Blue Cross Blue Shield Of Texas Prior Authorization Form
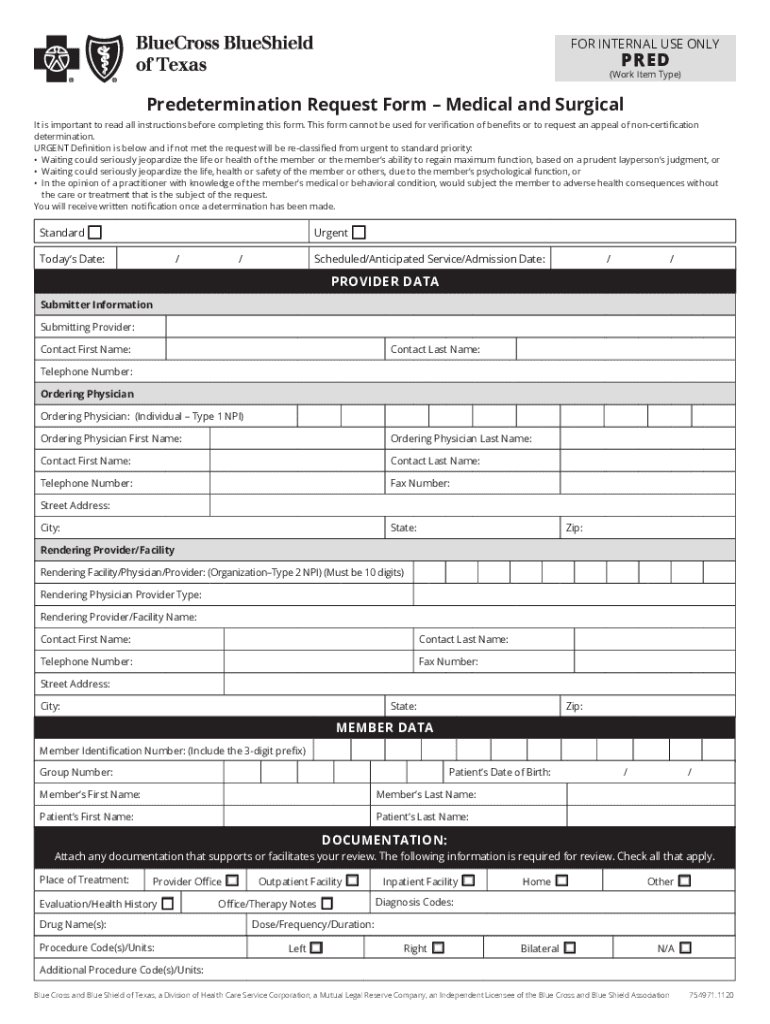
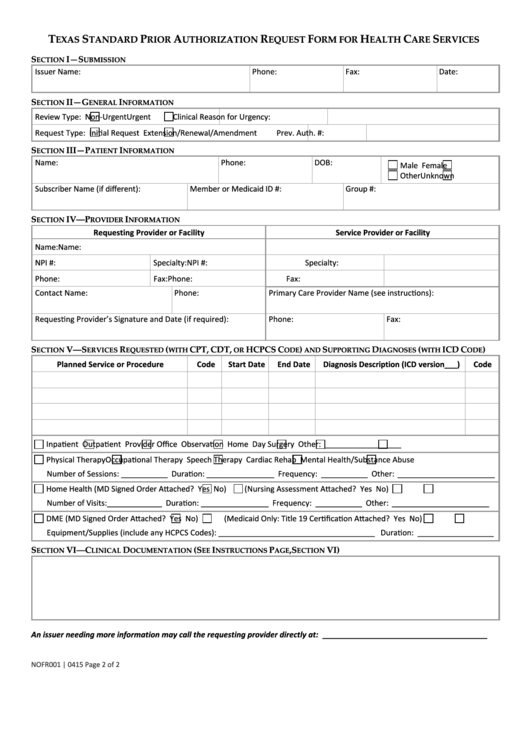
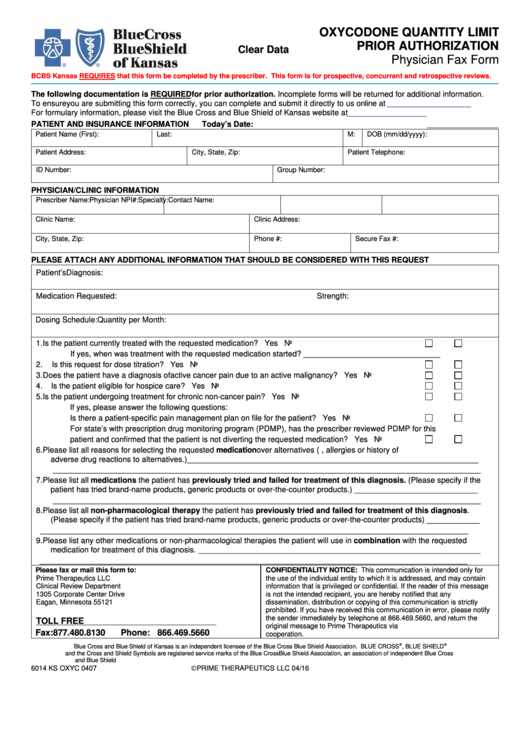
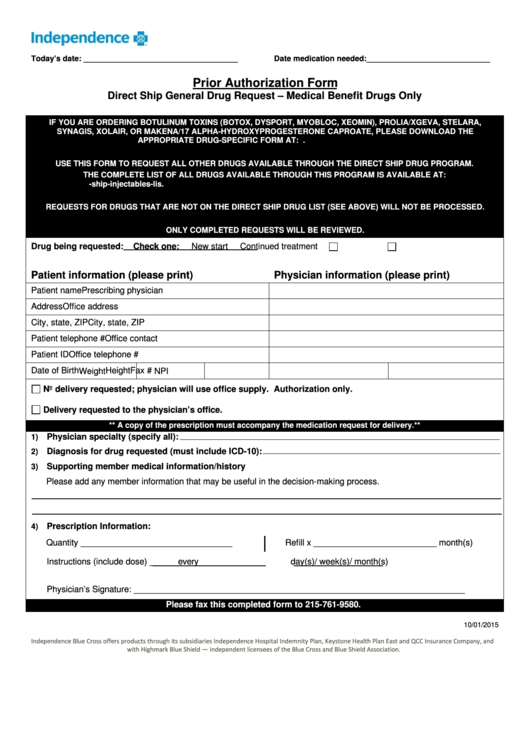
Blue Cross Blue Shield Of Texas Prior Authorization Form - Web ealth benefit plan issuers must accept the texas standard prior authorization request form for prescription drug benefits if the plan requires prior authorization of a. Web many times, your doctor will need to get approval — prior authorization — before your plan will cover certain health care services and medicines. This is called a prior authorization. Ad pdffiller.com has been visited by 1m+ users in the past month Required on some medications before your drug will be covered. A prior authorization is the. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. Web as a ppo/pos, hmo or traditional contracted provider with blue cross and blue shield of texas, you are responsible for the completion of the prior authorization process for. Web prior authorization services for fully insured and aso; Do not use this form to: Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. If your health plan's formulary guide indicates that you need a prior authorization for a. Select the patient registration menu option, choose. Do not use this form to: Web the specific effective. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. Sometimes you may need to get approval from blue cross and blue shield of texas (bcbstx) before we will cover certain inpatient, outpatient. Prior authorization requirements apply to all. Web ealth benefit. Access and download these helpful bcbstx health. Web what is prior authorization? A prior authorization is the. Prior authorization requirements apply to all. Prior authorizations lists for blue cross medicare advantage (ppo) and blue cross medicare advantage (hmo). Do not use this form to: Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. Select the patient registration menu option, choose. Web 08/21/2023, updated 09/29/2023 & 10/16/2023. If your health plan's formulary guide indicates that you need a prior authorization. Web continuity of care request form (request for continued access for providers) international claim form standard authorization form with instructions nominate a. Ad pdffiller.com has been visited by 1m+ users in the past month Web electronically, through the issuer’s portal, to request prior authorization of a prescription drug benefit. To view this information, visit the general reimbursement information section on. Prior authorization requirements apply to all. Prescription drug claim form texas standard prior authorization request form for prescription drug benefits Emergency or urgent care does not require authorization. A referral is a written order from your primary care provider (pcp) for you to see a specialist. Bcbstx must approve certain covered health services before you get them. If your health plan's formulary guide indicates that you need a prior authorization for a. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. Web 08/21/2023, updated 09/29/2023 & 10/16/2023. Referrals are required under the healthselect of texas ® plan. Web. To view this information, visit the general reimbursement information section on the. Web ealth benefit plan issuers must accept the texas standard prior authorization request form for prescription drug benefits if the plan requires prior authorization of a. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before. Select the patient registration menu option, choose. Web 08/21/2023, updated 09/29/2023 & 10/16/2023. A referral is a written order from your primary care provider (pcp) for you to see a specialist. Bcbstx must approve certain covered health services before you get them. Web continuity of care request form (request for continued access for providers) international claim form standard authorization form. Ad pdffiller.com has been visited by 1m+ users in the past month Prior authorizations lists for blue cross medicare advantage (ppo) and blue cross medicare advantage (hmo). Web what is prior authorization? Web 08/21/2023, updated 09/29/2023 & 10/16/2023. Web drug specific prior authorization form; If your health plan's formulary guide indicates that you need a prior authorization for a. Ad pdffiller.com has been visited by 1m+ users in the past month Prior authorization requirements apply to all. Prior authorizations lists for blue cross medicare advantage (ppo) and blue cross medicare advantage (hmo). Prescription drug claim form texas standard prior authorization request form for prescription drug benefits Web electronically, through the issuer’s portal, to request prior authorization of a prescription drug benefit. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. A prior authorization is the. Web drug specific prior authorization form; Referrals are required under the healthselect of texas ® plan. Web submitting online prior authorization requests using this new tool is easy and consists of only five steps: Sometimes you may need to get approval from blue cross and blue shield of texas (bcbstx) before we will cover certain inpatient, outpatient. Web ealth benefit plan issuers must accept the texas standard prior authorization request form for prescription drug benefits if the plan requires prior authorization of a. Web emergency care and urgent care. Web the specific effective date will be noted for each change that is posted. Covermymeds is bluecross blueshield of texas prior authorization forms’s. Web as a ppo/pos, hmo or traditional contracted provider with blue cross and blue shield of texas, you are responsible for the completion of the prior authorization process for. To view this information, visit the general reimbursement information section on the. Web 08/21/2023, updated 09/29/2023 & 10/16/2023. Select the patient registration menu option, choose.Bcbs Predetermination Form Fill Out and Sign Printable PDF Template
CA Blue Shield Prior Authorization Request Form Testing Fill
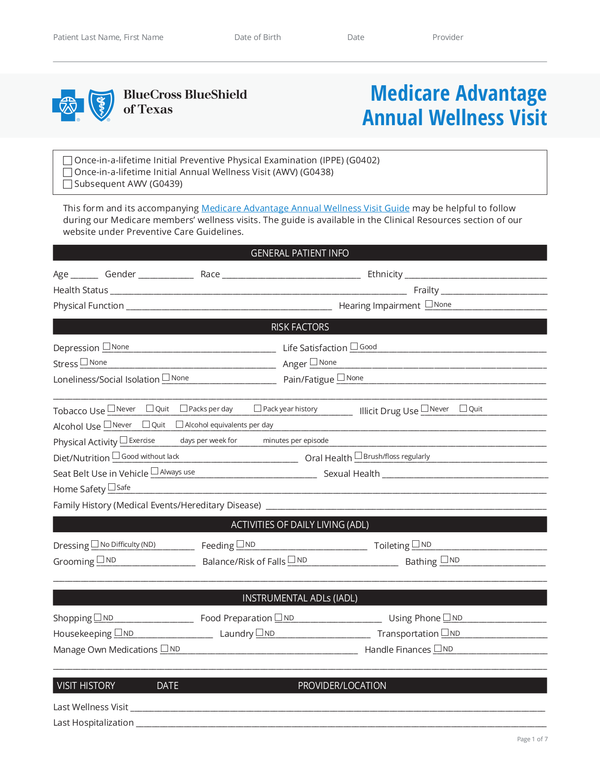
Fill Free fillable Blue Cross and Blue Shield of Texas PDF forms
Fillable Texas Standard Prior Authorization Request Form For Health
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates free
Fill Free fillable Blue Cross and Blue Shield of Texas PDF forms
Prior Authorization Form Independence Blue Cross printable pdf download
Fill Free fillable Blue Cross and Blue Shield of Texas PDF forms
Free pdf form filler google ladertennis
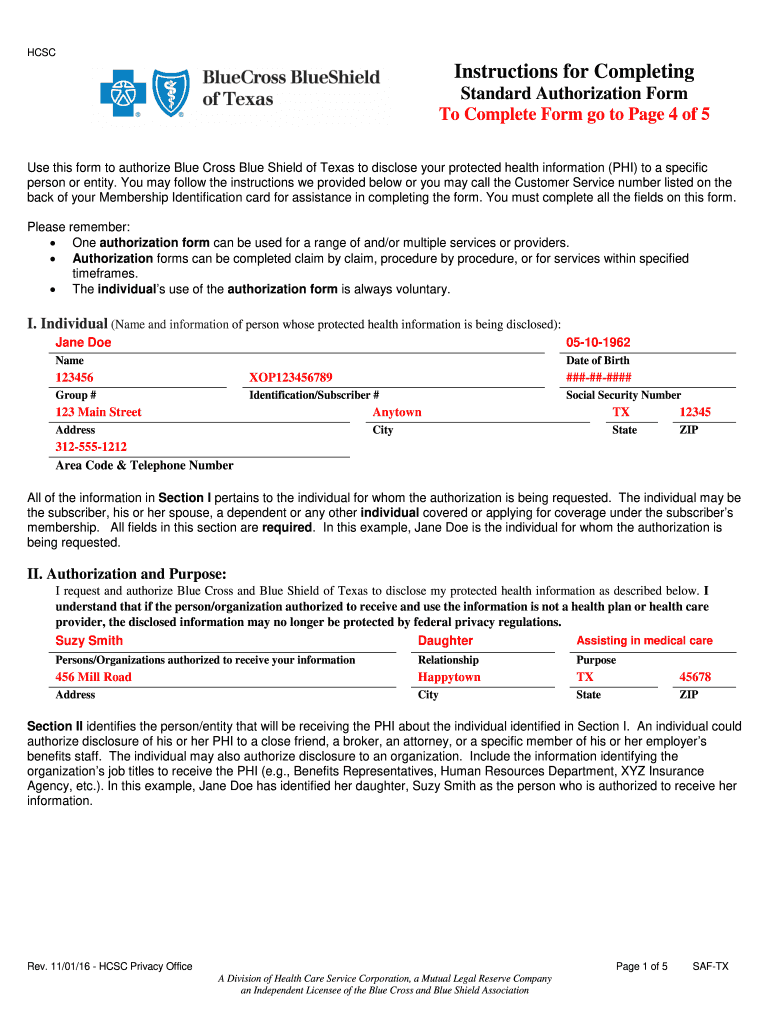
2012 Form TX Blue Cross Blue Shield SAFTX Fill Online, Printable
Related Post: