Bcbs Oklahoma Prior Authorization Form
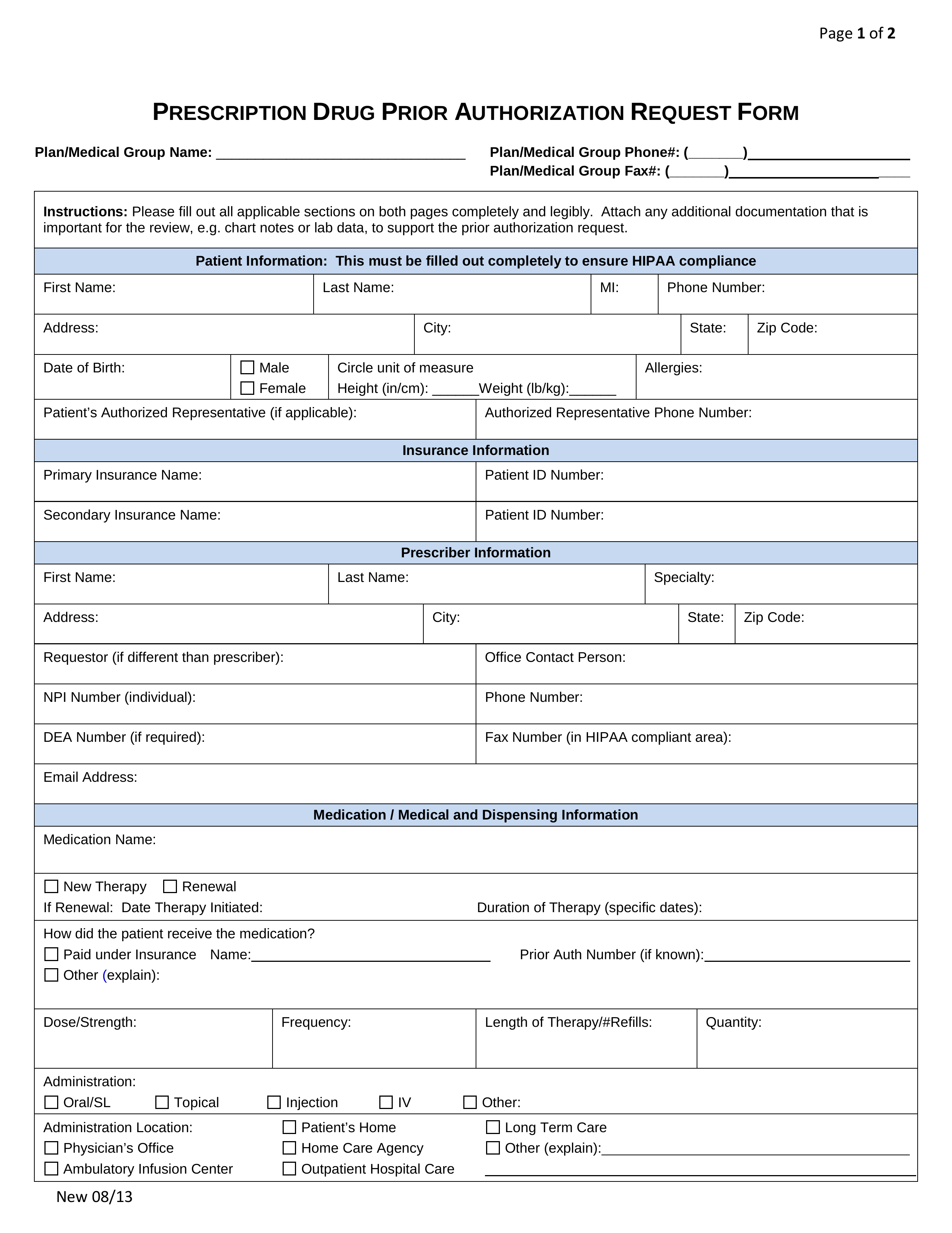
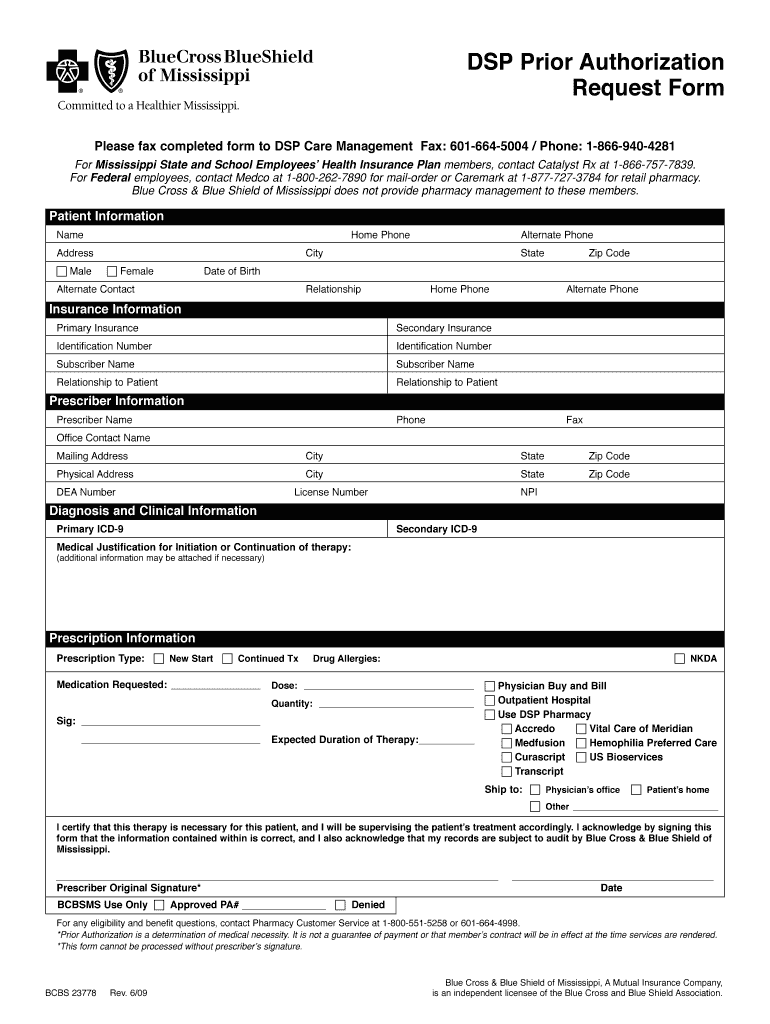
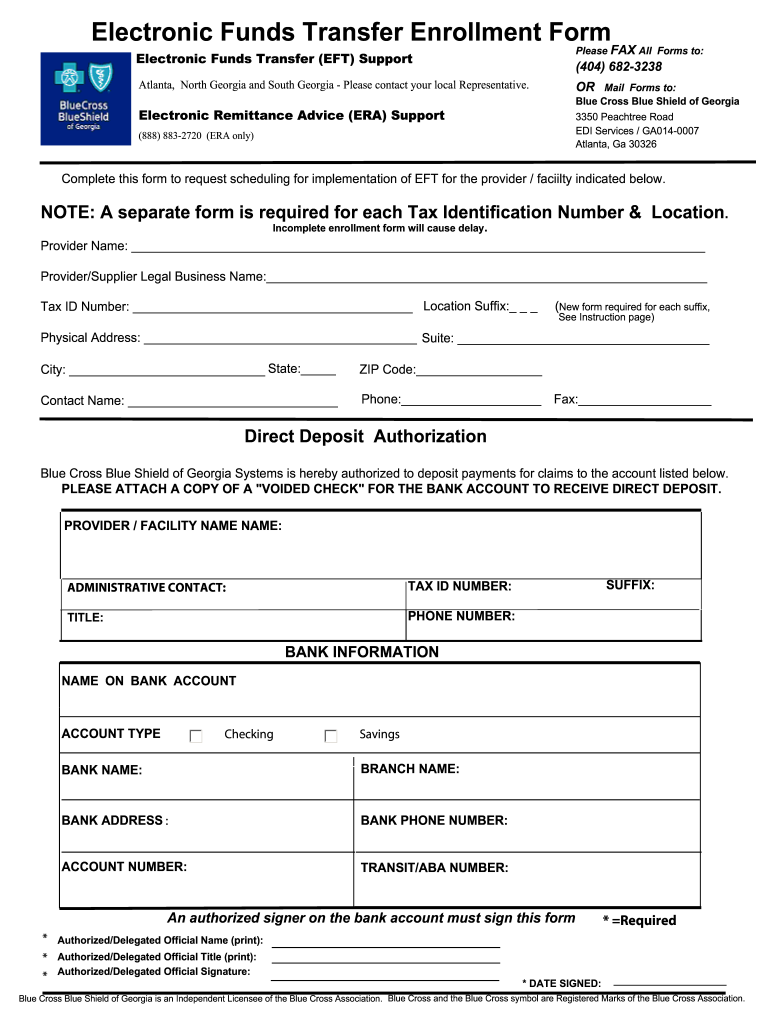
Bcbs Oklahoma Prior Authorization Form - Ad pdffiller.com has been visited by 1m+ users in the past month Confirm if prior authorization is required using availity ® or your preferred vendor. Required on some medications before your drug will be covered. The information contained in this presentation is intended to instruct soonercare providers on the prior authorization process for medical services, with member and. Web prior authorization/step therapy forms | blue cross and blue shield of oklahoma. 2023 commercial outpatient benefit preauthorization behavorial health procedure. If your health plan's formulary guide indicates that you need a prior authorization for a. There are three reasons for the use of prior authorization: Web here are some commonly used forms for conducting business with blue cross and blue shield of oklahoma (bcbsok). Web form name and description revision date; 2023 commercial outpatient benefit preauthorization behavorial health procedure. It’s easier than you think. An eligibility and benefits inquiry should be completed first to confirm membership, verify coverage and determine whether or not prior. Or, download pa and st program criteria summaries and fax forms from the prime therapeutics website using the following links:. Prior authorization (pa) and step. Prior authorization and step therapy programs. Mental health/substance use disorder precertification. Blue cross blue shield of oklahoma is committed to giving health care providers with the support and assistance they need. The information contained in this presentation is intended to instruct soonercare providers on the prior authorization process for medical services, with member and. Web submit an electronic prior authorization. Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained through us or a dedicated. Or, download pa and st program criteria summaries and fax forms from the prime therapeutics website using the following links:. An eligibility and benefits inquiry should be completed first to confirm membership, verify. Or, download pa and st program criteria summaries and fax forms from the prime therapeutics website using the following links:. Web authorizations & referrals is an online tool in the availity provider portal that allows you to submit preauthorization and/or referral requests handled by blue cross and blue shield. Web here are some commonly used forms for conducting business with. Required on some medications before your drug will be covered. This will determine if prior authorization will be obtained through us or a dedicated. Web prior authorization (pa) 2021. Prior authorization (pa) and step. An eligibility and benefits inquiry should be completed first to confirm membership, verify coverage and determine whether or not prior. Web pharmacy prior authorization amendment form: This will determine if prior authorization will be obtained through us or a dedicated. Prior authorization (pa) and step. Rewards and incentives for healthy activities. Web requests for prior authorization must in all cases be accompanied by appropriate clinical/medical record information except for routine vaginal or cesarean section. Prior authorization (pa) and step. This will determine if prior authorization will be obtained through us or a dedicated. Web requests for prior authorization must in all cases be accompanied by appropriate clinical/medical record information except for routine vaginal or cesarean section. Web prior authorization (pa) 2021. If your health plan's formulary guide indicates that you need a prior authorization. The information contained in this presentation is intended to instruct soonercare providers on the prior authorization process for medical services, with member and. Required on some medications before your drug will be covered. Web authorizations & referrals is an online tool in the availity provider portal that allows you to submit preauthorization and/or referral requests handled by blue cross and. If your health plan's formulary guide indicates that you need a prior authorization for a. Web prior authorization (pa) 2021. Web pharmacy prior authorization amendment form: Most hmo and ppo contracts require the member or provider to contact bcbsok to receive precertification (also known as. Rewards and incentives for healthy activities. Web new payer id effective jan. Standard authorization form and other hipaa privacy forms authorizes blue cross and blue shield of oklahoma. Scope controls, utilization controls and product based controls. Petition for tuberculosis related therapy authorization: Web complete all necessary precertification processes. Mental health/substance use disorder precertification. Most hmo and ppo contracts require the member or provider to contact bcbsok to receive precertification (also known as. The information contained in this presentation is intended to instruct soonercare providers on the prior authorization process for medical services, with member and. Web authorizations & referrals is an online tool in the availity provider portal that allows you to submit preauthorization and/or referral requests handled by blue cross and blue shield. Confirm if prior authorization is required using availity ® or your preferred vendor. Rewards and incentives for healthy activities. To access more downloadable forms,. Prior authorization and step therapy programs. Web requests for prior authorization must in all cases be accompanied by appropriate clinical/medical record information except for routine vaginal or cesarean section. Why is prior authorization important? Required on some medications before your drug will be covered. If your health plan's formulary guide indicates that you need a prior authorization for a. Web prior authorization/step therapy forms | blue cross and blue shield of oklahoma. An eligibility and benefits inquiry should be completed first to confirm membership, verify coverage and determine whether or not prior. Standard authorization form and other hipaa privacy forms authorizes blue cross and blue shield of oklahoma. Or, download pa and st program criteria summaries and fax forms from the prime therapeutics website using the following links:. Web worried that getting prior authorization might be a hassle? Web new payer id effective jan. Prior authorization (pa) and step. These pharmacy programs are available for members.Regence Bcbs Prior Authorization Form Fill Online, Printable
20152022 Blue Advantage BCBS Medicare Part D Prescription Drug
Empire Blue Cross Blue Shield Authorization To Release Information
Beautiful Bcbs Centennial Care Prior Authorization form
Free Medicaid (Rx) Prior Authorization Forms PDF eForms
Ms bcbs claim Fill out & sign online DocHub
Bcbs Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Bcbs Prior Authorization Form Form Resume Examples NRE34PV36x
Bcbs Prior Auth Forms To Print Fill Online, Printable, Fillable
Bcbs Prior Authorization Form PDF Fill Out and Sign Printable PDF
Related Post: