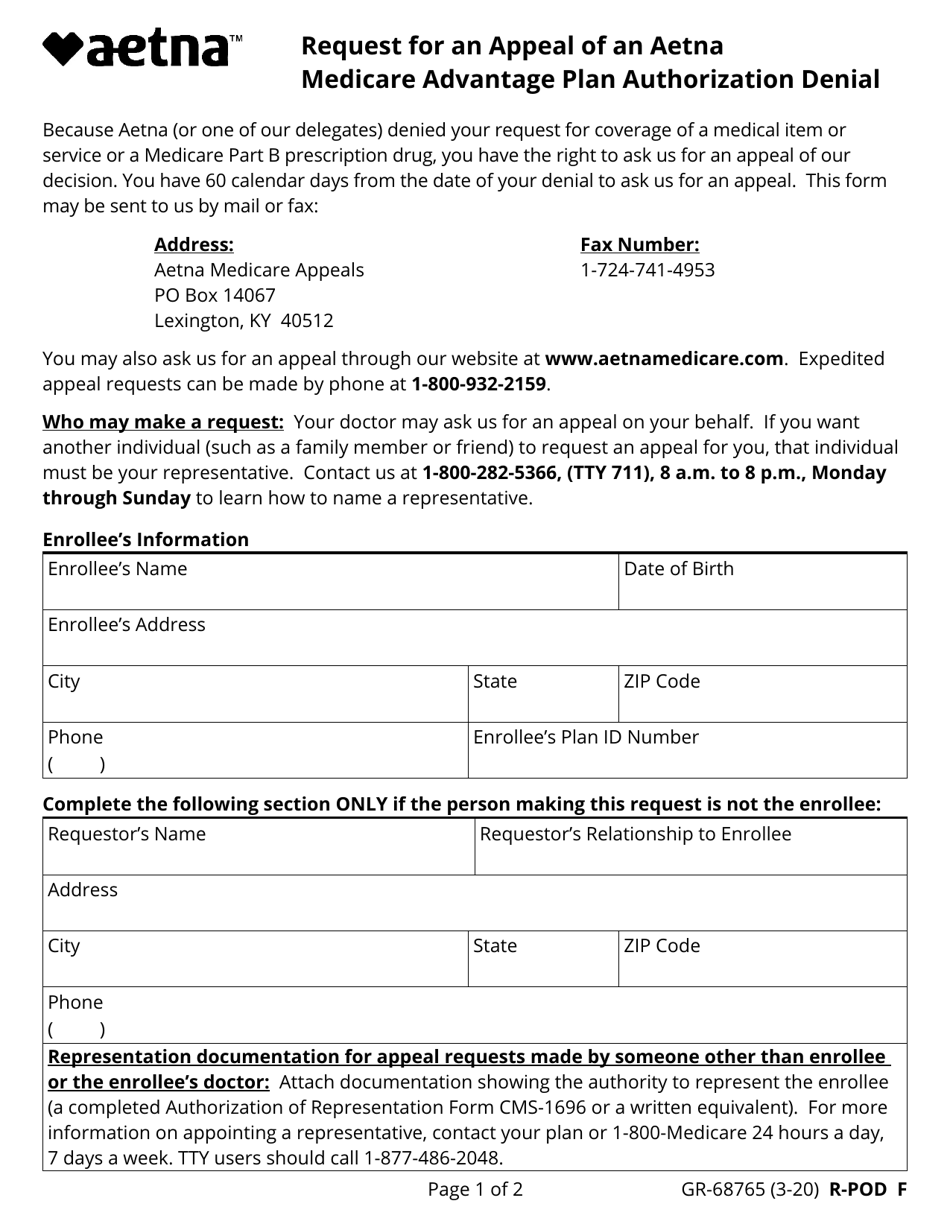
Aetna GR68764 2019 Fill and Sign Printable Template Online US
Free Aetna Prior (Rx) Authorization Form PDF eForms
Aetna Better Health Prior Authorization Fill and Sign Printable
Fillable Online Medicare Part D Prior Authorization Form Vectibixtm Po 6E6
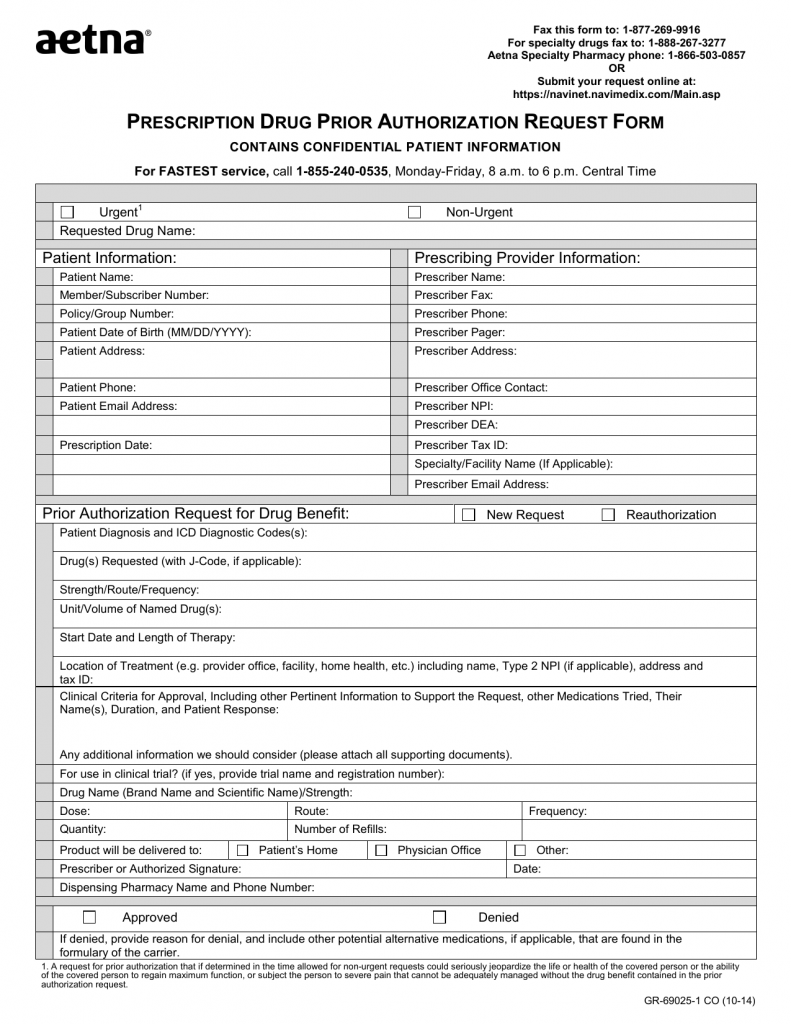
Download AETNA Prescription Drug Authorization Request Form PDF RTF
Related Post: