Rxbenefits Prior Authorization Form
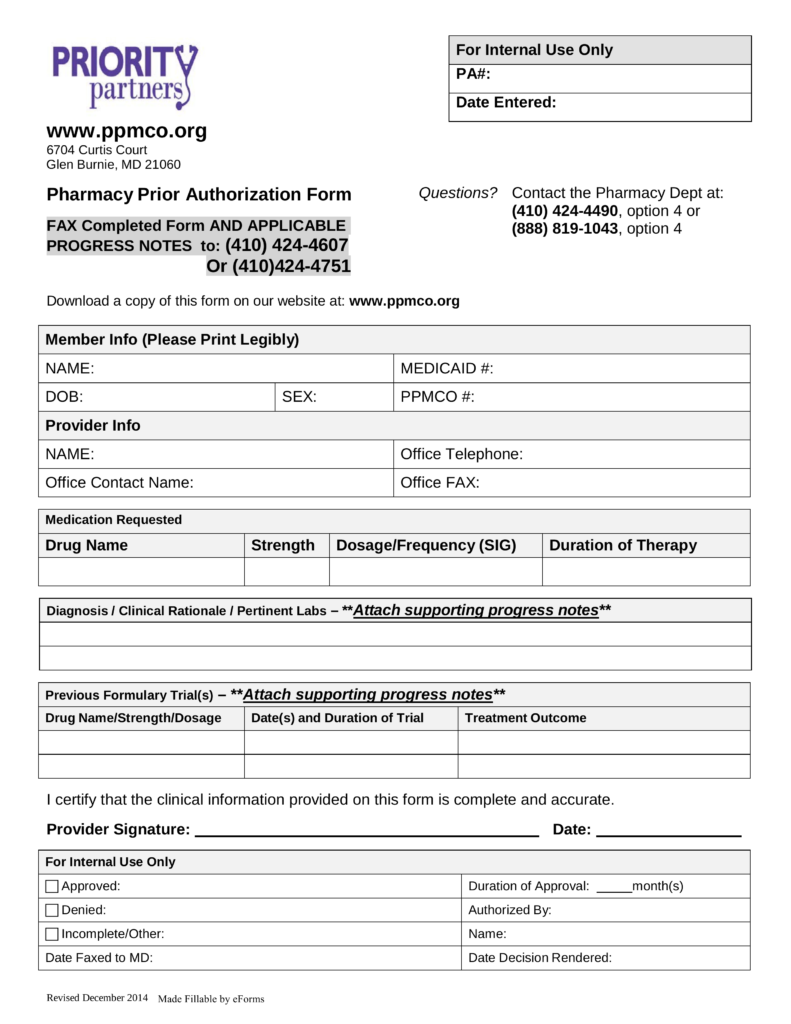
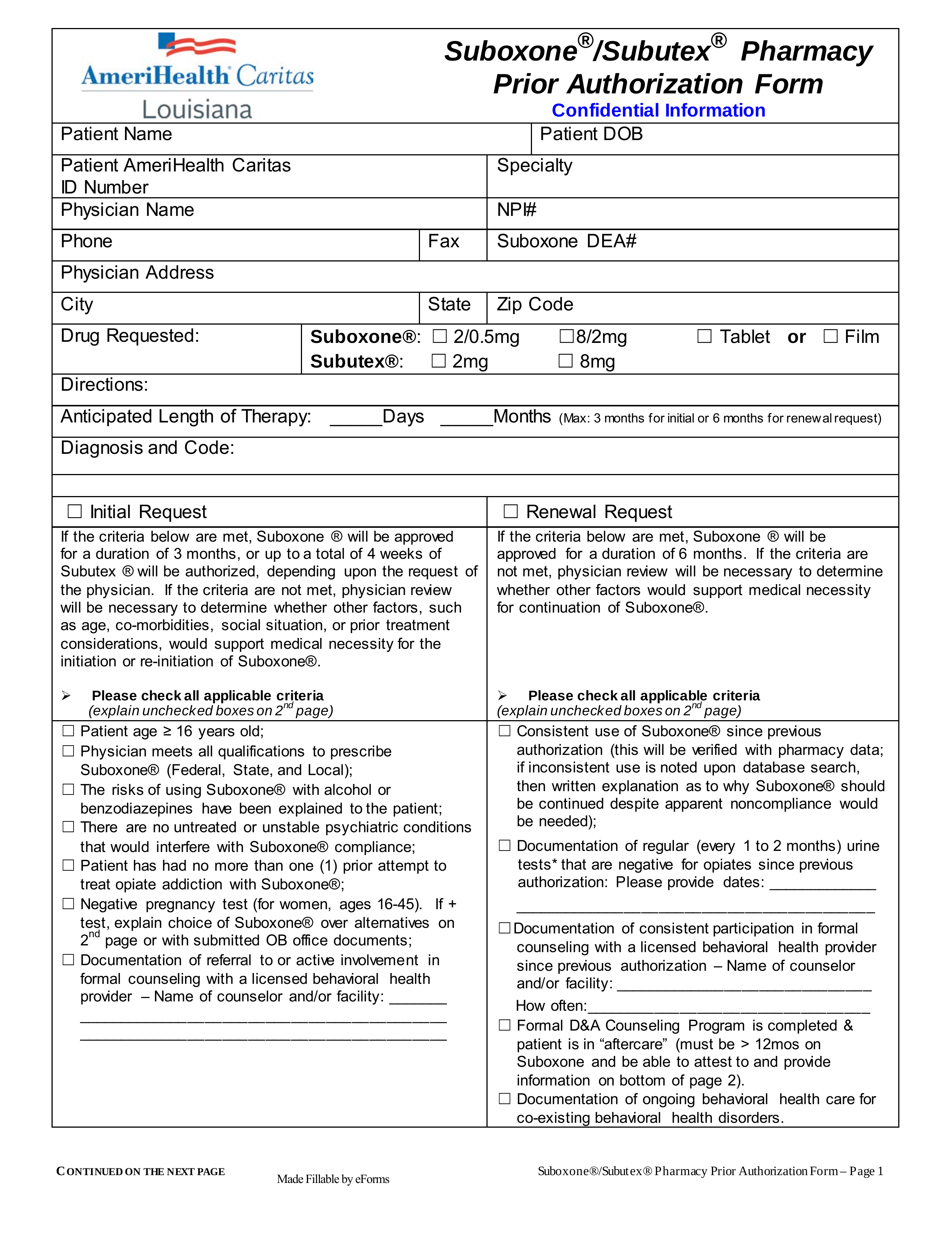
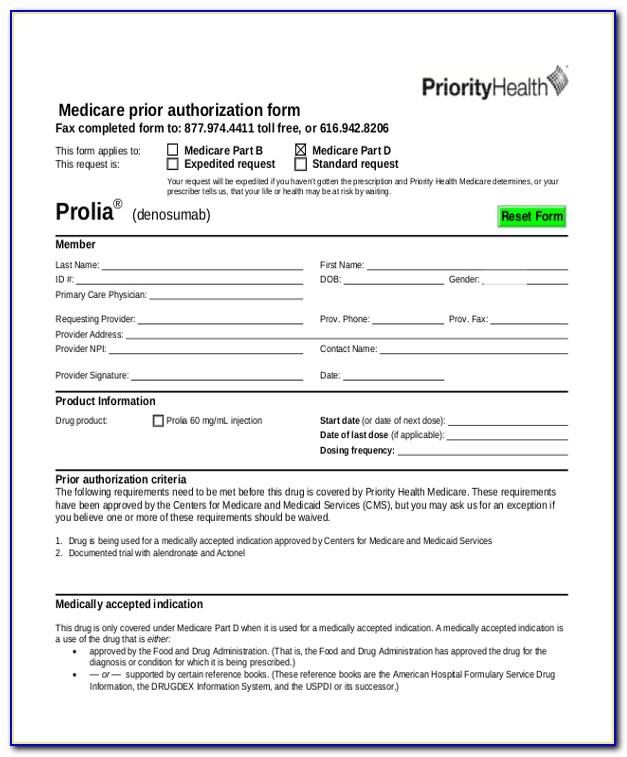
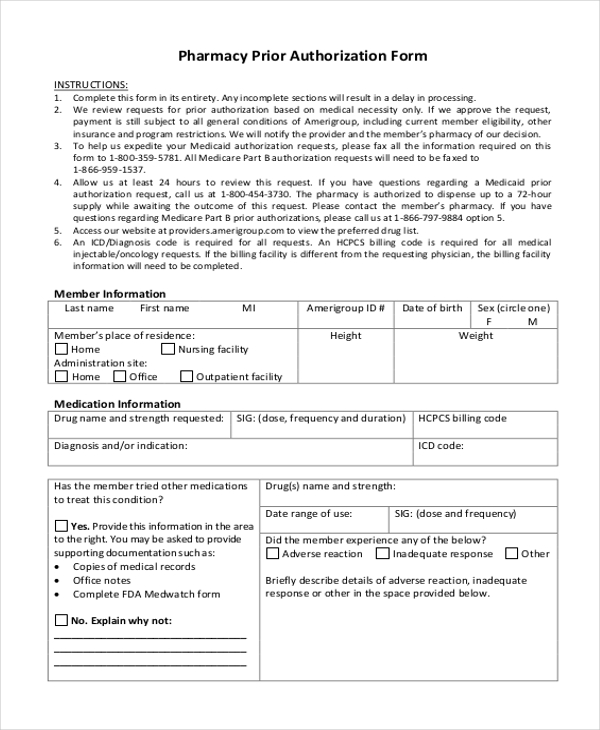
Rxbenefits Prior Authorization Form - Web optum rx prior authorization guidelines. A unique number assigned to the pa request. Web obtain prior authorization before you can fill your prescription. Web rx coverage and plan requirements. You can find this by profession the prior authorization line at 888.608.8851 or; Web your fastest form of contact will be to reach out to our member services team at [email protected]. Web reference the optumrx electronic prior authorization (epa ) and (fax) forms which contain clinical information used to evaluate the pa request as part of the determination. Click on the drug name to print the appropriate form, which should be completed, signed. Web prior authorization form check status on your pa request employer eligibility access your pbm solution: Web medication prior authorization request form fax completed form to 888.610.1180 or email to [email protected] electronic version available at. If you are having trouble. Looking for the prior authorization form? An rxbenefits prior authorization story as an employer, you know the importance of prioritizing your employees’ needs, but you also have to consider your. Web prior authorizations, commonly referred to as prior auths or pas, are designed to ensure that certain prescription drugs are used for appropriate medical. Web. Web drugs listed below require a prior authorization for coverage determination. Web up to 50% cash back download the rxbenefits prior auth request form. A unique number assigned to the pa request. Rxbenefits is a national pharmacy benefits optimizer focused on delivering full transparency and. You can find this by profession the prior authorization line at 888.608.8851 or; (hwmg) fax completed form to 888. You can find this by calling the prior authorization line at 888.608.8851 or you may have received a. Web prior authorization form check status on your pa request employer eligibility access your pbm solution: Web updated on 4.15.2020 medication prior authorization request form fax the completed form to 888.610.1180 electronic version available at. Web. Web prior authorizations (eoc) id: A unique number assigned to the pa request. Find out what terms like formulary and prior authorization mean and how these requirements can affect your medication options. Check status on your pa request. We never want you to go without an appropriate medication to treat your condition. You can find this by calling the prior authorization line at 888.608.8851 or you may have received a. Web pa’s the right way: A unique number assigned to the pa request. Web your fastest form of contact will be to reach out to our member services team at [email protected]. An rxbenefits prior authorization story as an employer, you know. A unique number assigned to the pa request. (hwmg) fax completed form to 888. Web prior authorizations, commonly referred to as prior auths or pas, are designed to ensure that certain prescription drugs are used for appropriate medical. Web pa’s the right way: You can find this by calling the prior authorization line at 888.608.8851 or you may have received. Find out what terms like formulary and prior authorization mean and how these requirements can affect your medication options. In those instances, prior authorization is required. Web pa’s the right way: We never want you to go without an appropriate medication to treat your condition. Description of service start date of service end date of service service code if available. A unique number assigned to the pa request. Click on the drug name to print the appropriate form, which should be completed, signed. Web up to 50% cash back download the rxbenefits prior auth request form. Web reference the optumrx electronic prior authorization (epa ) and (fax) forms which contain clinical information used to evaluate the pa request as part. A unique number assigned to the pa request. Web rx coverage and plan requirements. If you are having trouble. The epa solution supports all forms of pa and formulary exception requests. An rxbenefits prior authorization story as an employer, you know the importance of prioritizing your employees’ needs, but you also have to consider your. You can find this by profession the prior authorization line at 888.608.8851 or; Web pa’s the right way: Web rx coverage and plan requirements. (hwmg) fax completed form to 888. Web medication prior authorization request form fax completed form to 888.610.1180 or email to [email protected] electronic version available at. Web rxbenefits’ independent prior authorization review process prior authorizations (pas) can be a headache for members but are necessary in ensuring that they receive only the. Web optum rx prior authorization guidelines. (hwmg) fax completed form to 888. Web drugs listed below require a prior authorization for coverage determination. You can find this by profession the prior authorization line at 888.608.8851 or; Click on the drug name to print the appropriate form, which should be completed, signed. Web prior authorizations, commonly referred to as prior auths or pas, are designed to ensure that certain prescription drugs are used for appropriate medical. Exclusions may include cost reduction requests such as. You can find this by calling the prior authorization line at 888.608.8851 or you may have received a. Web updated on 4.15.2020 medication prior authorization request form fax the completed form to 888.610.1180 electronic version available at. Web reference the optumrx electronic prior authorization (epa ) and (fax) forms which contain clinical information used to evaluate the pa request as part of the determination. We never want you to go without an appropriate medication to treat your condition. If you are having trouble. Web up to 50% cash back download the rxbenefits prior auth request form. Check status on your pa request. Web pa’s the right way: Web medication prior authorization request form fax completed form to 888.610.1180 or email to [email protected] electronic version available at. Rxbenefits is a national pharmacy benefits optimizer focused on delivering full transparency and. Web rx coverage and plan requirements. Web prior authorizations (eoc) id:priority partners prior authorization forms Ten Easy Rules
Medicare Generation Rx Prior Authorization Form Form Resume
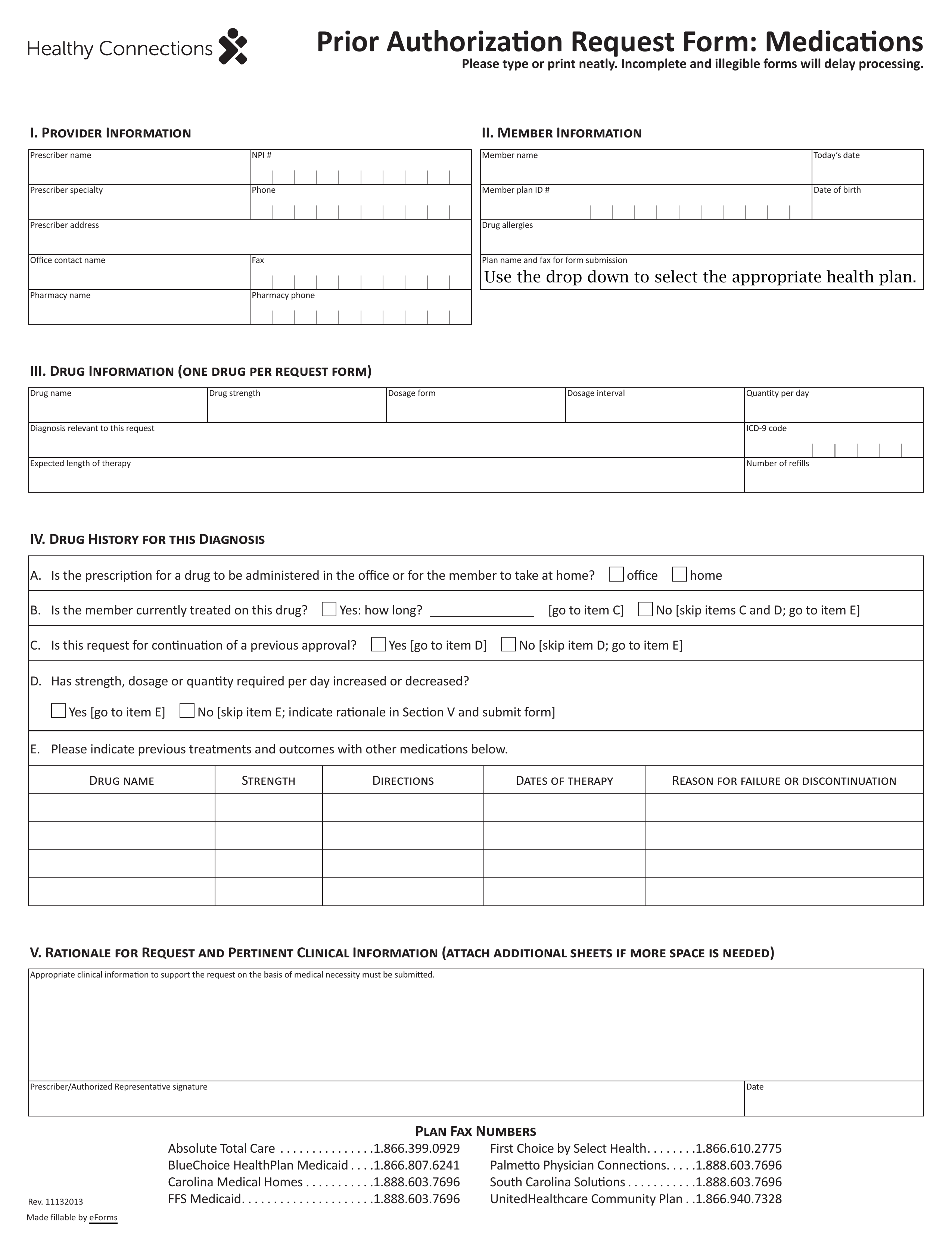
Free PerformRX Prior (Rx) Authorization Form PDF eForms
Medco Prior Auth Form Medication Form Resume Examples q25Z4Lxk0o
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
FREE 11+ Prior Authorization Forms in PDF MS Word
Fillable Online MEDICATION PRIOR AUTHORIZATION REQUEST FORM
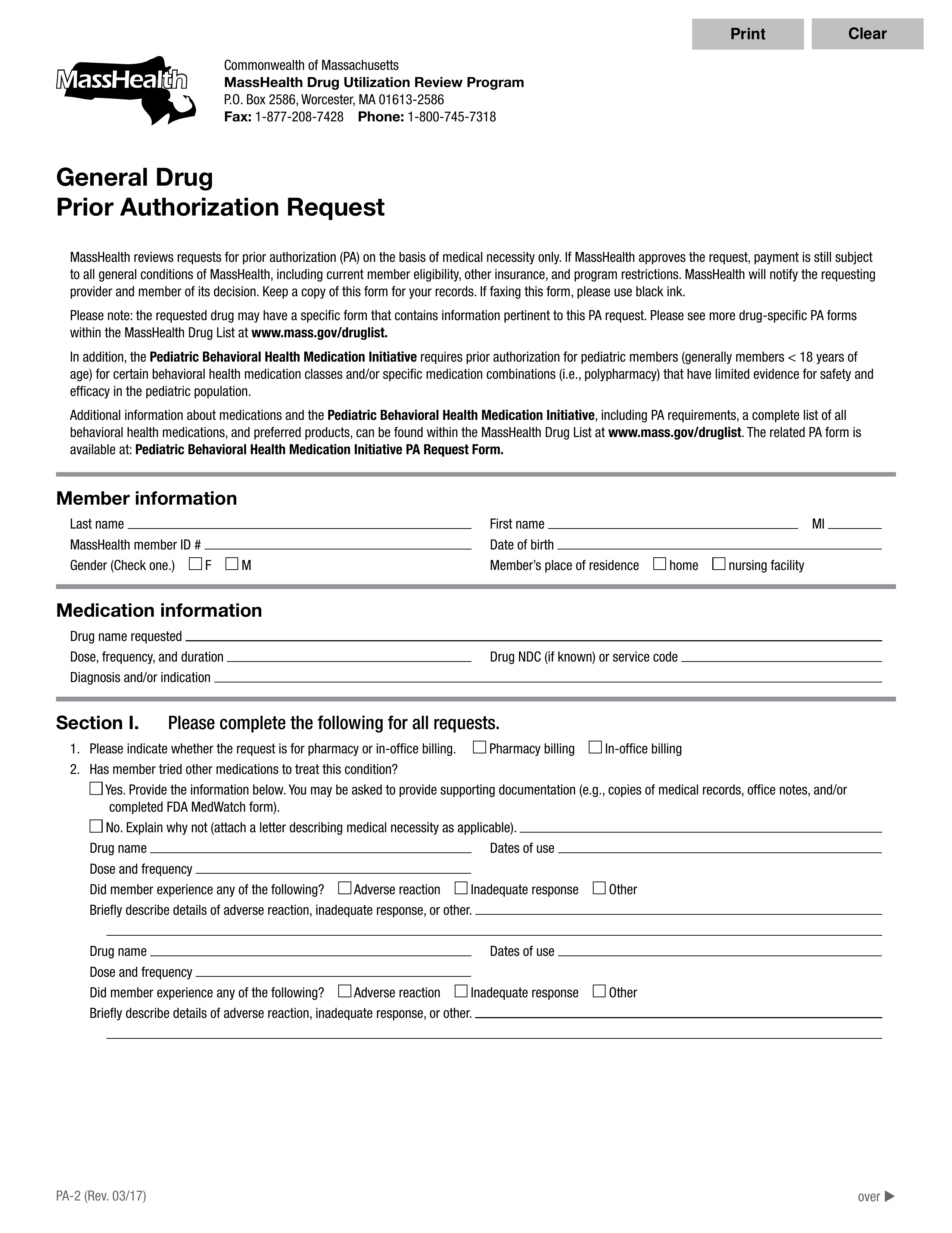
Free MassHealth Prior (Rx) Authorization Form PDF eForms
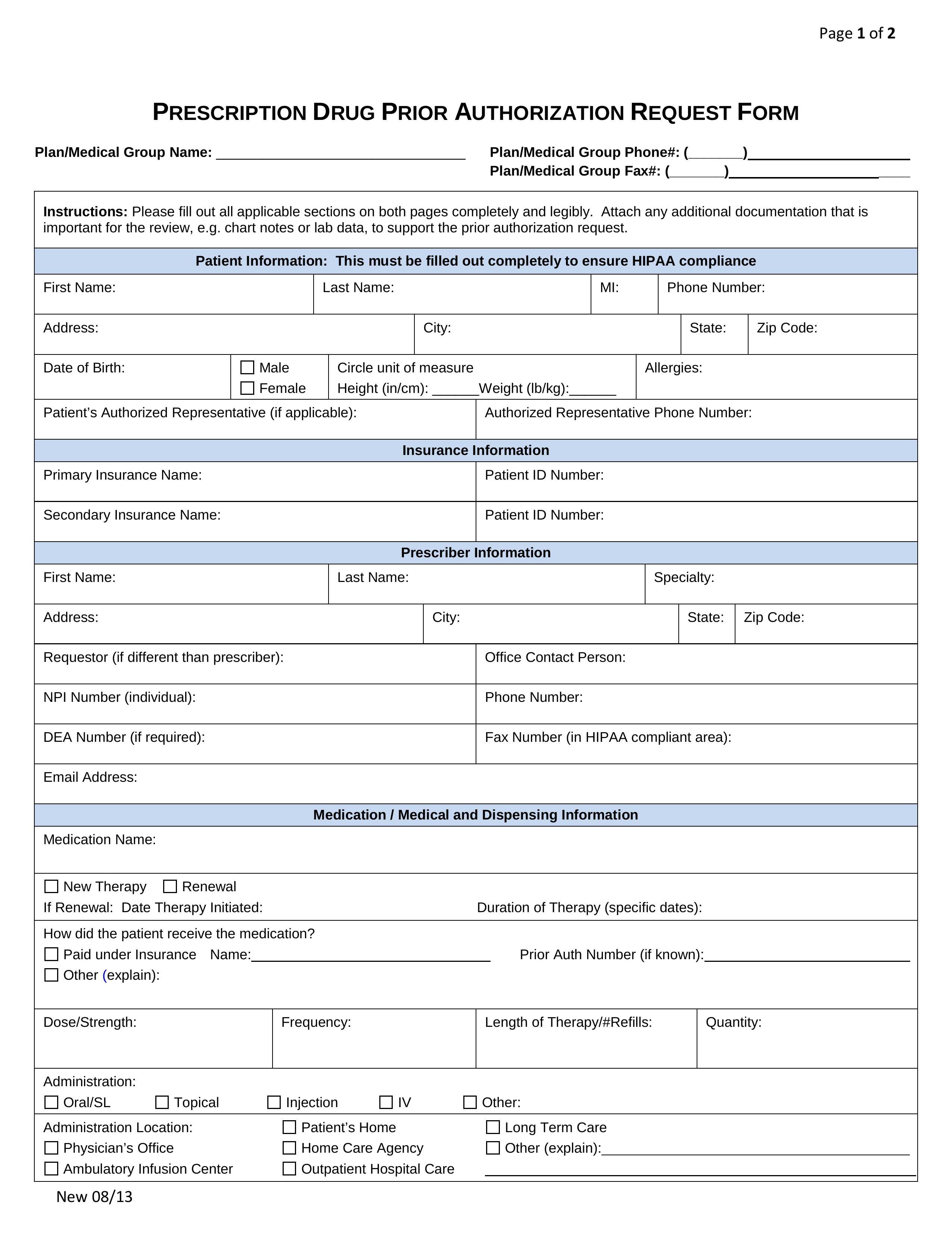
Free Prior (Rx) Authorization Forms PDF eForms
Free SelectHealth Prior (Rx) Authorization Form PDF eForms
Related Post: