Uphp Prior Authorization Form
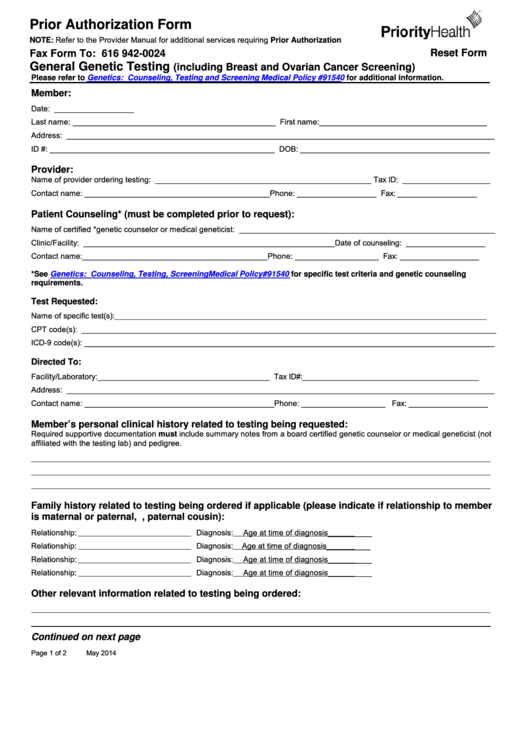
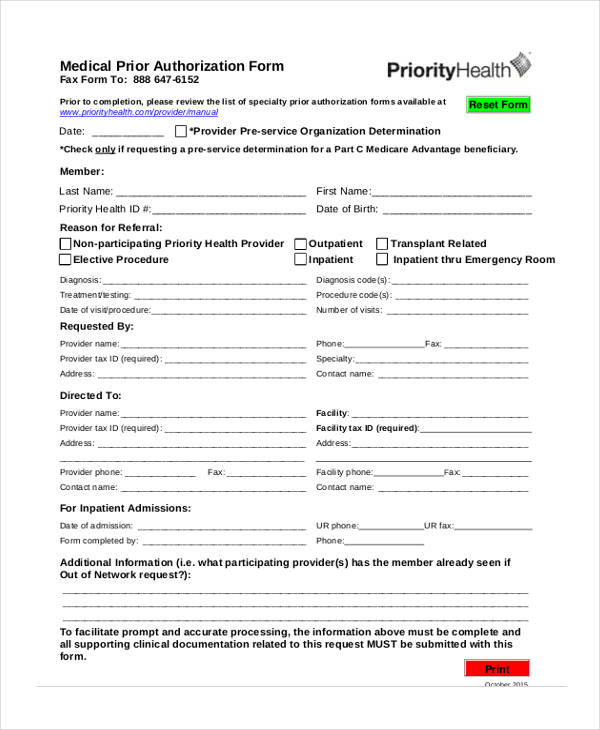
Uphp Prior Authorization Form - Provider submits in writing by fax (preferred), phone or mail: Easily fill out pdf blank, edit, and sign them. Web service request requires prior authorization or notification. Web prior authorization applies to new starts only. Web prior authorization and notification is the digital tool that helps you submit inquiries, process requests and get status updates. (all authorizations are pending valid eligibility). If urgent, give reason:_____ number of pages:_____ referral #: Web do not use this form: Web prior authorization request form routine: Prior authorization number (mdhhs use only). Request or access prior authorizations and view clinical guidelines. Easily fill out pdf blank, edit, and sign them. Provider submits in writing by fax (preferred), phone or mail: Web uphp prior authorization pa request form fax to 906 225 9269. Web certain drugs may require prior authorization or step therapy. Edit, sign and save uphp medical supply prior auth form. Web uphp health plan request for. For helpful tips and instructions, please refer to. Web uphp prior authorization pa request form fax to 906 225 9269. Web prior authorization request form routine: Web you must also date and sign the pieces of paper. Web do not use this form: Web •reviews prior authorization requests: Providers may utilize the prior authorization forms below to request approval of prior. Provider submits in writing by fax (preferred), phone or mail: Request or access prior authorizations and view clinical guidelines. Check out how easy it is to complete and esign documents online using fillable templates and a. Ad register and subscribe now to work on uphp dme/medical supply prior auth request form. For helpful tips and instructions, please refer to. Web 3 of 3 uhp_authorization/referral process overview 12.2020 note: You (or your physician) are required to get prior authorization before you fill your prescription for this drug. Web 3 of 3 uhp_authorization/referral process overview 12.2020 note: A standard prior authorization form, fis 2288, was created by the michigan department of insurance and financial services (difs) to simplify the process. The unitedhealthcare provider portal allows you to submit referrals, prior. Web prior authorization applies to new starts only. Web uphp health plan request for. Easily fill out pdf blank, edit, and sign them. Upper peninsula health plan (uphp) does require some services and items to be reviewed prior to you receiving those services or items. Upper peninsula health plan provider enrollment. Upper peninsula health plan provider enrollment. Prior authorization number (mdhhs use only). Web service request requires prior authorization or notification. If urgent, give reason:_____ number of pages:_____ referral #: Michigan department of health and human services 1. Ad register and subscribe now to work on uphp dme/medical supply prior auth request form. Web •reviews prior authorization requests: Michigan department of health and human services 1. Create this form in 5 minutes! Web do not use this form: Web certain drugs may require prior authorization or step therapy. Web you must also date and sign the pieces of paper. The unitedhealthcare provider portal allows you to submit referrals, prior authorizations, claims, claim reconsideration and appeals, demographic changes. Edit, sign and save uphp medical supply prior auth form. Provider submits in writing by fax (preferred), phone or mail: Michigan department of health and human services 1. Web upper peninsula health plan prior authorization form. Web service request requires prior authorization or notification. Web prior authorization request form routine: Prior authorization number (mdhhs use only). Web prior authorization and notification is the digital tool that helps you submit inquiries, process requests and get status updates. Web service request requires prior authorization or notification. Web uphp health plan request for. Access prior authorizations and view clinical. Upper peninsula health plan provider enrollment. Request or access prior authorizations and view clinical guidelines. (all authorizations are pending valid eligibility). Web prior authorization request form routine: Michigan department of health and human services 1. Easily fill out pdf blank, edit, and sign them. A standard prior authorization form, fis 2288, was created by the michigan department of insurance and financial services (difs) to simplify the process. Web uphp prior authorization pa request form fax to 906 225 9269. Web 3 of 3 uhp_authorization/referral process overview 12.2020 note: 1) to request an appeal, 2) to con~irm eligibility, 3) to verify coverage, 4) to ask whether a service requires prior authorization, 5) to request prior. Prior authorization number (mdhhs use only). Web •reviews prior authorization requests: Edit, sign and save uphp medical supply prior auth form. Providers may utilize the prior authorization forms below to request approval of prior. Getting informed permission before administering. If urgent, give reason:_____ number of pages:_____ referral #:Fillable Prior Authorization Form Priority Health printable pdf download
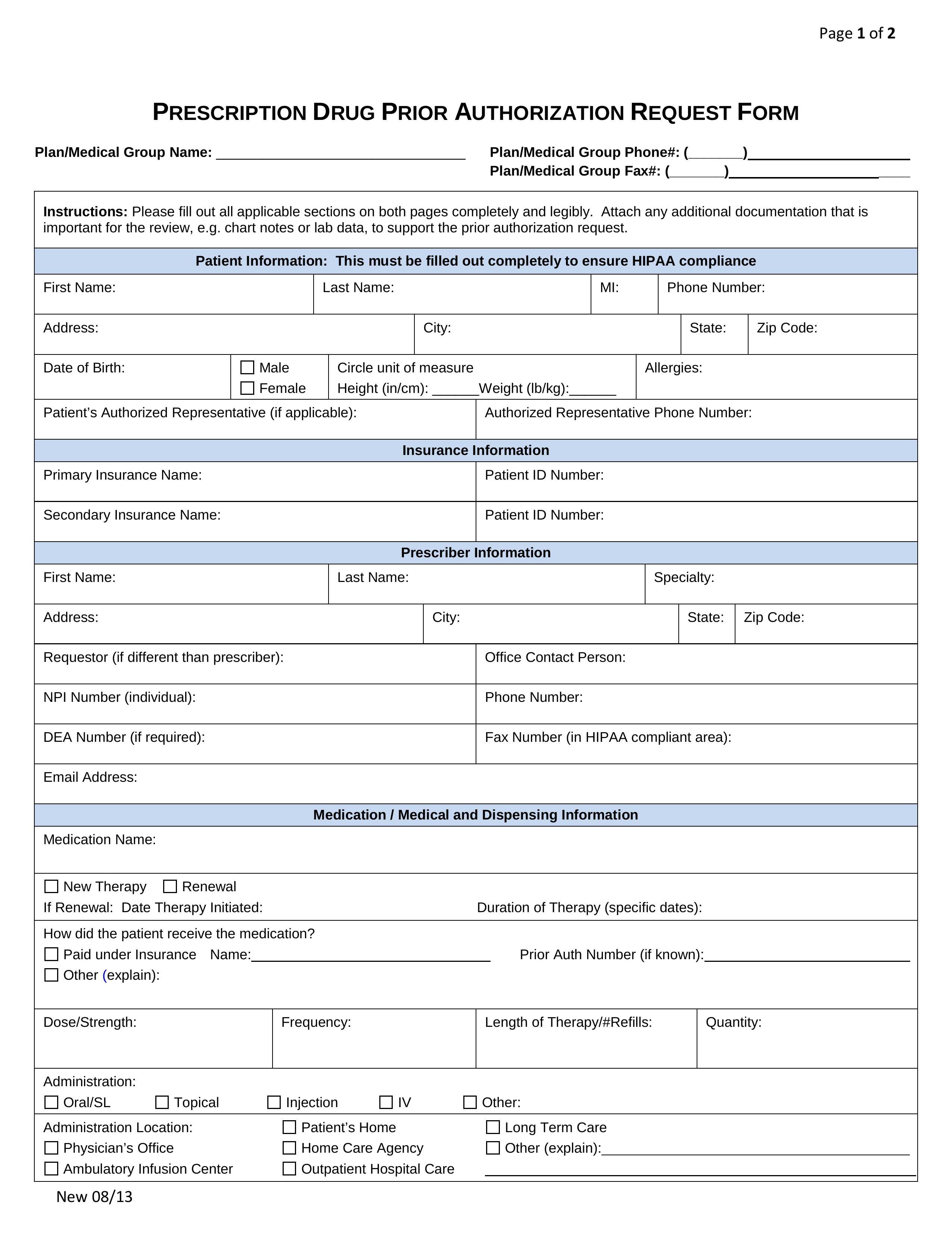
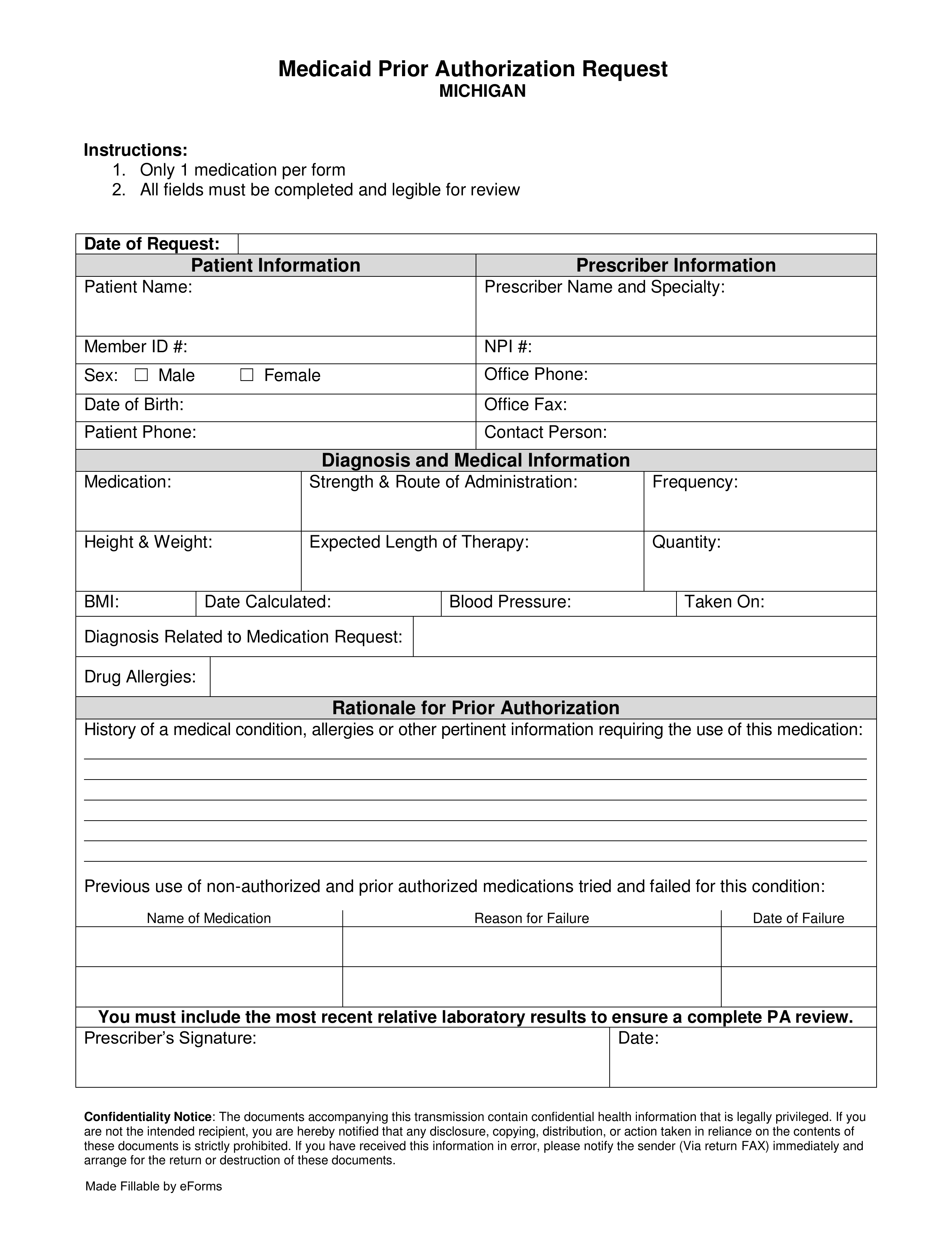
Free Prior (Rx) Authorization Forms PDF eForms
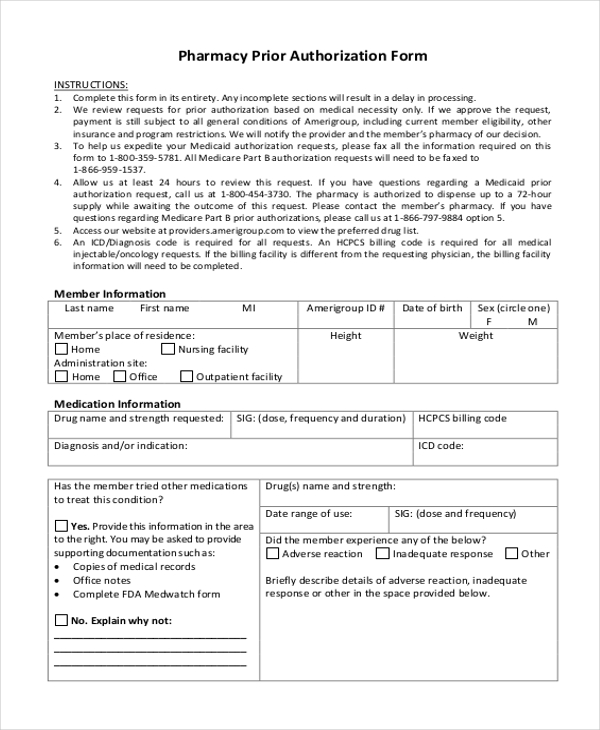
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
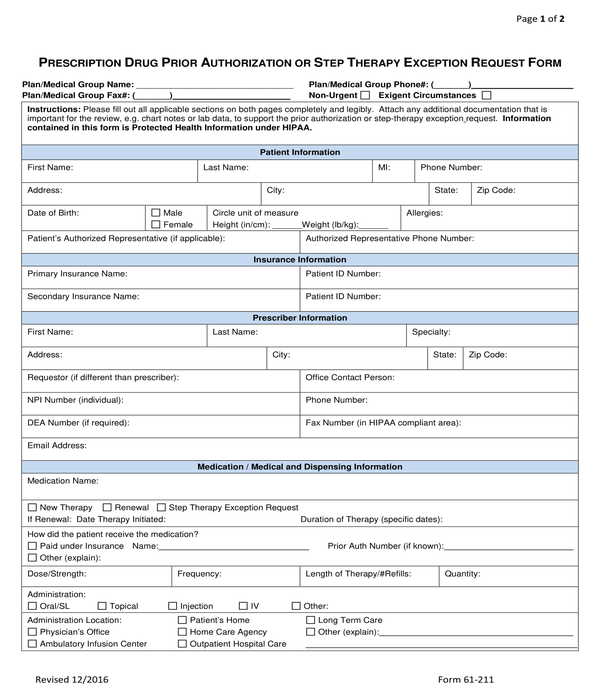
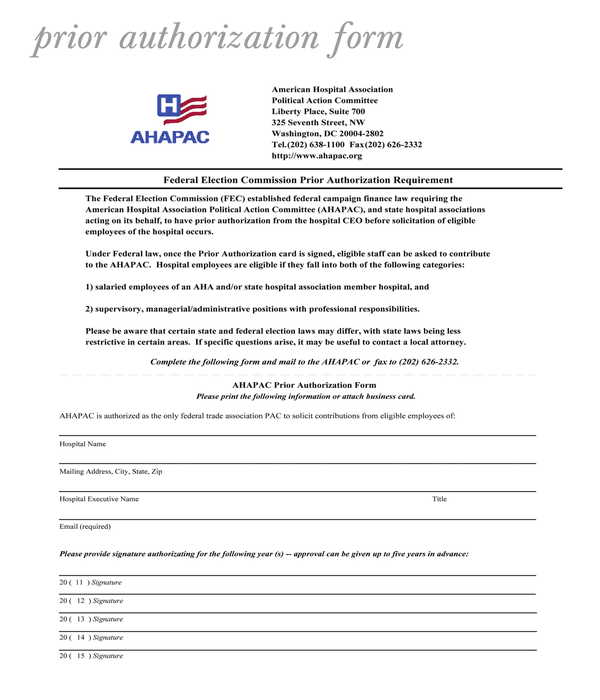
FREE 11+ Prior Authorization Forms in PDF MS Word
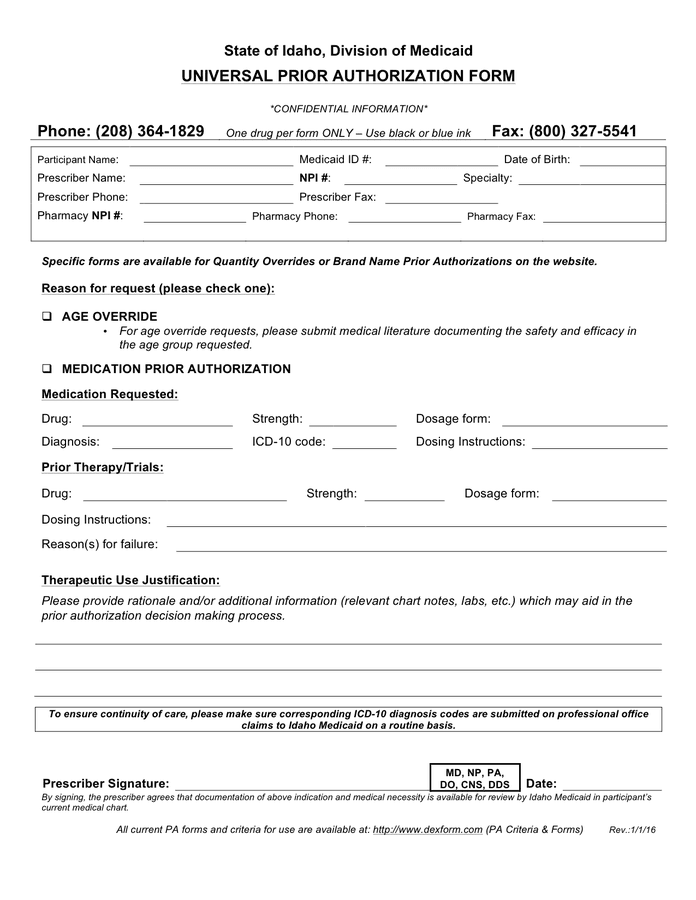
Universal prior authorization form in Word and Pdf formats
FREE 11+ Prior Authorization Forms in PDF MS Word
Free Michigan Medicaid Prior (Rx) Authorization Form PDF eForms
FREE 11+ Prior Authorization Forms in PDF MS Word
UPHP DME/Medical Supply Prior Authorization Request Form 20172022
FREE 13+ Prior Authorization Forms in PDF MS Word
Related Post: