Highmark Appeal Form
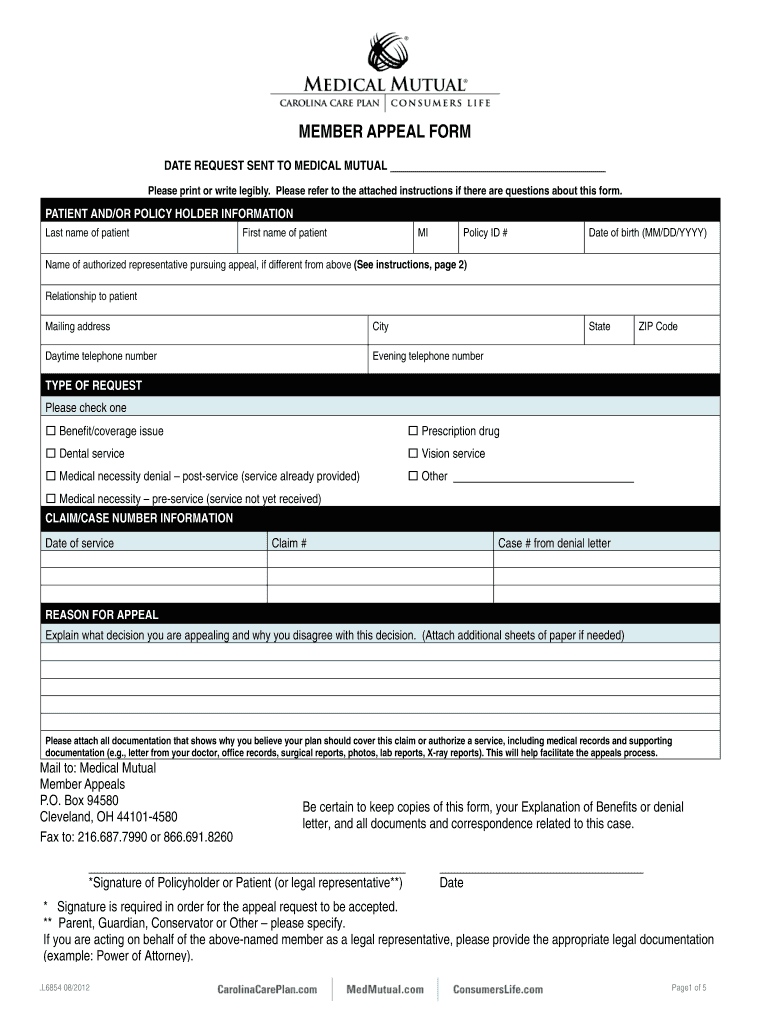
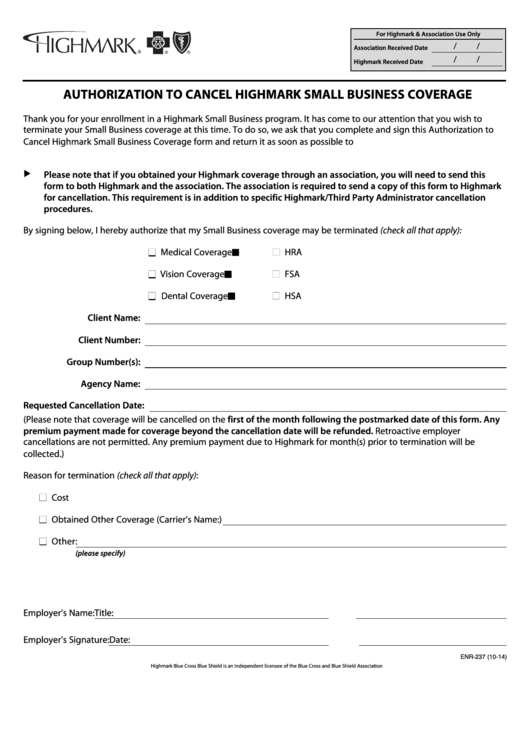
Highmark Appeal Form - The following questions will help us understand your appeal. 90 days form the date service provided. Web you may use the following forms for your convenience: Web use this form to request a redetermination/appeal from a plan sponsor on a denied medication request or direct claim denial. Either you or your treating provider can file an appeal on your behalf. Medicaid complaints, grievances & fair hearings. Can be used by you, your appointed. Request for medicare prescription drug coverage determination; Web at highmark, your concerns are important to us. As a highmark blue cross blue shield delaware (highmark de) participating provider,. This form must be completed and received at highmark health options within 60 days of the date on the “notice of adverse benefit determination.” how. Web or mail your completed and signed form to: Web you may use the following forms for your convenience: As a highmark health options member, you can ask for an appeal. Request for drug coverage. Web to appeal, you or your authorized representative must contact highmark delaware customer service within 180 days from the date you received the claim. Please turn to 2nd page for a few more questions <<issue>>. By filling out the appeal form online. The following questions will help us. As a blue cross blue shield of delaware (bcbsd) participating provider, you. Web use this form to request an appeal. This form must be completed and received at highmark health options within 60 days of the date on the “notice of adverse benefit determination.” how. 90 days form the date service provided. Web how can you file an appeal? Please turn to 2nd page for a few more questions <<issue>>. The following questions will help us understand your appeal. View the policies and procedures below to know your rights and how to submit an appeal or grievance. Web on this page, you will find some recommended forms that providers may use when communicating with highmark, its members or other providers in the network. Web you may also ask us for. Web when to file your appeal: Request for drug coverage form; At the end of this packet is a form that you may use for filing your appeal. Web who can file an appeal? Please turn to 2nd page for a few more questions <<issue>>. At the end of this packet is a form that you may use for filing your appeal. Medicaid complaints, grievances & fair hearings. Web who can file an appeal? Web on this page, you will find some recommended forms that providers may use when communicating with highmark, its members or other providers in the network. 90 days form the date. Web ̈ appeal (appeals must be submitted within 180 days of your receipt of the claim decision.) ̈ external review (external review requests must be submitted within four. This form must be completed and received at highmark health options within 60 days of the date on the “notice of adverse benefit determination.” how. As a highmark health options member, you. By filling out the appeal form that came with your letter and mailing it back. The following questions will help us. Web you may also ask us for an appeal through our website at www.highmarkblueshield.com. Web use this form to request a redetermination/appeal from a plan sponsor on a denied medication request or direct claim denial. Request for drug coverage. Web you may also ask us for an appeal through our website at www.highmarkblueshield.com. Medicaid complaints, grievances & fair hearings. As a highmark health options member, you can ask for an appeal. Can be used by you, your appointed. Web how can you file an appeal? At the end of this packet is a form that you may use for filing your appeal. Web ̈ appeal (appeals must be submitted within 180 days of your receipt of the claim decision.) ̈ external review (external review requests must be submitted within four. Web you have 60 days from the date on your notice of action to file. An appeal is a request for a review of a denied or limited. Web use this form to request a redetermination/appeal from a plan sponsor on a denied medication request or direct claim denial. Web anthem bcbs of ohio, kentucky, indiana and wisconsin timely filing limit for filing an initial claims: Web to appeal, you or your authorized representative must contact highmark delaware customer service within 180 days from the date you received the claim. By filling out the appeal form that came with your letter and mailing it back. Medicaid complaints, grievances & fair hearings. Web who can file an appeal? Web ̈ appeal (appeals must be submitted within 180 days of your receipt of the claim decision.) ̈ external review (external review requests must be submitted within four. Web at highmark, your concerns are important to us. Web how can you file an appeal? Either you or your treating provider can file an appeal on your behalf. Web when to file your appeal: As a highmark health options member, you can ask for an appeal. Web on this page, you will find some recommended forms that providers may use when communicating with highmark, its members or other providers in the network. By filling out the appeal form online. Web picture_as_pdf member appeal form. Request for medicare prescription drug coverage determination; Please turn to 2nd page for a few more questions <<issue>>. The following questions will help us understand your appeal. Web or mail your completed and signed form to:Medical Mutual Appeal Form Fill Out and Sign Printable PDF Template
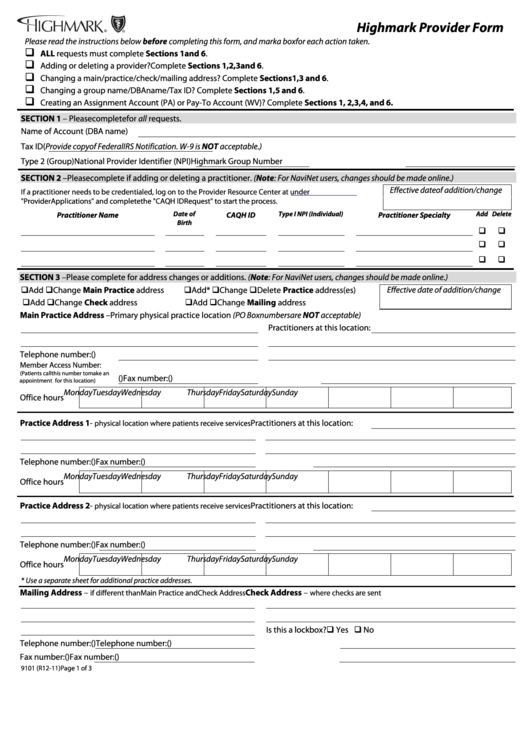
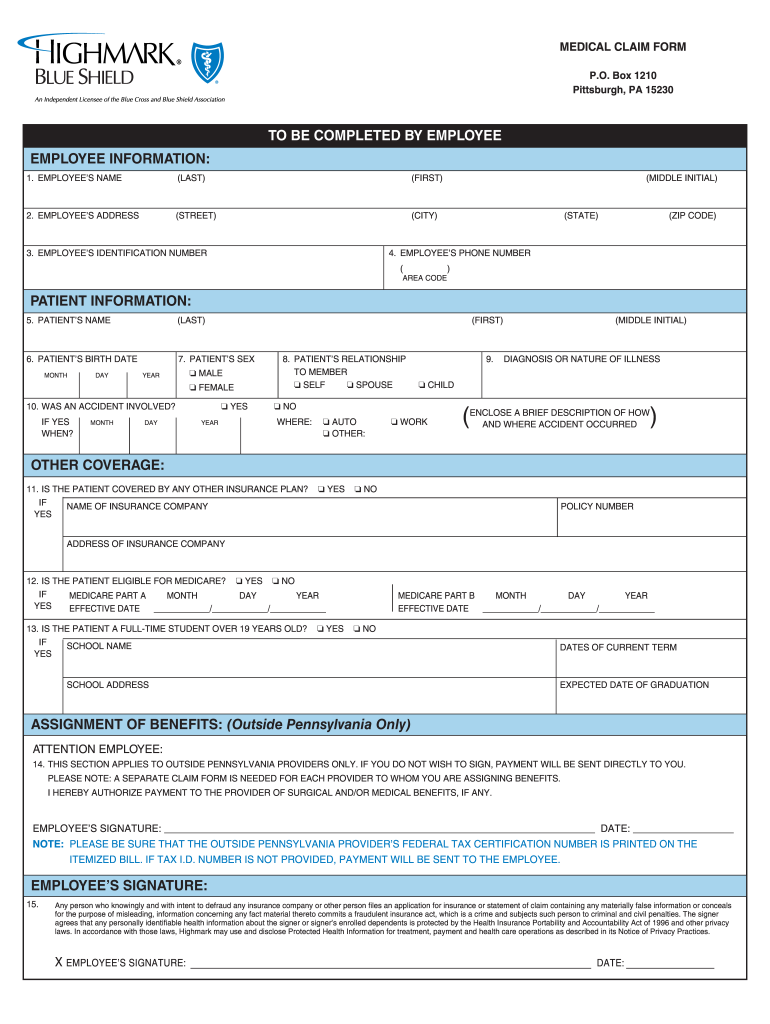
Form 9101 Highmark Provider Form Blue Cross Of Northeastern
2016 CA OSHAB Appeal Form 100 Fill Online, Printable, Fillable, Blank
Healthcare gov appeal form Fill out & sign online DocHub
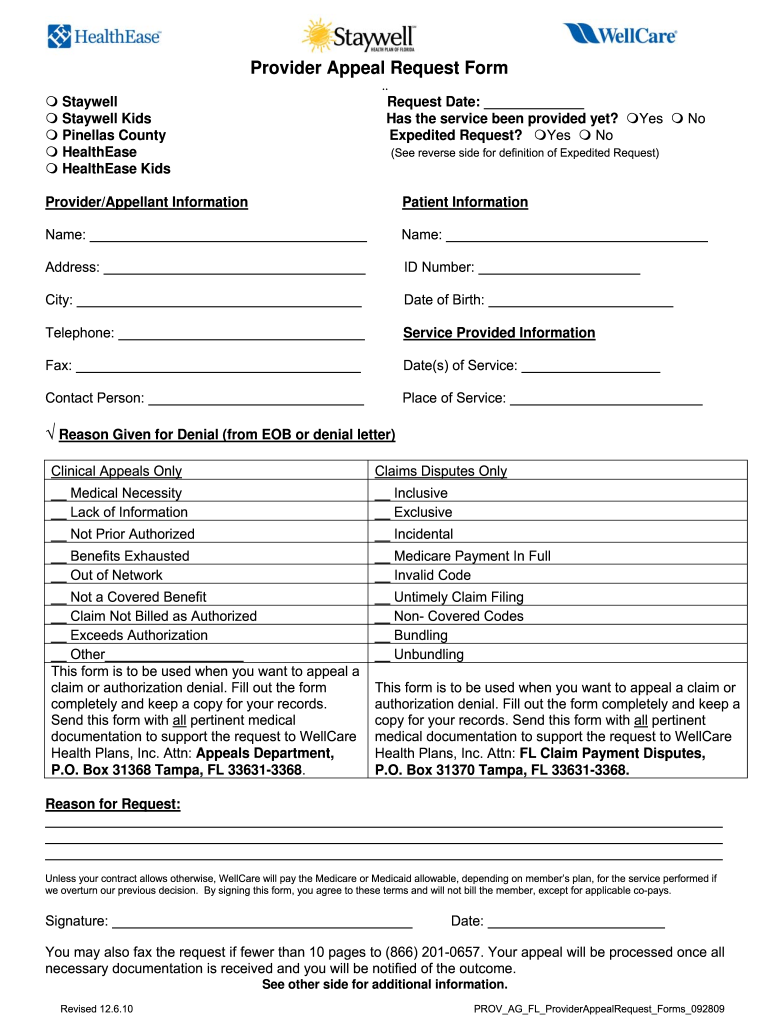
Wellcare Appeal Form Fill Out and Sign Printable PDF Template signNow
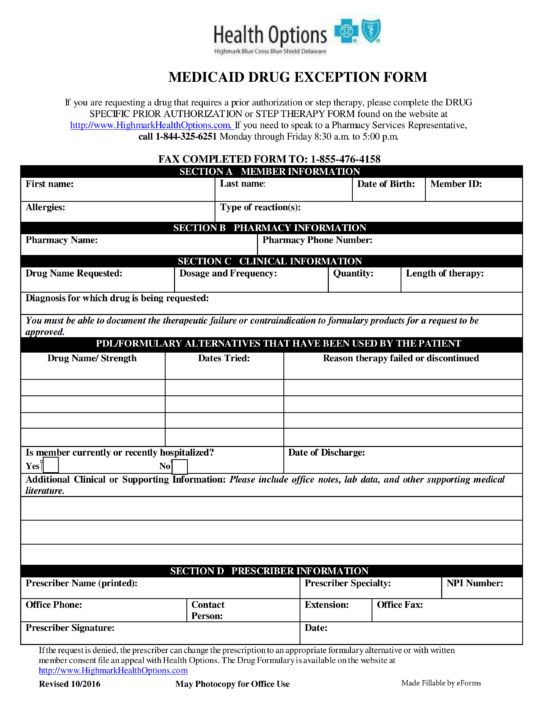
Top Highmark Prior Authorization Form Templates free to download in PDF
highmark bcbs form 1033c Fill out & sign online DocHub
US Court of Appeals Criminal Appeal Information Sheet Complete Legal
Free Delaware Medicaid Prior (Rx) Authorization Form PDF eForms
Fillable Highmark Patient Request For Medical Records Transfer Form
Related Post: