Fep Blue Prior Authorization Form
Fep Blue Prior Authorization Form - Web how to file internal and external appeals. Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. Upload, modify or create forms. Ad register and subscribe now to work on your blue advantage med part d prescriptn drug auth. Web standard and basic option prior approval list fep blue focus prior approval list. Preferred providers must be used in order to receive benefits. Web learn how we manage prior authorization & medical necessity determination requests for certain orthopedic and cardiac services for our fep members. Try it for free now! See the assigned federal brochures. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web most drugs are covered without requiring prior approval. Ad register and subscribe now to work on your blue advantage med part d prescriptn drug auth. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800. Blue cross and blue shield of illinois (bcbsil) is continuing to. Web view the list of fep blue focus procedures/dme requiring prior approval. To 9 p.m., eastern time to request prior approval or to obtain a list of drugs and supplies. However, some select drugs require your doctor to provide information about your prescription to determine coverage. This page provides prior approval requirements, contact information, and forms for the federal employee. Web your pharmacy coverage works outside the u.s., too*. For more information about pharmacy prior approval and the required forms visit the prior approval page. Web standard and basic option prior approval list fep blue focus prior approval list. Web fep prior approval documents. Web prior approval must be renewed periodically. Web prior approval pharmacy forms. To 9 p.m., eastern time to request prior approval or to obtain a list of drugs and supplies. Effective on january 1, 2023 updated: 1 results found for search term : For more information about pharmacy prior approval and the required forms visit the prior approval page. Web fep prior approval documents. If you have questions regarding the list,. Web a prior approval is required for the procedures listed below for both the fep standard and basic option plan and the fep blue focus plan. Back cover • changes for 2024:. To obtain a list of these drugs and supplies and to obtain prior approval request forms,. If you have questions regarding the list,. Try it for free now! See the assigned federal brochures. Web approved requests for medications which are subject to prior authorization require additional criteria to be met prior to final validation and coverage determination. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies. For more information about pharmacy prior approval and the required forms visit the prior approval page. Try it for free now! However, some select drugs require your doctor to provide information about your prescription to determine coverage. Please follow the instructions in this document if you disagree with our decision regarding services that require prior approval. Back cover • changes. Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral health (bh) preservice request and review process for. Web 2023 fep blue focus; Web your pharmacy coverage works outside the u.s., too*. For more information about pharmacy prior approval and the required forms visit the prior approval page. See the assigned federal brochures. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800. Web standard and basic option prior approval list fep blue focus prior approval list. *cvs caremark is an independent company that provides pharmacy benefit. Effective on january 1, 2023 updated: 1 results found for search term : Web most drugs are covered without requiring prior approval. Back cover • changes for 2024:. 1 results found for search term : If you have questions regarding the list,. *cvs caremark is an independent company that provides pharmacy benefit. If you have questions regarding the list,. However, some select drugs require your doctor to provide information about your prescription to determine coverage. Web how to file internal and external appeals. Examples of services that may require authorization include the following. Web for members enrolled in basic option and fep blue focus: If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Blue cross and blue shield of illinois (bcbsil) is continuing to make enhancements to its behavioral health (bh) preservice request and review process for. Ad register and subscribe now to work on your blue advantage med part d prescriptn drug auth. To 9 p.m., eastern time to request prior approval or to obtain a list of drugs and supplies. Upload, modify or create forms. Web 2023 fep blue focus; Web most drugs are covered without requiring prior approval. Web view the list of fep blue focus procedures/dme requiring prior approval. Please follow the instructions in this document if you disagree with our decision regarding services that require prior approval. View and download our medical, pharmacy and overseas claim forms. Web your pharmacy coverage works outside the u.s., too*. Effective on january 1, 2023 updated: For more information about pharmacy prior approval and the required forms visit the prior approval page. Web all forms must be signed, then either faxed or mailed. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800.federal bcbs basic overseas claim form 2012 Fill out & sign online
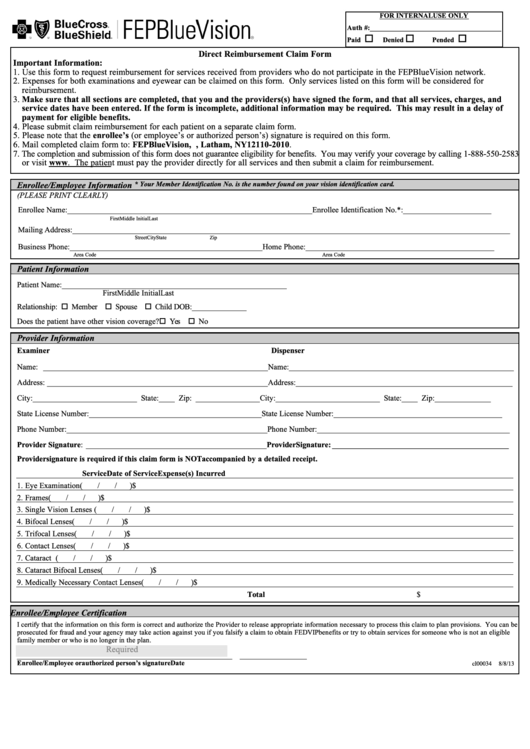
Direct Reimbursement Claim Form Fep Bluevision printable pdf download
Aarp United Healthcare Prior Authorization Form Form Resume
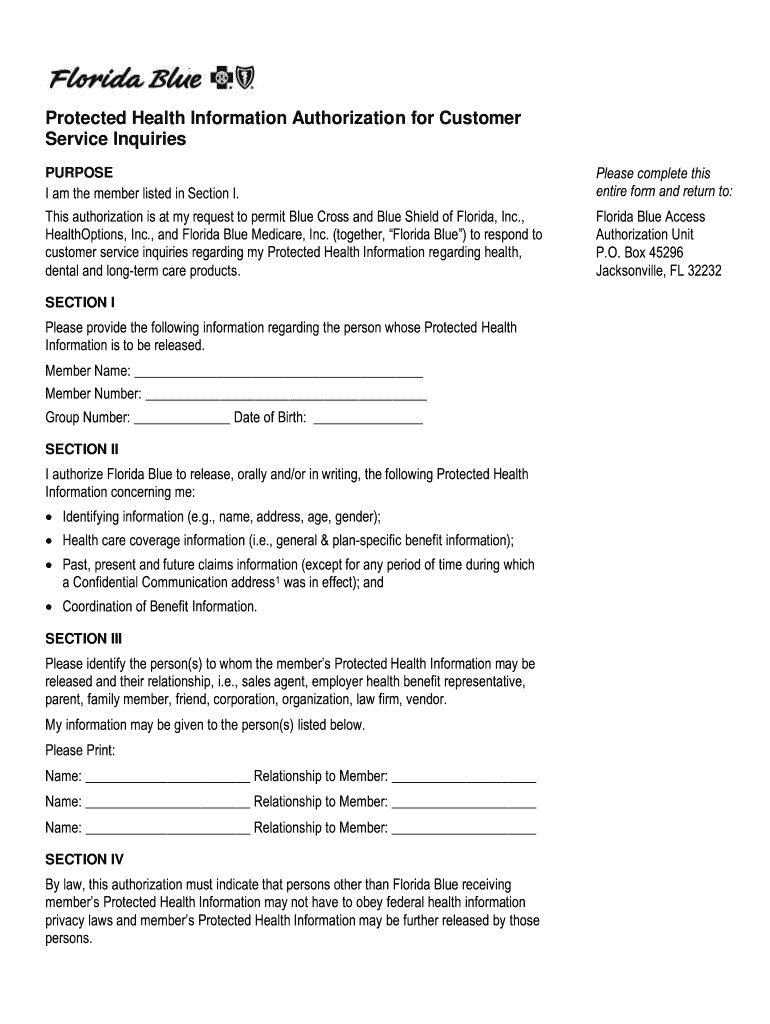
Florida Blue Prior Authorization Form Pdf Fill Out and Sign Printable
Fep Blue Fill Online, Printable, Fillable, Blank pdfFiller
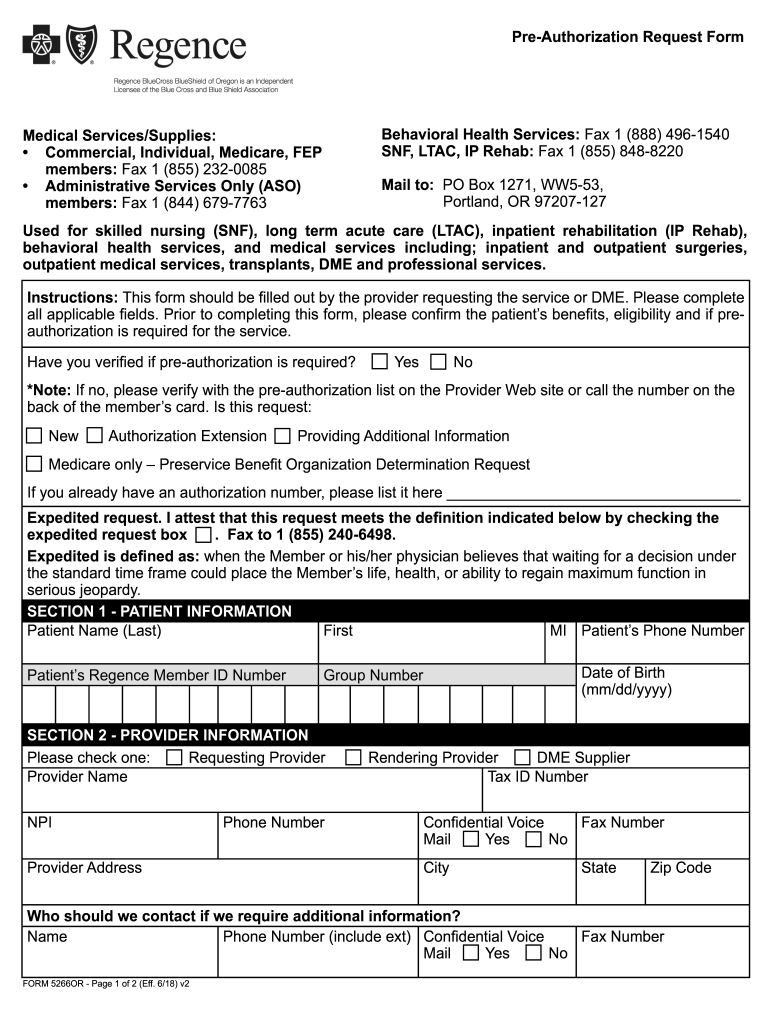
Regence preauthorization form Fill out & sign online DocHub
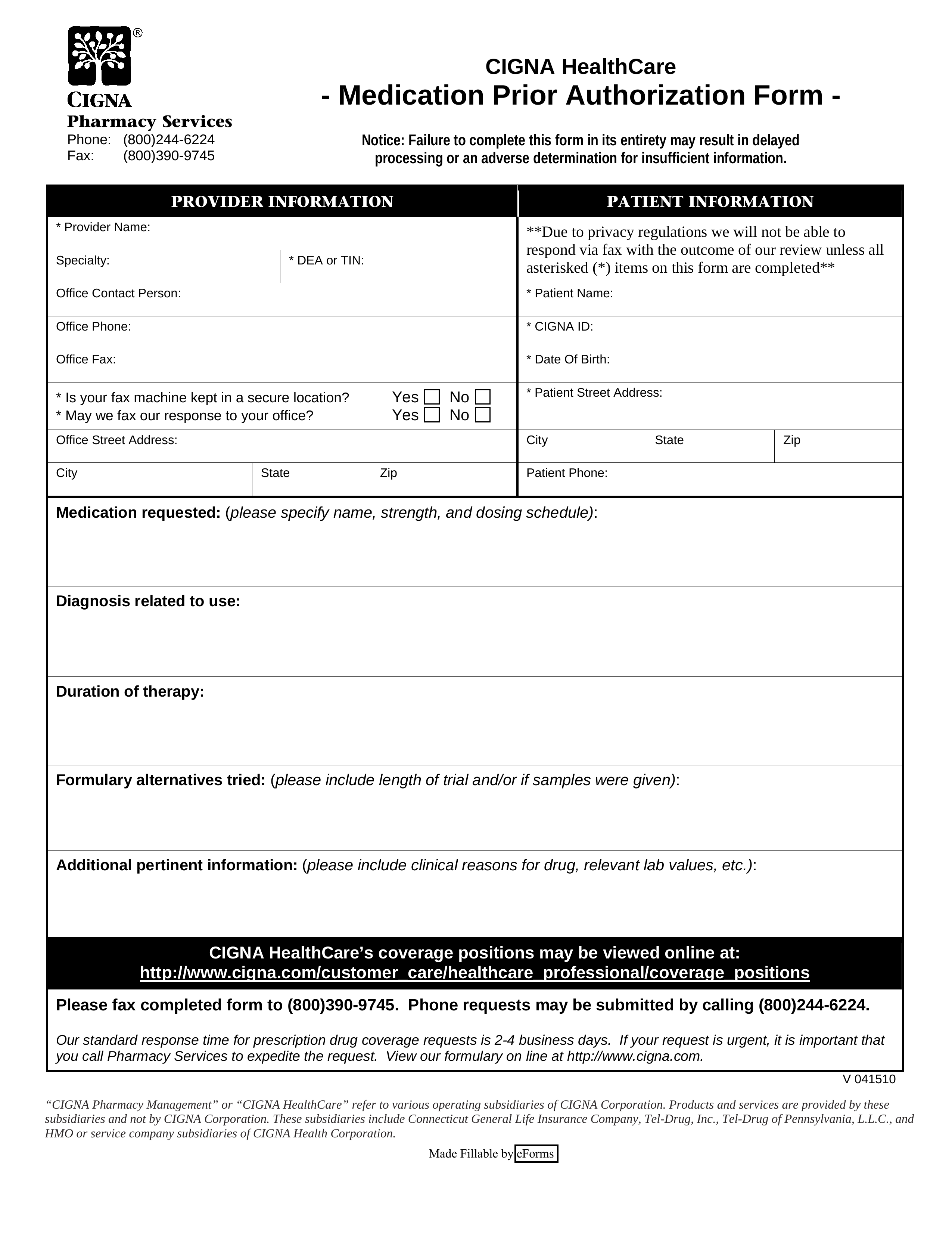
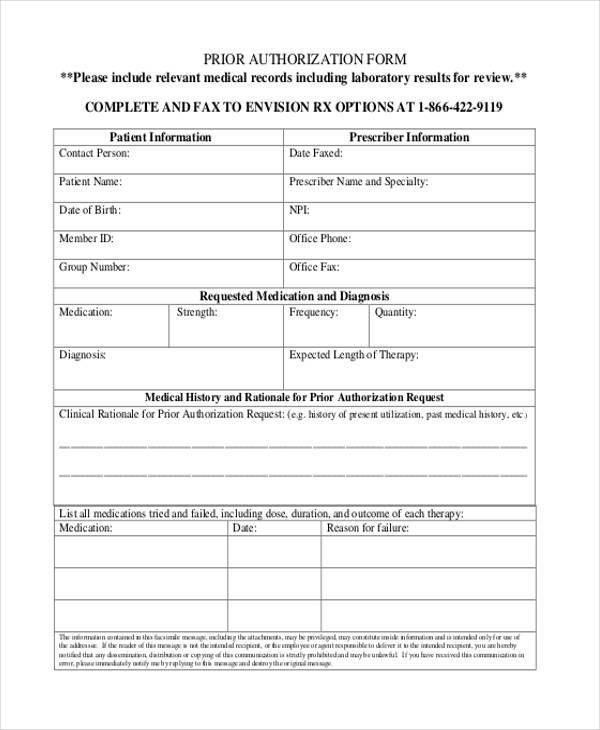
Free Cigna Prior (Rx) Authorization Form PDF eForms
FREE 35+ Sample Authorization Forms in PDF
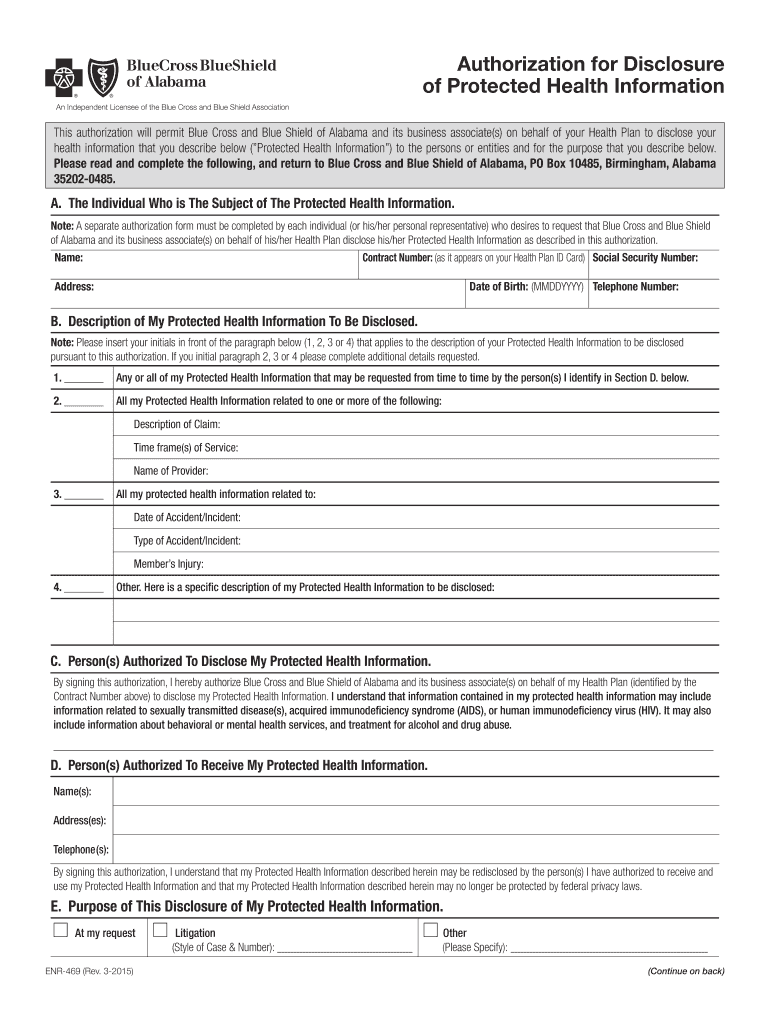
Bcbs alabama authorization form Fill out & sign online DocHub
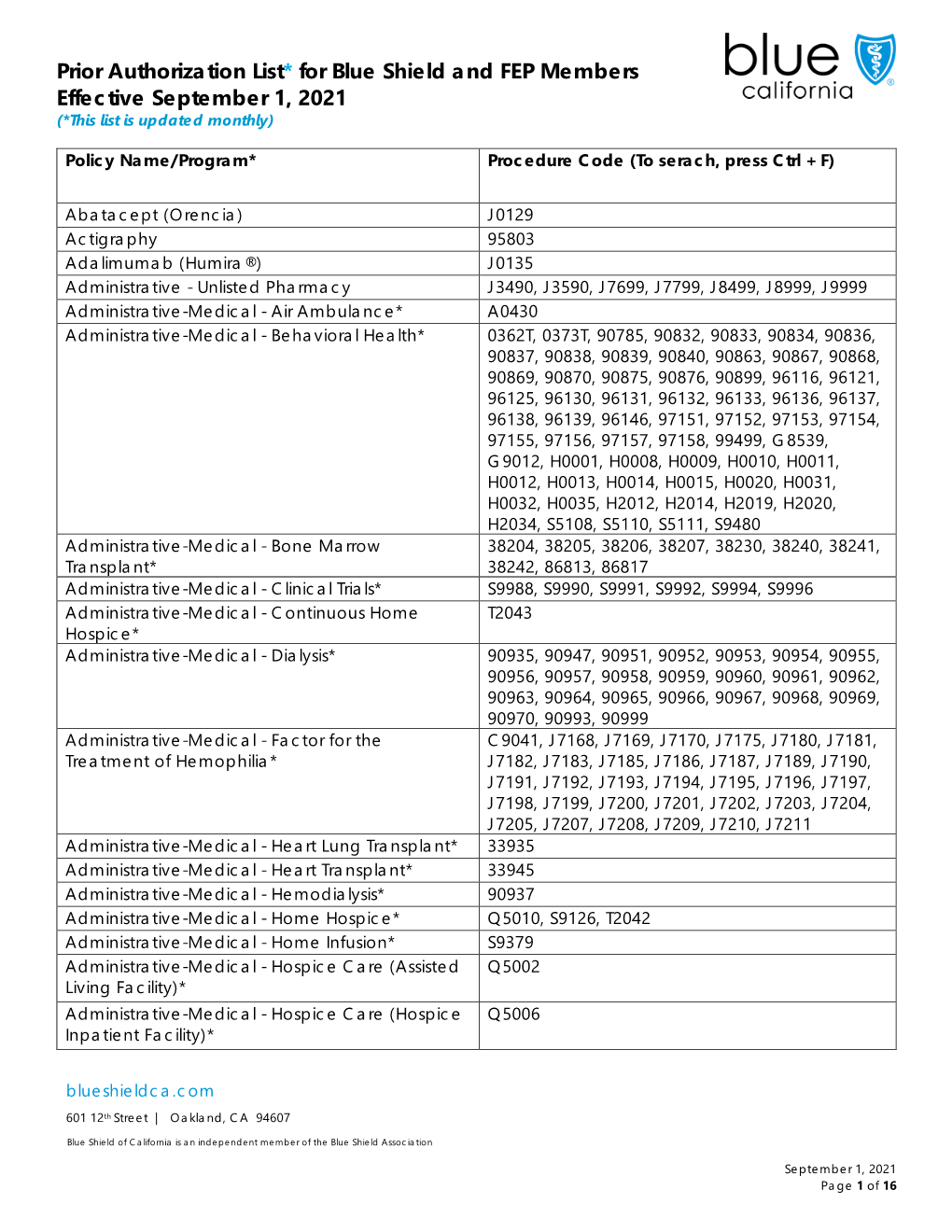
Prior Authorization List* for Blue Shield and FEP Members Effective
Related Post: