Blueadvantagearkansas Prior Authorization Form
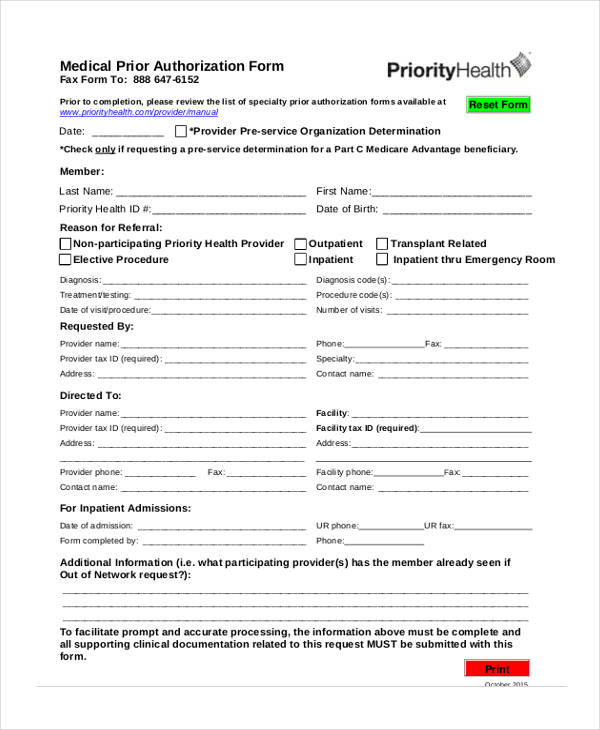
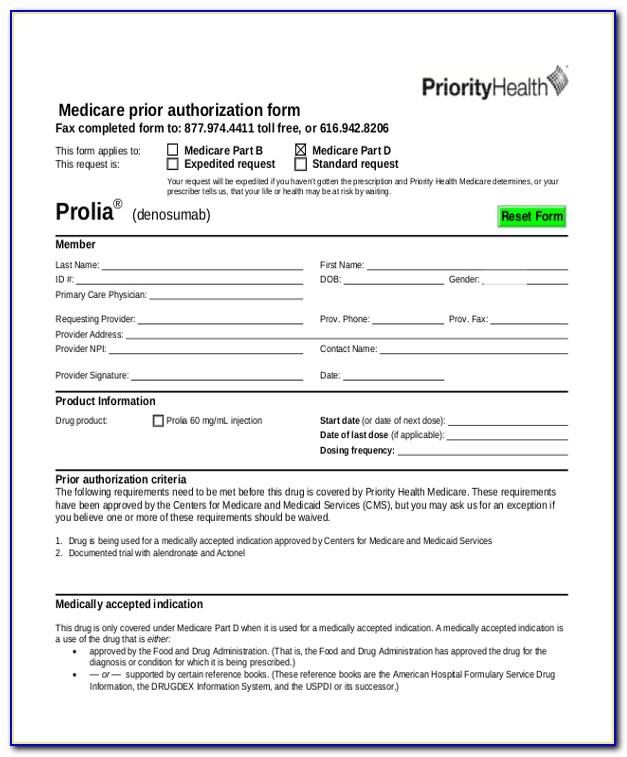
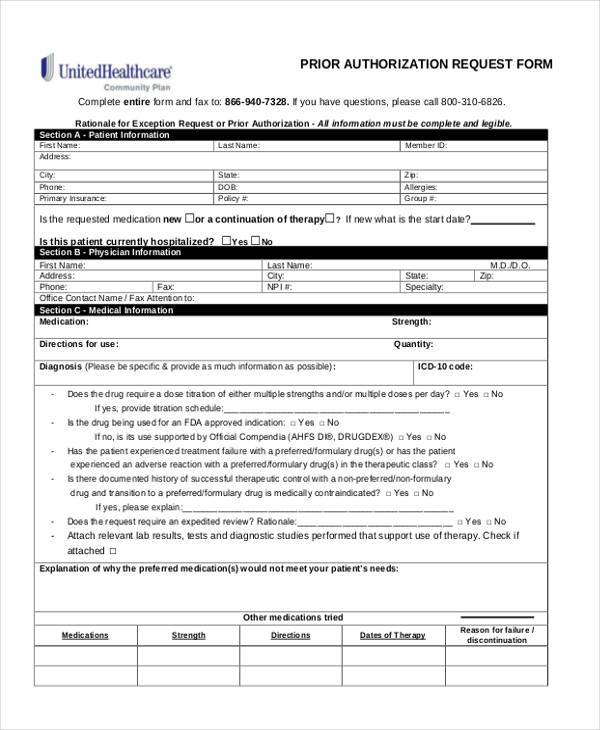
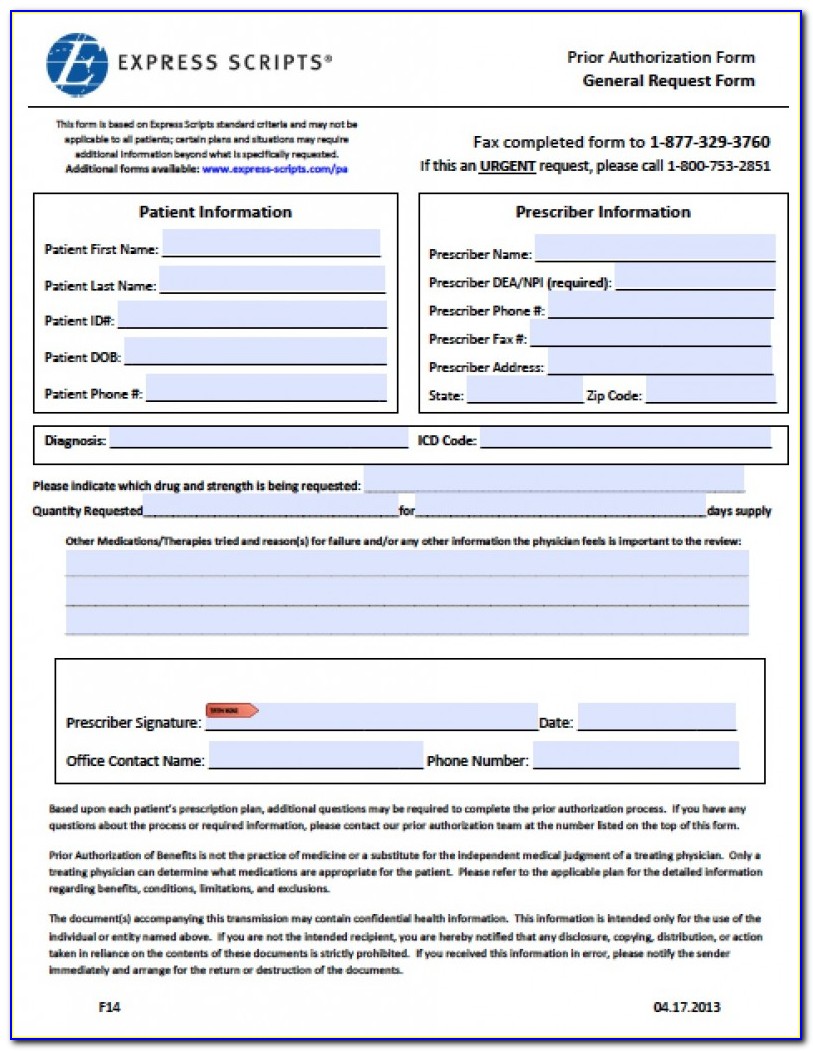
Blueadvantagearkansas Prior Authorization Form - Web arkansas blue cross medicare advantage prior authorization request form access forms for dental providers. Referral process for primary care network; Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Web blueadvantage | documents and forms web content viewer documents & forms we've put together the most common documents and forms you might need for things like filing. Please allow 72 hours for review and acknowledgement of initial receipt. Web prior approval program information. Web ***note*** a prior authorization will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with. Web •indiana health coverage programs (ihcp) universal pa form not required when utilizing portal preferred method of submission •ihcp universal pa form is still required. Discover a wide selection of options to meet your insurance. Please fax or mail responses to: Web providers who are requesting a prior approval for walmart or other blueadvantage members should use the appropriate form from the blueadvantage website. Web ***note*** a prior authorization will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with. Web prior authorization form for requested services [pdf] for tyson or walmart. Please check with your human resources office before using one of these forms. Looking for the best in health insurance in arkansas? Web prior authorization form for requested services [pdf] for tyson or walmart members, please use the courtesy review form. Arkansas blue cross medicare advantage prior authorization request form [pdf] medicare advantage prior authorization list. Web ***note*** a prior. Please check with your human resources office before using one of these forms. Health information network (hin) hedis measures; Web blueadvantage inpatient admissions shield association and is licensed to offer health plans in all 75 counties of arkansas. Provider application/contract request [pdf] use. Web blueadvantage | documents and forms web content viewer documents & forms we've put together the most. Bluecard® program urac accreditation transparency and. Web providers who are requesting a prior approval for walmart or other blueadvantage members should use the appropriate form from the blueadvantage website. Health information network (hin) hedis measures; Web prior authorization you can look up cpt or hcpcs codes to determine if a medical, surgical, or diagnostic service requires prior authorization for a. Web medicare advantage prior authorization. Discover a wide selection of options to meet your insurance. Provider application/contract request [pdf] use. Web prior authorization applies to both brand and generic products. Looking for the best in health insurance in arkansas? Web form not applicable for blueadvantage members this form may only be utilized to submit a request for a service that requires prior approval. Health information network (hin) hedis measures; Web prior authorization you can look up cpt or hcpcs codes to determine if a medical, surgical, or diagnostic service requires prior authorization for a horizon member. Web prior authorization. Web arkansas blue cross medicare advantage prior authorization request form access forms for dental providers. Discover a wide selection of options to meet your insurance. This review consists of checking clinical documentation to verify the. Web blueadvantage inpatient admissions shield association and is licensed to offer health plans in all 75 counties of arkansas. Provider application/contract request [pdf] use. Some employers use customized forms or electronic systems. Web blueadvantage | documents and forms web content viewer documents & forms we've put together the most common documents and forms you might need for things like filing. Web prior authorization applies to both brand and generic products. Web providers who are requesting a prior approval for walmart or other blueadvantage members. Web prior authorization medications
this is not a comprehensive list of covered medications. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Provider application/contract request [pdf] use. Web a confidential, electronic medical record with information available from medical claims and testing, combined. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Referral process for primary care network; Web form not applicable for blueadvantage members this form may only be utilized to submit a request for a service that requires prior approval. Web arkansas blue. Looking for the best in health insurance in arkansas? Web prior authorization form for requested services [pdf] for tyson or walmart members, please use the courtesy review form. Provider application/contract request [pdf] use. Web ***note*** a prior authorization will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with. Web form not applicable for blueadvantage members this form may only be utilized to submit a request for a service that requires prior approval. Some employers use customized forms or electronic systems. Web prior authorization you can look up cpt or hcpcs codes to determine if a medical, surgical, or diagnostic service requires prior authorization for a horizon member. Web prior authorization medications
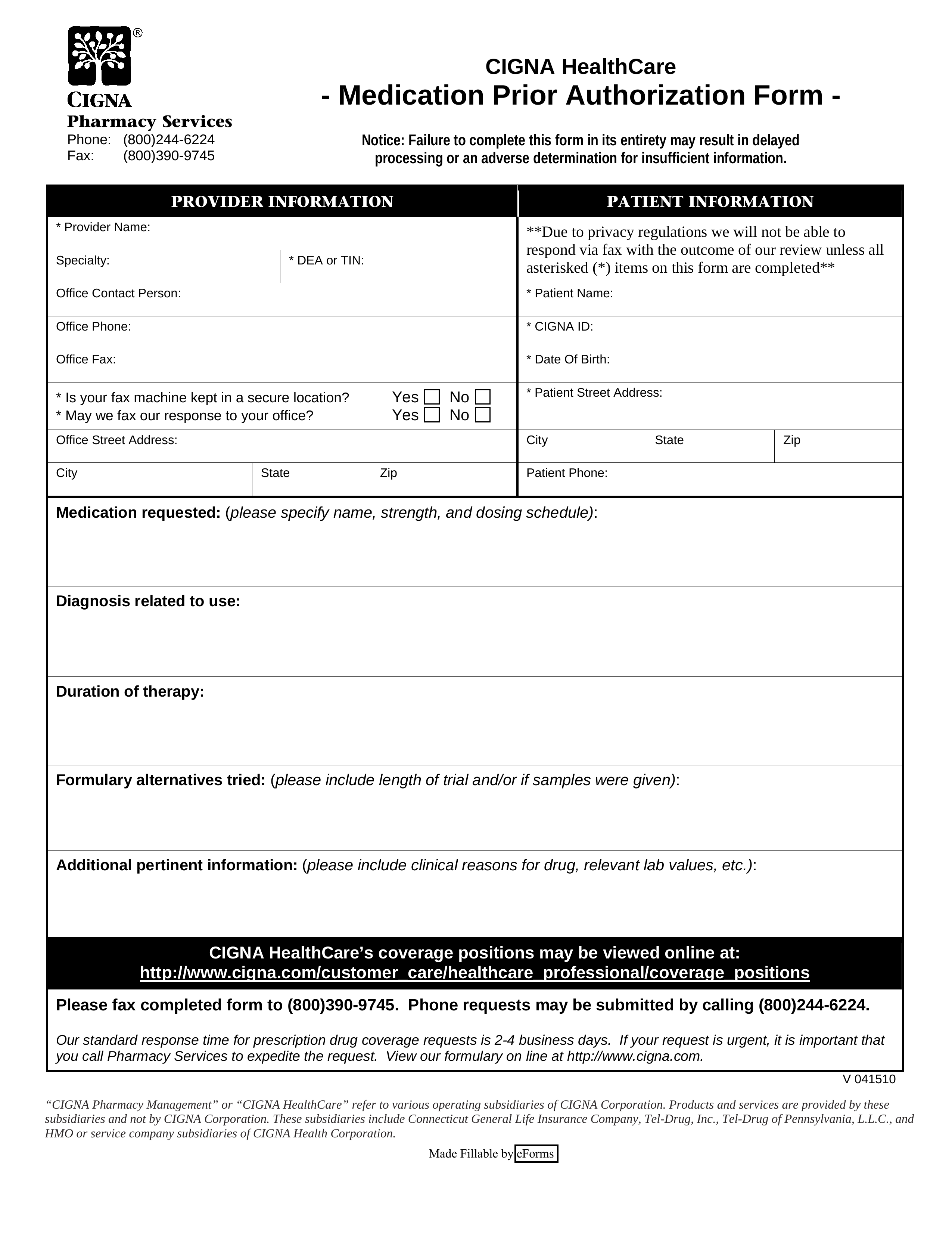
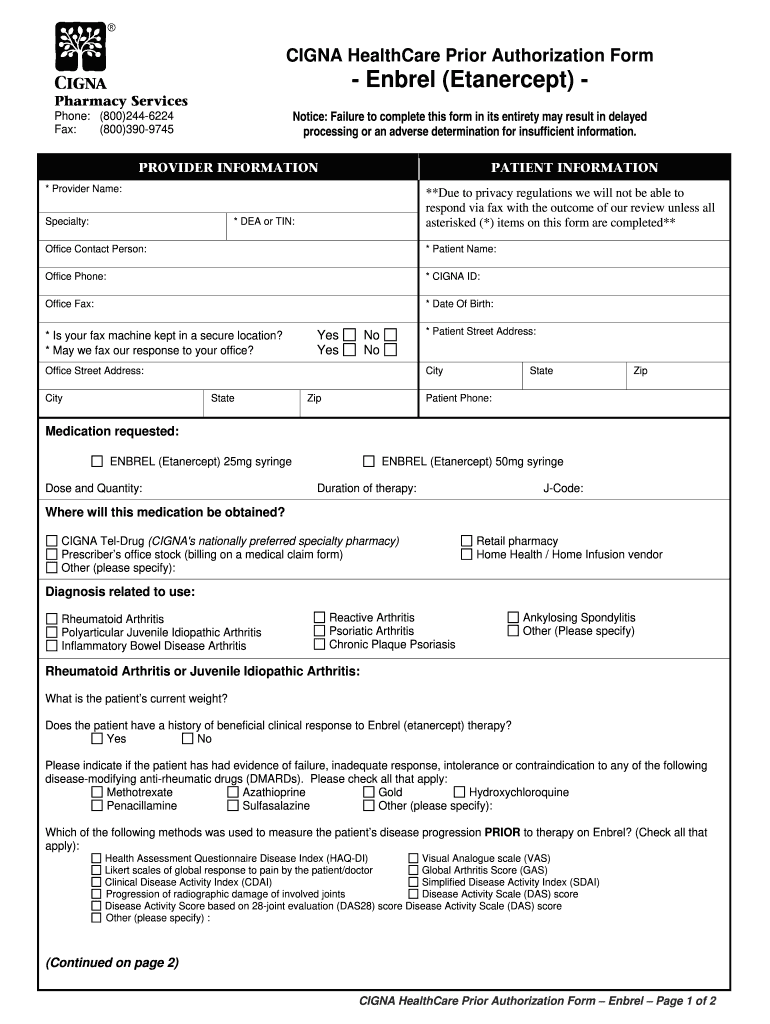
this is not a comprehensive list of covered medications. Referral process for primary care network; Web prior authorization applies to both brand and generic products. Web aligning with the adoption of the mbm, chapter ii, section 60, medical supplies and dme rule, the office of mainecare services (oms) will be updating the. Web prior approval program information. Web providers who are requesting a prior approval for walmart or other blueadvantage members should use the appropriate form from the blueadvantage website. This review consists of checking clinical documentation to verify the. Web ***note*** a prior approval will only be considered when complete medical records and a treatment plan or letter of medical necessity are submitted with this request. Please fax or mail responses to: Web blueadvantage inpatient admissions shield association and is licensed to offer health plans in all 75 counties of arkansas. Discover a wide selection of options to meet your insurance. Web yes no please attach medical records, treatment plan, and any relevant clinical documentation to support the request. Certain medications that require prior authorization based on age, gender or quantity limit specifications are not.Free Cigna Prior (Rx) Authorization Form PDF eForms
Surescripts Prior Auth Printable Form Printable Form, Templates and
How To Write A Prior Authorization Letter
Free Idaho Medicaid Prior (Rx) Authorization Form PDF eForms
Medco Prior Auth Form Medication Form Resume Examples q25Z4Lxk0o
20152023 Blue Advantage BCBS Medicare Part D Prescription Drug
FREE 35+ Sample Authorization Forms in PDF
20152022 HI Standardized Prescription Drug Prior Authorization Form
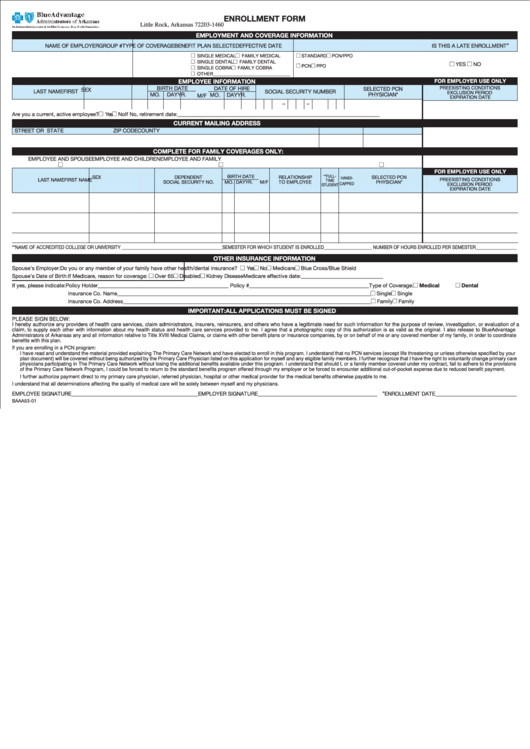
Enrollment Form Blue Advantage, Arkansas printable pdf download
Medco Prior Auth Form Medication Form Resume Examples q25Z4Lxk0o
Related Post: