Carefirst Prior Authorization Form For Medication
Carefirst Prior Authorization Form For Medication - To submit a prior authorization request online, log in to the provider portal and navigate to the prior auth/notifications tab. Web prior authorization from carefirst is required. Web up to $40 cash back the purpose of the care1st prior authorization form is to obtain approval from the insurance provider, care1st, for certain medical services, prescription. Web to request a brand exception: Web how to submit a drug prior authorization. Before you fill prescriptions for certain drugs. We require you or your physician to get prior authorization for certain drugs. Web •indiana health coverage programs (ihcp) universal pa form not required when utilizing portal preferred method of submission •ihcp universal pa form is still required. We require you or your physician to get prior authorization for certain drugs. To make an appropriate determination, providing the most. Web attend a live webinar to learn more. This means that you will need to get approval from carefirst before you Web if you prefer, download our request for a medicare prescription drug coverage determination to request a prior authorization, tiering exception, or to request coverage. Web prior authorization requests for drugs covered under the medical benefit must be submitted. Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst. Web up to $40 cash back the purpose of the care1st prior authorization form is to obtain approval from the insurance provider, care1st, for certain medical services, prescription. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically. Certificate of medical necessity (cmn) attached. We require you or your physician to get prior authorization for certain drugs. To submit a prior authorization request online, log in to the provider portal and navigate to the prior auth/notifications tab. For more information, please complete our. Web •indiana health coverage programs (ihcp) universal pa form not required when utilizing portal preferred. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. We require you or your physician to get prior authorization for certain drugs. Web carefirst's medicare advantage prescription drug faqs. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web. Web up to $40 cash back the purpose of the care1st prior authorization form is to obtain approval from the insurance provider, care1st, for certain medical services, prescription. This means that you will need to get approval from carefirst before you. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered.. To make an appropriate determination, providing the most. To submit a prior authorization request online, log in to the provider portal and navigate to the prior auth/notifications tab. Your doctor may need to provide some of your medical history or laboratory tests. This means that you will need to get approval from carefirst before you. Web carefirst's medicare advantage prescription. This fax machine is located in a secure location as required by. To make an appropriate determination, providing the most. Web to request a brand exception: Web up to $40 cash back the purpose of the care1st prior authorization form is to obtain approval from the insurance provider, care1st, for certain medical services, prescription. Prior authorization requests for drugs covered. Web prior authorization preferred drug list quantity limits step therapy generic substitution preventive drugs travel coverage expand all | collapse all general information do i. Web prior authorization from carefirst is required. Web prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal. For more information, please complete our. Web •indiana. This fax machine is located in a secure location as required by. Before you fill prescriptions for certain drugs. This means that you will need to get approval from carefirst before you Web how to submit a drug prior authorization. Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst provider portal . Approval in advance to get certain drugs that may or may not be on our formulary. This fax machine is located in a secure location as required by. To make an appropriate determination, providing the most. Before you fill prescriptions for certain drugs. Web prior authorization from carefirst is required. To submit a prior authorization request online, log in to the provider portal and navigate to the prior auth/notifications tab. Web attend a live webinar to learn more. Web prior authorization preferred drug list quantity limits step therapy generic substitution preventive drugs travel coverage expand all | collapse all general information do i. Web carefirst's medicare advantage prescription drug faqs. To make an appropriate determination, providing the most. This upgrade was released in 2021 for medicare advantage (ma) members and is now available for commercial and fep members. Certificate of medical necessity (cmn) attached. Web up to $40 cash back the purpose of the care1st prior authorization form is to obtain approval from the insurance provider, care1st, for certain medical services, prescription. A prior authorization means we need clinical information from your prescriber before we can pay for your. This means that you will need to get approval from carefirst before you. To make an appropriate determination, providing the most. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. For more information, please complete our. We require you or your physician to get prior authorization for certain drugs. We require you or your physician to get prior authorization for certain drugs. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web how to submit a drug prior authorization. Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the carefirst. Web to request a brand exception: Before you fill prescriptions for certain drugs.CareFirst BCBS CUT01241E 2018 Fill and Sign Printable Template
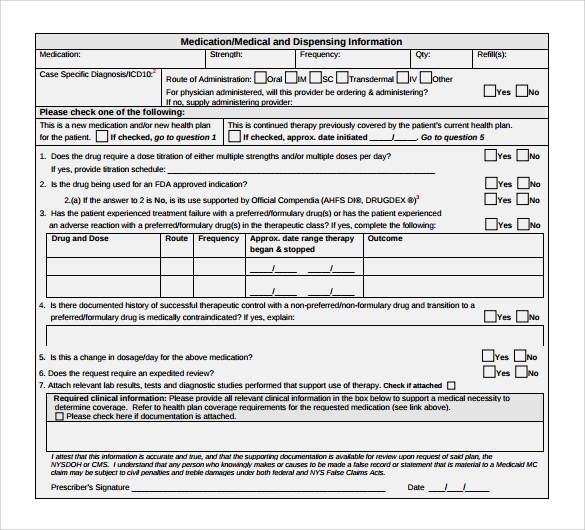
9+ Sample Caremark Prior Authorization Forms Sample Templates
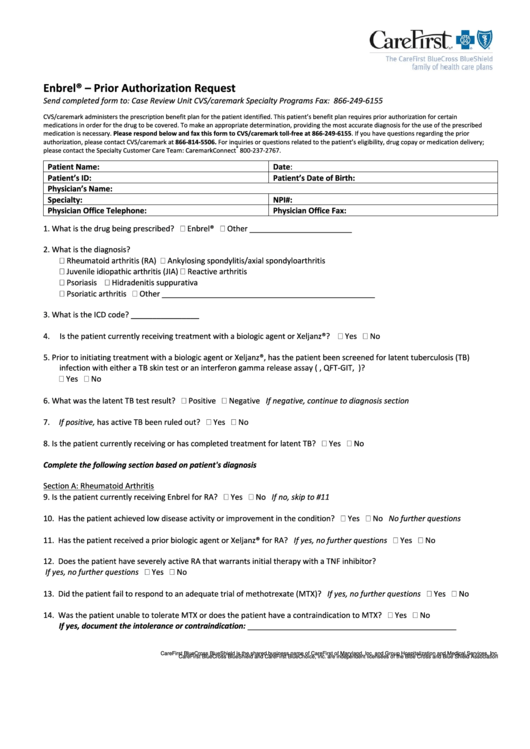
Carefirst Prior Authorization Request Enbrel printable pdf download
FREE 10+ Sample Medical Authorization Forms in PDF MS Word Excel
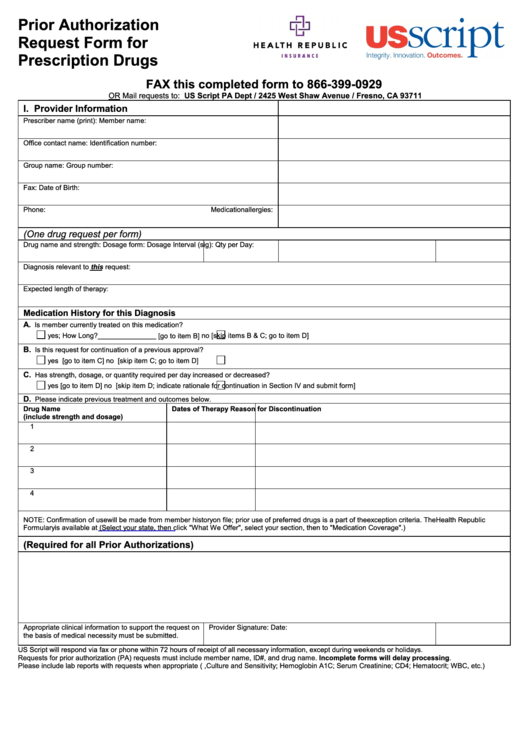
Prior Authorization Request Form For Prescription Drugs Us Script
Medicare Generation Rx Prior Authorization Form Form Resume
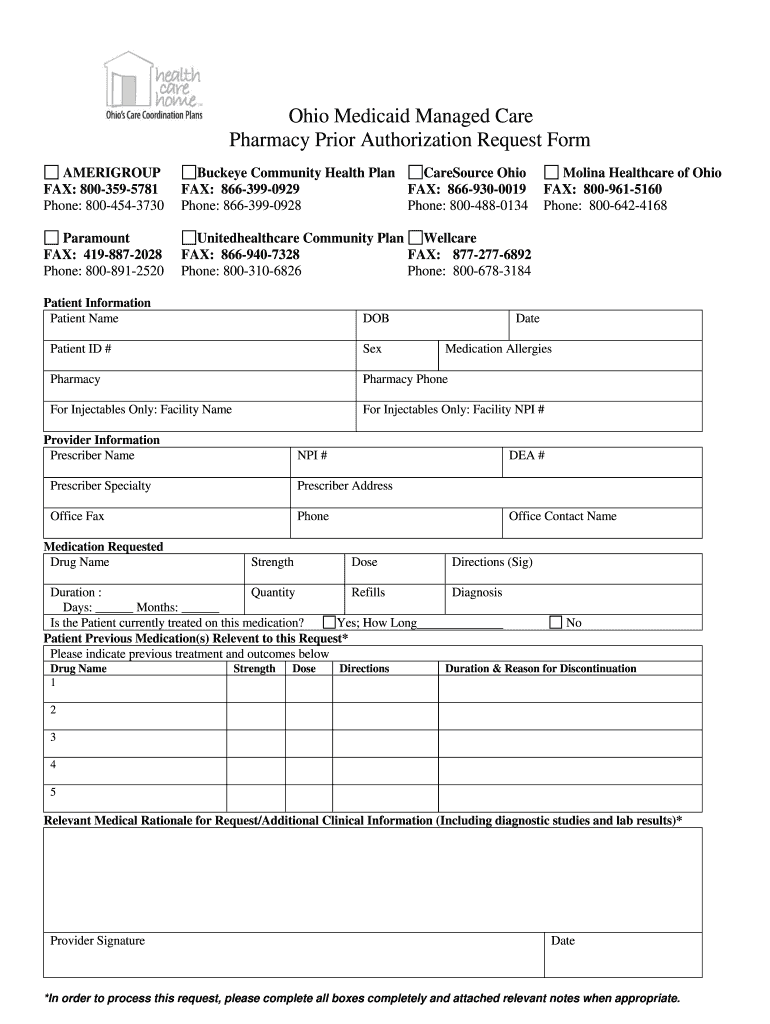
OH Medicaid Managed Care Pharmacy Prior Authorization Request Form
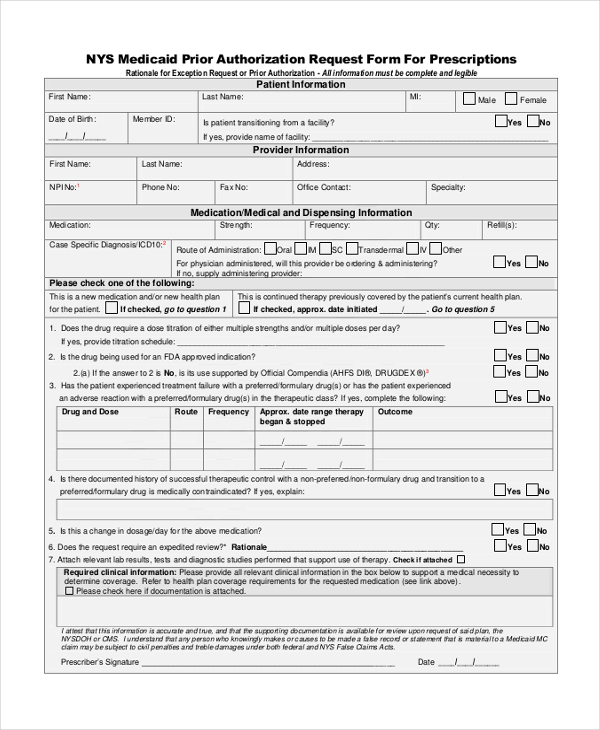
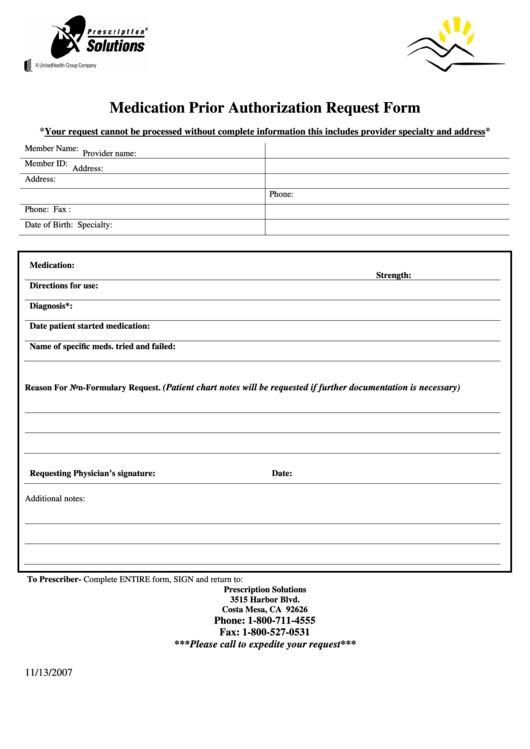
Medication Prior Authorization Request Form printable pdf download
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
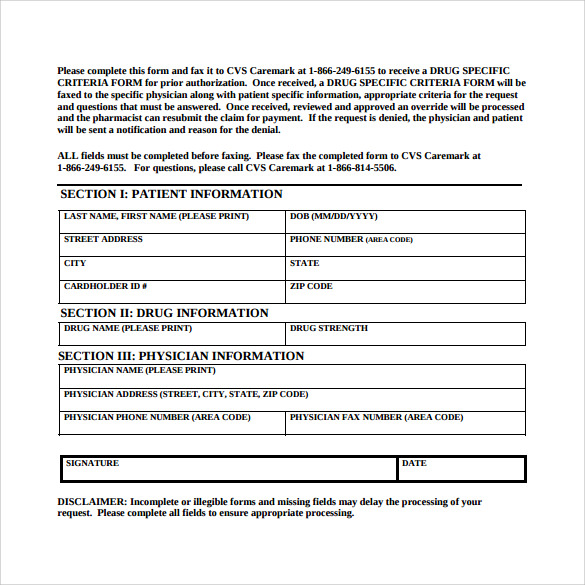
FREE 8+ Sample Caremark Prior Authorization Forms in PDF
Related Post: