Benecard Pbf Prior Authorization Form
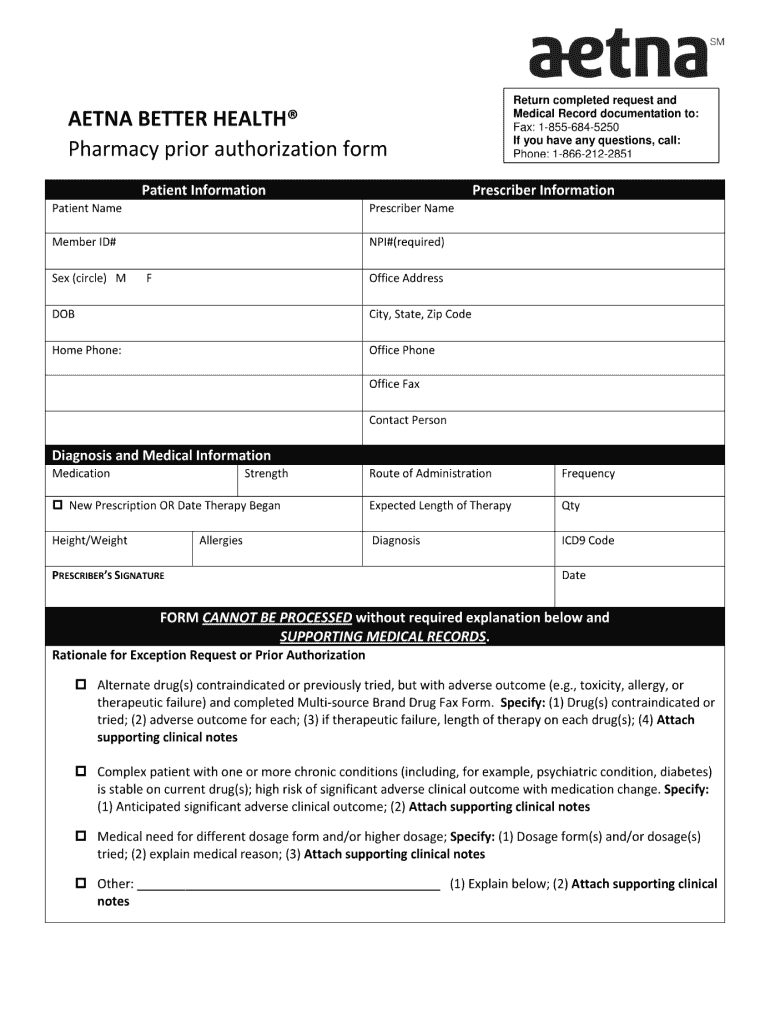
Benecard Pbf Prior Authorization Form - Web benecard pbf believes in keeping patients and plan sponsors always first. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Web benecard services, llc is a full service, in house prescription benefit administrator that includes mail and specialty drug dispensing. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Clinical review for prior authorization; Web benecard is the pharmacy benefit manager (pbm) our clients choose to utilize when it comes to their rx benefits. You can also find more helpful content under the resources & insights section of this site. Web as the individual identified to be personal representative on this form. A prior authorization reject means that the medication. Save or instantly send your ready documents. Working together, benecard pbf, pharmacies, and healthcare providers help. Web benecard is the pharmacy benefit manager (pbm) our clients choose to utilize when it comes to their rx benefits. Web benecard pbf believes in keeping patients and plan sponsors always first. Web as the individual identified to be personal representative on this form. Clinical review for prior authorization; You can also find more helpful content under the resources & insights section of this site. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Web complete benecard prior authorization form online with us legal forms. Updates typically take effect in january and july. Web we believe in providing a better experience for the patient. Web benecard services' members call: Clinical review for prior authorization; You can access your plan’s formulary by logging. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Web forms are available for download below. Web benecard services, llc is a full service, in house prescription benefit administrator that includes mail and specialty drug dispensing. We specialize in delivering tailored benefit. You can also find more helpful content under the resources & insights section of this site. 400 benecard pbf 5040 ritter road mechanicsburg, pa 17055. Save or instantly send your ready documents. A prior authorization reject means that the medication. Easily fill out pdf blank, edit, and sign them. We specialize in delivering tailored benefit. Web benecard services' members call: Benecard's team truly understands the pharmacy benefit. Clinical review for prior authorization; Not seeing what you need? Clinical review for prior authorization; You can access your plan’s formulary by logging. 400 benecard pbf 5040 ritter road mechanicsburg, pa 17055. Web forms are available for download below. Clinical review for prior authorization; Working together, benecard pbf, pharmacies, and healthcare providers help. You can also find more helpful content under the resources & insights section of this site. Web benecard is the pharmacy benefit manager (pbm) our clients choose to utilize when it comes to their rx benefits. Clinical review for prior authorization; Clinical review for prior authorization; Web forms are available for download below. You can access your plan’s formulary by logging. Benecard's team truly understands the pharmacy benefit. Updates typically take effect in january and july. A prior authorization reject means that the medication. Web benecard pbf pharmacy provider manual. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. You can access your plan’s formulary by logging. A prior authorization reject means that the medication. Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Use get form or simply click on the template preview to open it in the editor. Web our pharmacist’s proactive guidance also ended up saving the member approximately $8,000 (awp). Updates typically take effect in january and july. Web 2.2 the limitations on benecard's liability to you in paragraph 2.1 above shall apply whether or not benecard has been advised of or should have been aware of the possibility of any. Save or instantly send your ready documents. Not seeing what you need? Web benecard services, llc is a full service, in house prescription benefit administrator that includes mail and specialty drug dispensing. Updates typically take effect in january and july. Web forms are available for download below. Web as the individual identified to be personal representative on this form. Clinical review for prior authorization; Clinical review for prior authorization; Web benecard pbf releases updated formularies (a list of covered drugs) twice a year. Web our pharmacist’s proactive guidance also ended up saving the member approximately $8,000 (awp). You can access your plan’s formulary by logging. Web benecard is the pharmacy benefit manager (pbm) our clients choose to utilize when it comes to their rx benefits. 400 benecard pbf 5040 ritter road mechanicsburg, pa 17055. Working together, benecard pbf, pharmacies, and healthcare providers help. Clinical review for prior authorization; We specialize in delivering tailored benefit. Web we believe in providing a better experience for the patient and everyone involved in patient care. Web complete benecard prior authorization form online with us legal forms. Web benecard services' members call:Aetna blank prior authorization forms Fill out & sign online DocHub
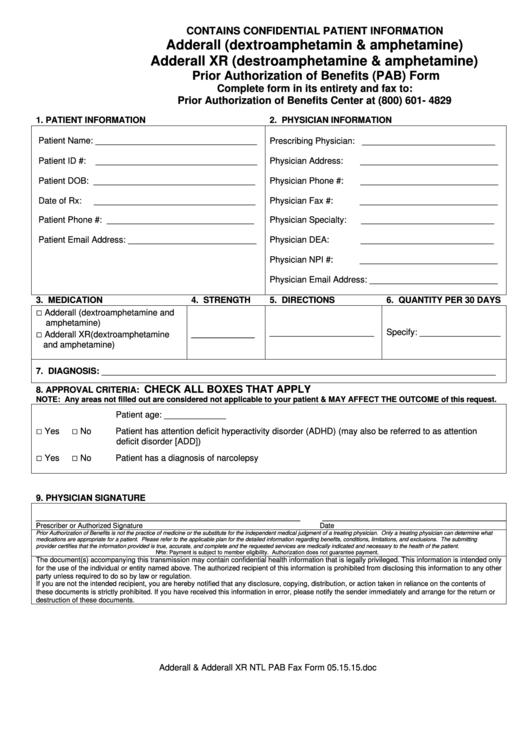
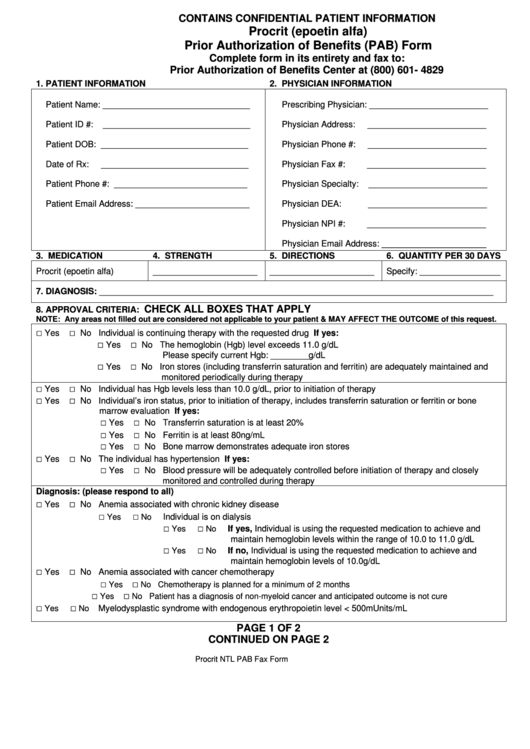
Prior Authorization Of Benefits (Pab) Form printable pdf download
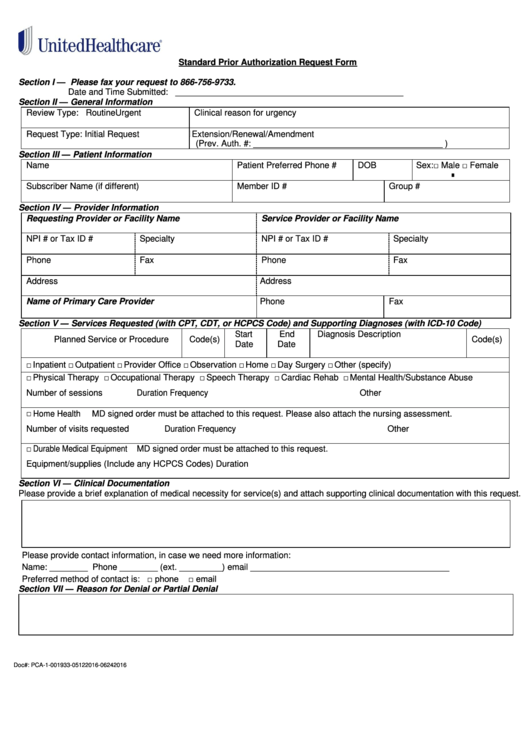
Fillable Standard Prior Authorization Request Form United Healthcare
How To Write A Prior Authorization Letter
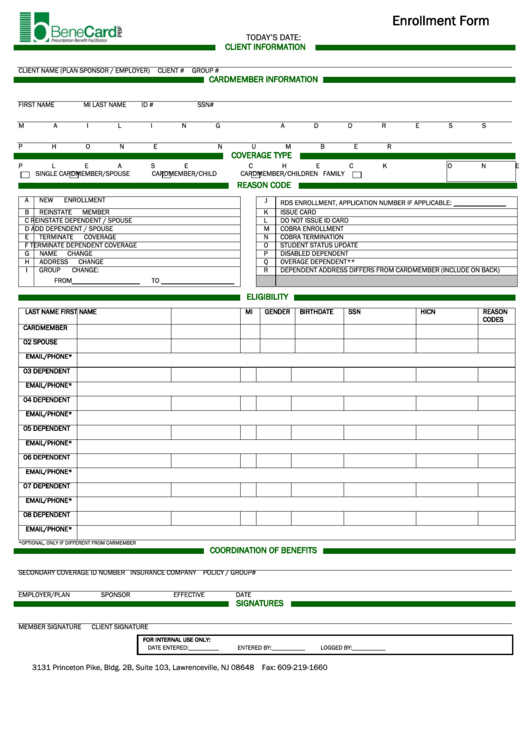
Benecard Enrollment Form printable pdf download
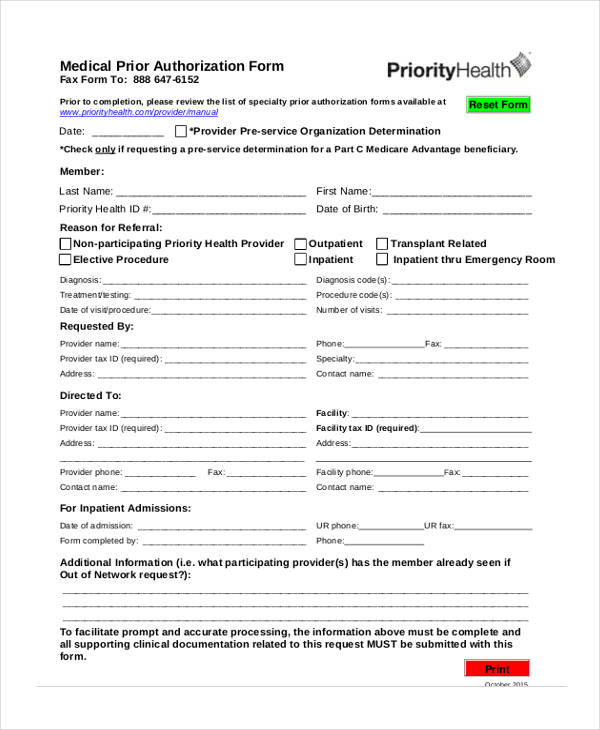
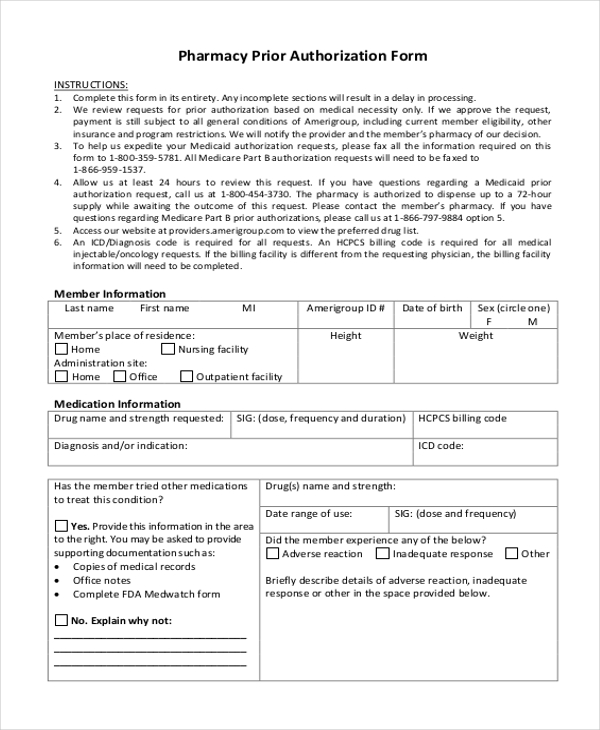
FREE 11+ Prior Authorization Forms in PDF MS Word
Surescripts Prior Auth Printable Form Printable Form, Templates and
Medco Prior Auth Form Medication Form Resume Examples q25Z4Lxk0o
FREE 8+ Sample Prior Authorization Forms in PDF MS Word
Procrit (Epoetin Alfa) Prior Authorization Of Benefits (Pab) Form
Related Post: