Federal Bcbs Prior Authorization Form
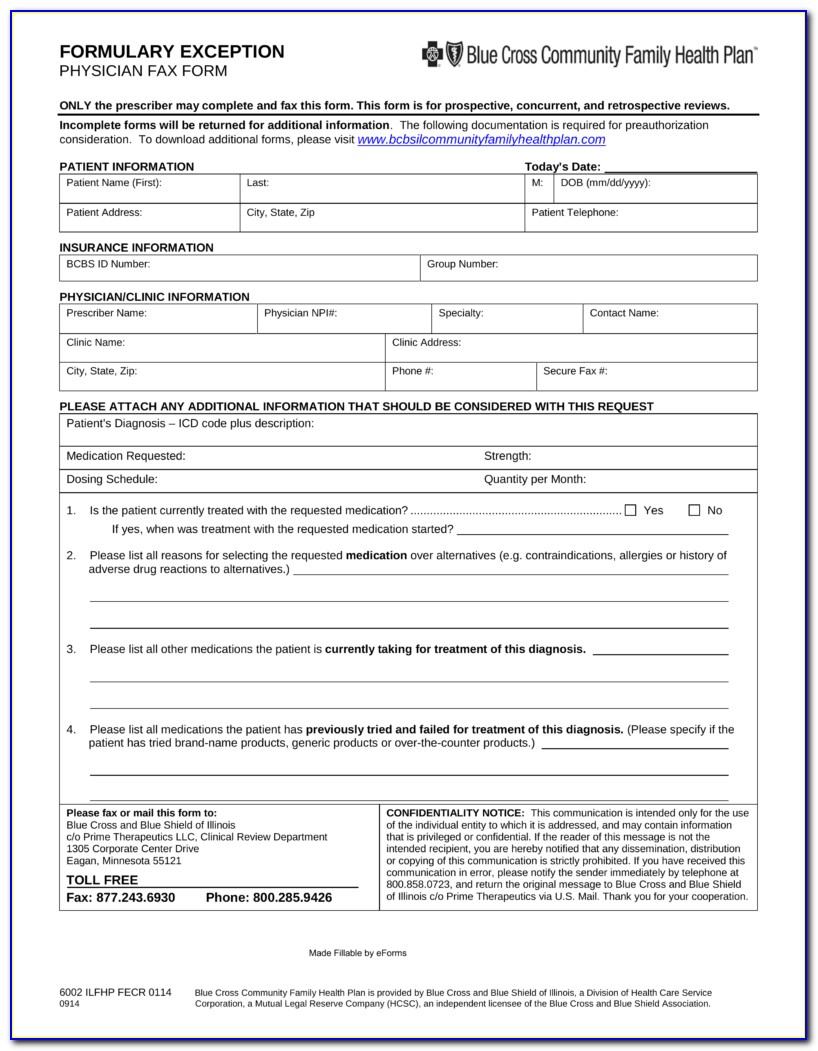
Federal Bcbs Prior Authorization Form - Most preauthorization requests can be resolved by contacting provider relations and. Web prior approval pharmacy forms. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800. Web your healthcare provider can request prior approval electronically, by fax or by mail. Web blue cross blue shield of michigan request for preauthorization form. Web most drugs are covered without requiring prior approval. Original receipts from your doctor, dentist, etc. For more information about pharmacy prior approval and the required forms visit the prior approval page. An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. Web for washington and alaska. Web for washington and alaska. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800. Original receipts from your doctor, dentist, etc. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). However, some select drugs require your doctor to. Web 1 results found for search term : Web prior approval pharmacy forms. Web blue cross blue shield of michigan request for preauthorization form. A copier or scanner to make a copy of each receipt for yourself. An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. Web prior approval pharmacy forms. Find what you need by. Web your healthcare provider can request prior approval electronically, by fax or by mail. Standard and basic option prior approval list. Web 1 results found for search term : Web starting in 2024, members with medicare part a and/or part b will be eligible to enroll in our new medicare part d drug plan that offers additional approved prescription drugs in. Web your pharmacy coverage works outside the u.s., too*. Web 1 results found for search term : Prior approval lists by plan. Most preauthorization requests can be resolved. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Web your pharmacy coverage works outside the u.s., too*. An anthem (blue cross blue shield) prior authorization form is what physicians will use when requesting payment for a patient’s prescription cost. Original receipts from your doctor, dentist, etc. A printer to print the. Standard and basic option prior approval list. If you have questions regarding the list,. Web your pharmacy coverage works outside the u.s., too*. Web this page provides prior approval requirements, contact information, and forms for the federal employee program (fep). Find what you need by. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web starting in 2024, members with medicare part a and/or part b will be eligible to enroll in our new medicare part d drug plan that offers additional approved prescription drugs in. Web 1. Prior approval lists by plan. Web prior approval pharmacy forms. Web your pharmacy coverage works outside the u.s., too*. Effective 1/1/2022, our blue cross and blue shield of texas (bcbstx) federal employee program (fep ®) participants will have some changes to their prior. Web a prior approval is required for the procedures listed below for both the fep standard and. A printer to print the form. Web learn how we manage prior authorization & medical necessity determination requests for certain orthopedic and cardiac services for our fep members. Web most drugs are covered without requiring prior approval. Original receipts from your doctor, dentist, etc. Web prior approval pharmacy forms. View and download our medical, pharmacy and overseas claim forms. Web prior approval must be renewed periodically. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Standard and basic option prior approval list. Prior approval lists by plan. View and download our medical, pharmacy and overseas claim forms. A copier or scanner to make a copy of each receipt for yourself. Web your pharmacy coverage works outside the u.s., too*. A printer to print the form. Original receipts from your doctor, dentist, etc. Effective 1/1/2022, our blue cross and blue shield of texas (bcbstx) federal employee program (fep ®) participants will have some changes to their prior. Prior approval lists by plan. Web blue cross blue shield of michigan request for preauthorization form. If we approve the request for prior approval or precertification, you will be provided with a notice that identifies the approved services and the authorization period. Web 1 results found for search term : Web prior approval must be renewed periodically. Web for washington and alaska. Standard and basic option prior approval list. Most preauthorization requests can be resolved by contacting provider relations and. Web starting in 2024, members with medicare part a and/or part b will be eligible to enroll in our new medicare part d drug plan that offers additional approved prescription drugs in. The full list of drugs that need to be approved, prior approval forms and additional information. Find what you need by. Web learn how we manage prior authorization & medical necessity determination requests for certain orthopedic and cardiac services for our fep members. Web prior approval pharmacy forms. To obtain a list of these drugs and supplies and to obtain prior approval request forms, call the retail pharmacy program at 800.20152022 Blue Advantage BCBS Medicare Part D Prescription Drug
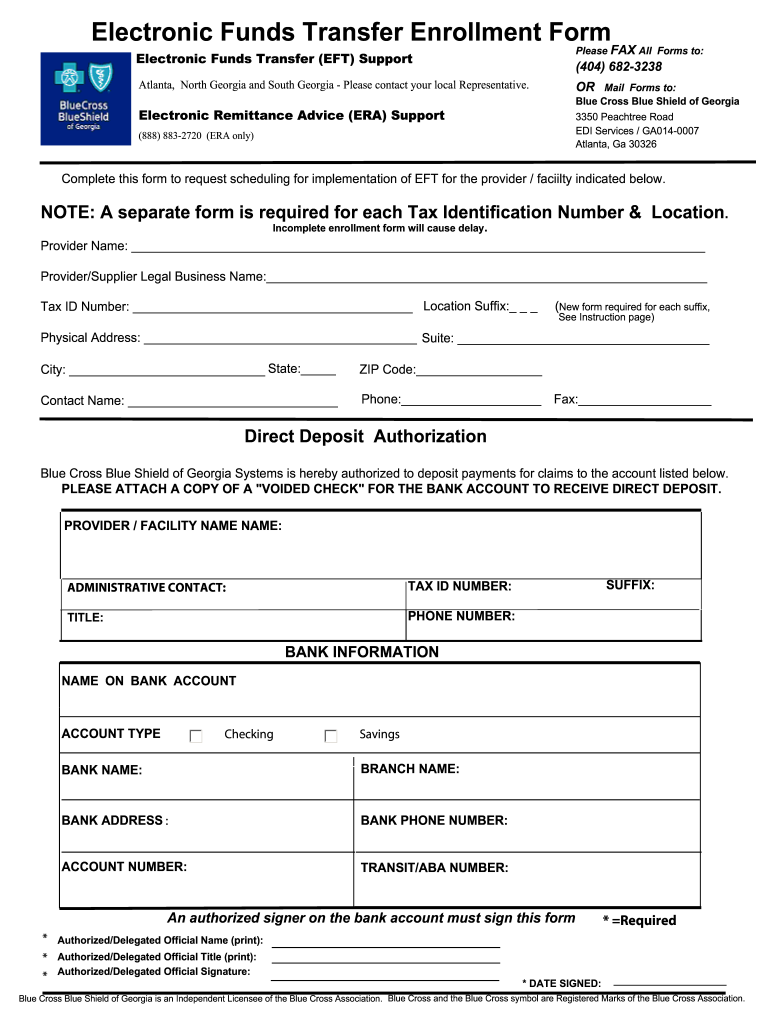
Bcbs Prior Authorization Form PDF Fill Out and Sign Printable PDF
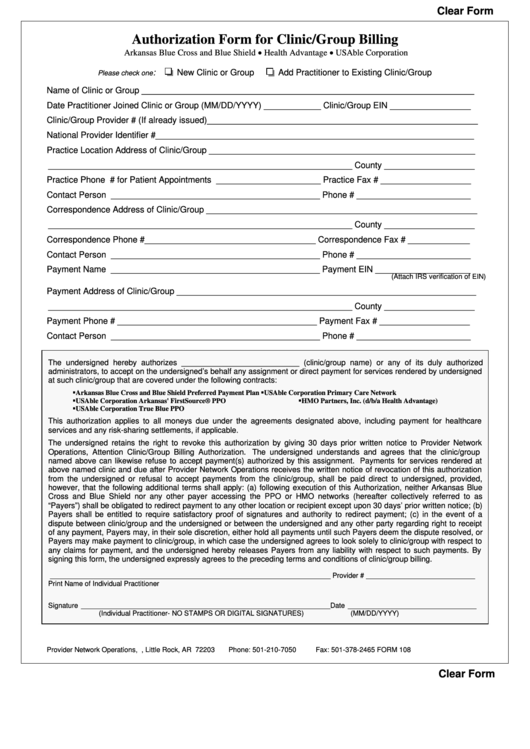
Fillable Bcbs Authorization Form For Clinic/group Billing printable pdf
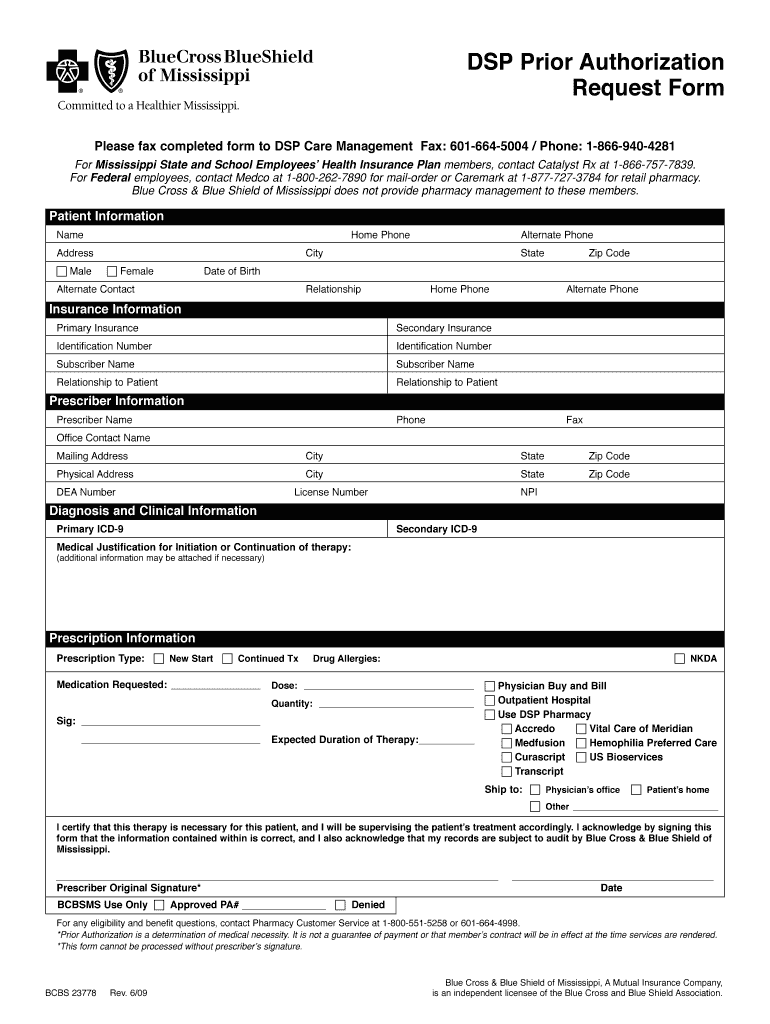
Bcbs Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Empire Blue Cross Blue Shield Authorization To Release Information
20182022 Form CareFirst BCBS CUT01241E Fill Online, Printable
Ms bcbs claim Fill out & sign online DocHub
Free New York Medicaid Prior Authorization Form PDF eForms
Bcbs Prior Authorization Form Form Resume Examples NRE34PV36x
Related Post: