Tricare Cgm Prior Authorization Form
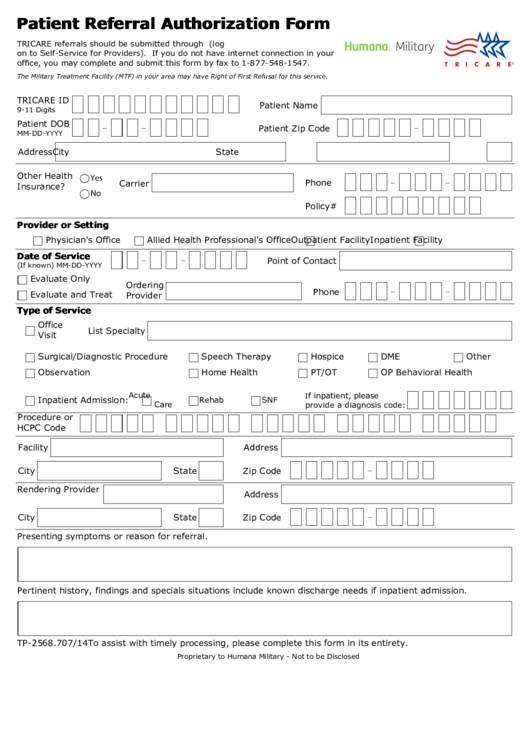
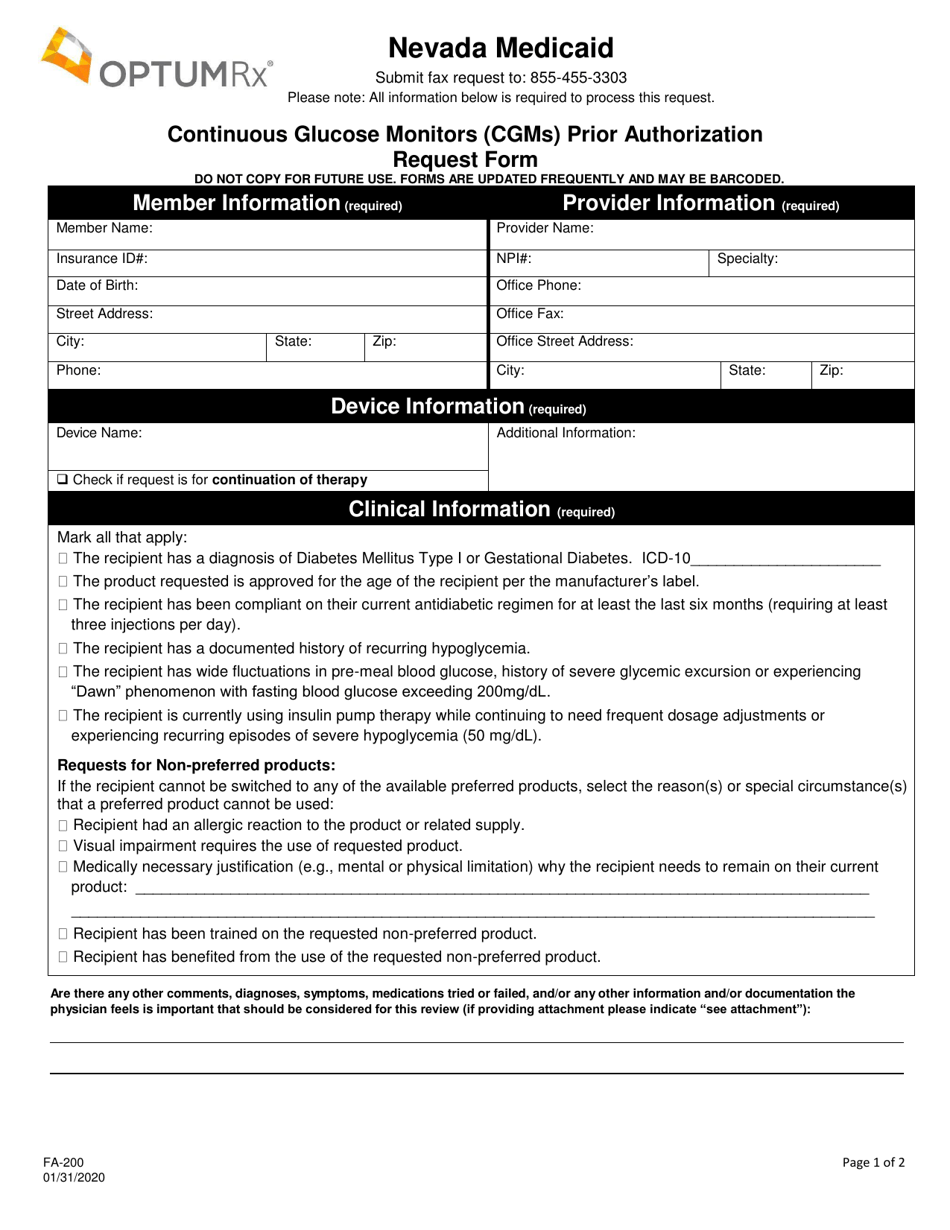
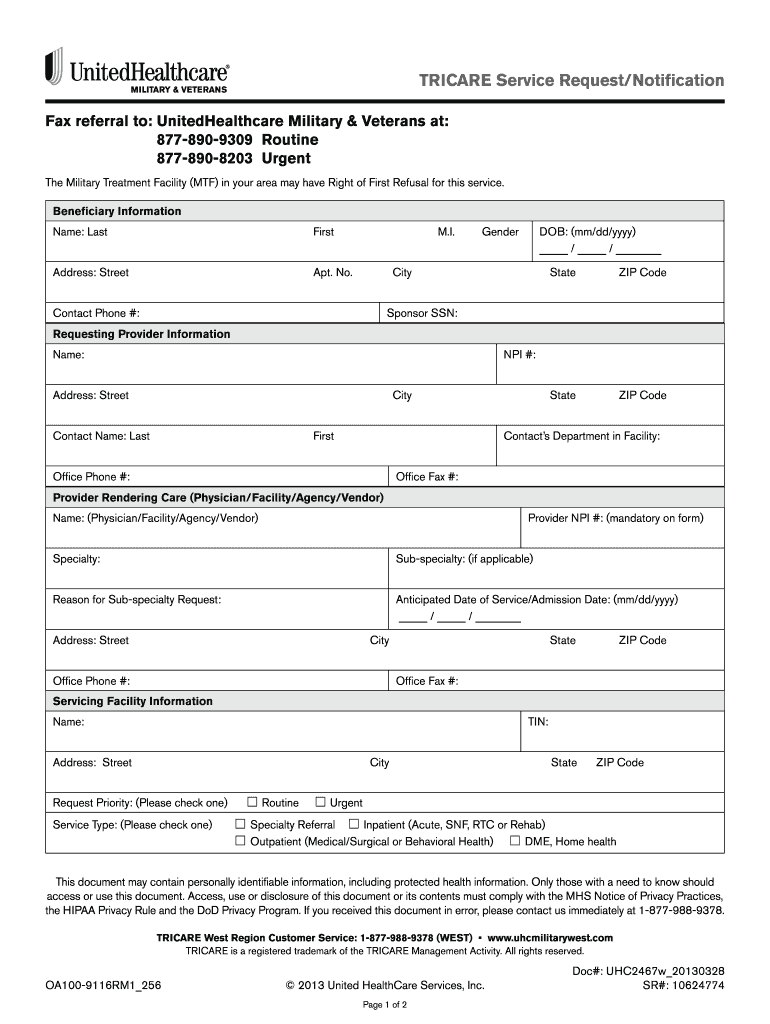
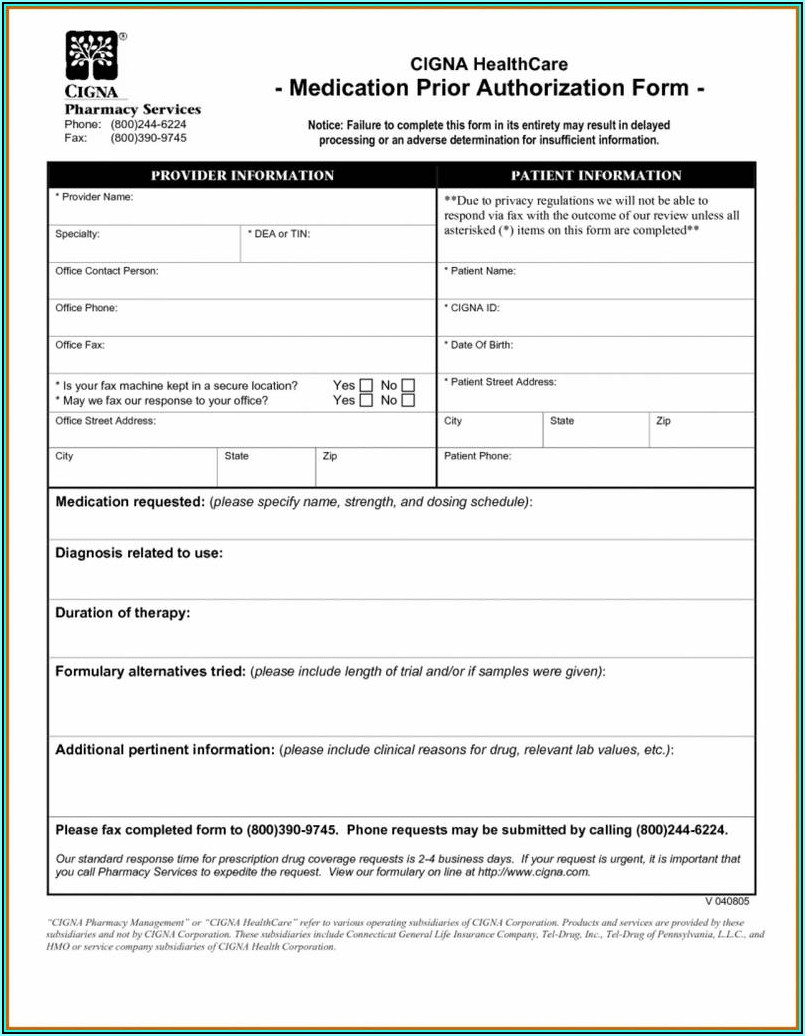
Tricare Cgm Prior Authorization Form - Web prior authorization requirements prior authorization is required for all ldts except for cystic fibrosis (cf) testing. Search for your drug on the tricare formulary search tool. • though not required, the attestation form was developed to streamline the information needed to ensure tricare policy is. A referral is not required for services. Valid for as long as you meet medical. Certain services (e.g., applied behavior analysis (aba), inpatient admissions, some behavioral. Review line of duty (lod) care. Providers must submit a completed ldt request and. Web the outpatient tricare pharmacy benefit evaluates several components including prior authorization criteria, step therapy, quantity limits, formulary status, and. Contact the pharmacy dept at: Web prior authorization requirements prior authorization is required for all ldts except for cystic fibrosis (cf) testing. Web the prior authorization, referral and benefit tool allows you to easily determine if an approval from health net federal services, llc (hnfs) is required. Web the outpatient tricare pharmacy benefit evaluates several components including prior authorization criteria, step therapy, quantity limits, formulary. We make it easy to share information get your written prescriptions to us by using our mail order form. Certain services (e.g., applied behavior analysis (aba), inpatient admissions, some behavioral. Find tricare claims forms, our medical questionnaire, and other. Web the outpatient tricare pharmacy benefit evaluates several components including prior authorization criteria, step therapy, quantity limits, formulary status, and. Enter. Providers must submit a completed ldt request and. Web the outpatient tricare pharmacy benefit evaluates several components including prior authorization criteria, step therapy, quantity limits, formulary status, and. • though not required, the attestation form was developed to streamline the information needed to ensure tricare policy is. Contact the pharmacy dept at: Web brand over generic prior authorization request form. Covermymeds is tricare prior authorization forms’s preferred method. You need a prescription and prior authorization. Web continuous glucose monitoring system (cgms) atestation form continuous glucose monitoring system (cgms) requests should be submited at. Contact the pharmacy dept at: Valid for as long as you meet medical. We make it easy to share information get your written prescriptions to us by using our mail order form. Search for your drug on the tricare formulary search tool. Covermymeds is tricare prior authorization forms’s preferred method. Valid for as long as you meet medical. Web to the prescription and the patient may attach the completed form mail it to: Web usfhp pharmacy prior authorization form questions? If you are being referred, your provider will get you a. Web • the referral/authorization is valid for two years. Web brand over generic prior authorization request form to be completed and signed by the prescriber. Web continuous glucose monitoring system (cgms) atestation form continuous glucose monitoring system (cgms) requests should be submited. You need a prescription and prior authorization. Web continuous glucose monitoring system (cgms) atestation form continuous glucose monitoring system (cgms) requests should be submited at. Request changes to my authorization. • though not required, the attestation form was developed to streamline the information needed to ensure tricare policy is. Search for your drug on the tricare formulary search tool. Valid for as long as you meet medical. You need a prescription and prior authorization. To be used only for prescriptions which are to be filled through the. Web • the referral/authorization is valid for two years. Web tricare select and all other beneficiaries. Providers must submit a completed ldt request and. Web to the prescription and the patient may attach the completed form mail it to: Contact the pharmacy dept at: Certain services (e.g., applied behavior analysis (aba), inpatient admissions, some behavioral. To be used only for prescriptions which are to be filled through the. Web continuous glucose monitoring system (cgms) atestation form continuous glucose monitoring system (cgms) requests should be submited at. Covermymeds is tricare prior authorization forms’s preferred method. Web prior authorization requirements prior authorization is required for all ldts except for cystic fibrosis (cf) testing. If you are being referred, your provider will get you a. A referral is not required for. You need a prescription and prior authorization. Providers must submit a completed ldt request and. Web continuous glucose monitoring system (cgms) atestation form continuous glucose monitoring system (cgms) requests should be submited at. Find tricare claims forms, our medical questionnaire, and other. Web tricare select and all other beneficiaries. Web to the prescription and the patient may attach the completed form mail it to: Web the outpatient tricare pharmacy benefit evaluates several components including prior authorization criteria, step therapy, quantity limits, formulary status, and. If you are being referred, your provider will get you a. Certain services (e.g., applied behavior analysis (aba), inpatient admissions, some behavioral. Web • the referral/authorization is valid for two years. We make it easy to share information get your written prescriptions to us by using our mail order form. Contact the pharmacy dept at: Review line of duty (lod) care. Covermymeds is tricare prior authorization forms’s preferred method. Web the prior authorization, referral and benefit tool allows you to easily determine if an approval from health net federal services, llc (hnfs) is required. Web prior authorization requirements prior authorization is required for all ldts except for cystic fibrosis (cf) testing. Web brand over generic prior authorization request form to be completed and signed by the prescriber. To be used only for prescriptions which are to be filled through the. Request changes to my authorization. • though not required, the attestation form was developed to streamline the information needed to ensure tricare policy is.Fillable Tricare Patient Referral Authorization Form printable pdf download
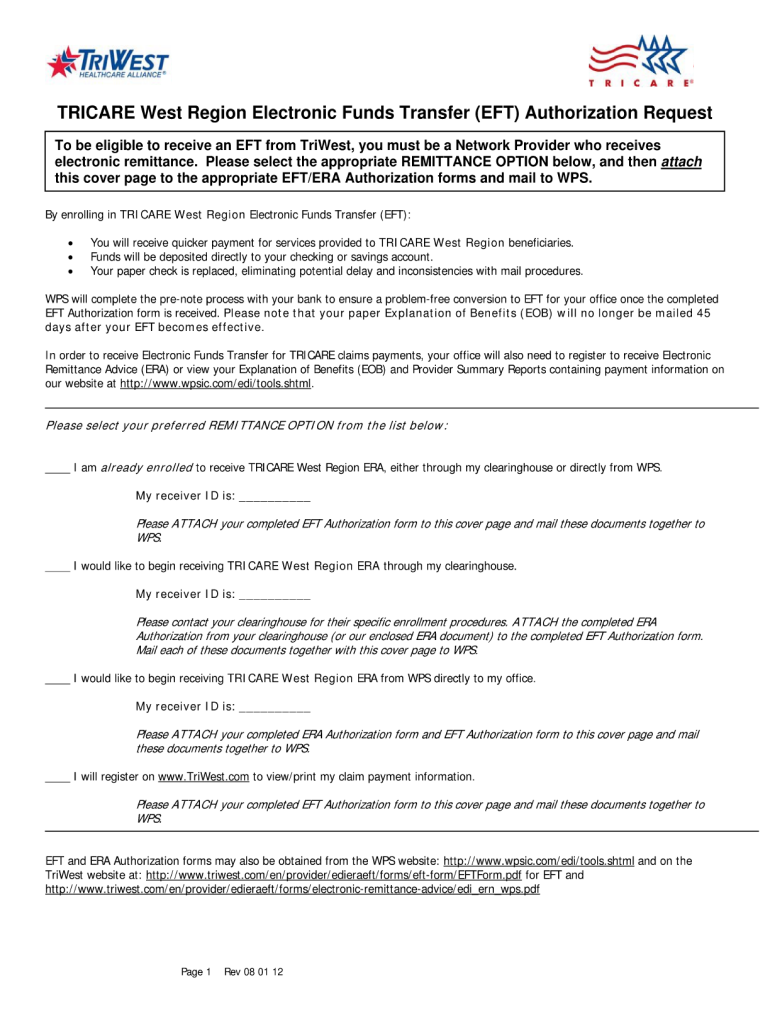
Tricare west region Fill out & sign online DocHub
Details for Tricare Patient Referral Authorization Form Template and
Form FA200 Download Printable PDF or Fill Online Continuous Glucose
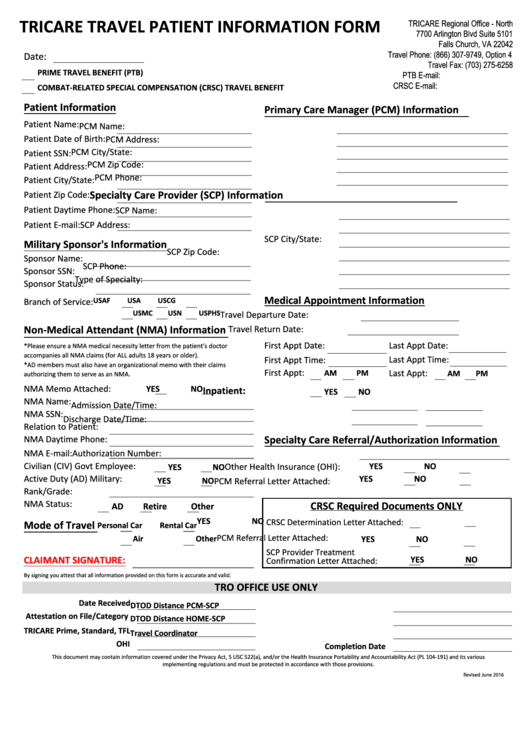
Tricare HF0315x019 20152022 Fill and Sign Printable Template Online
Free TRICARE Prior (Rx) Authorization Form PDF eForms
Tricare Pa Printable Forms Printable Forms Free Online
Covermymeds Humana Prior Auth Form / Aetna Prior Authorization Forms
Sample International SOS Authorization Form TRICARE Overseas Fill
Printable Tricare Forms Printable Forms Free Online
Related Post: