Bcbs Federal Predetermination Form
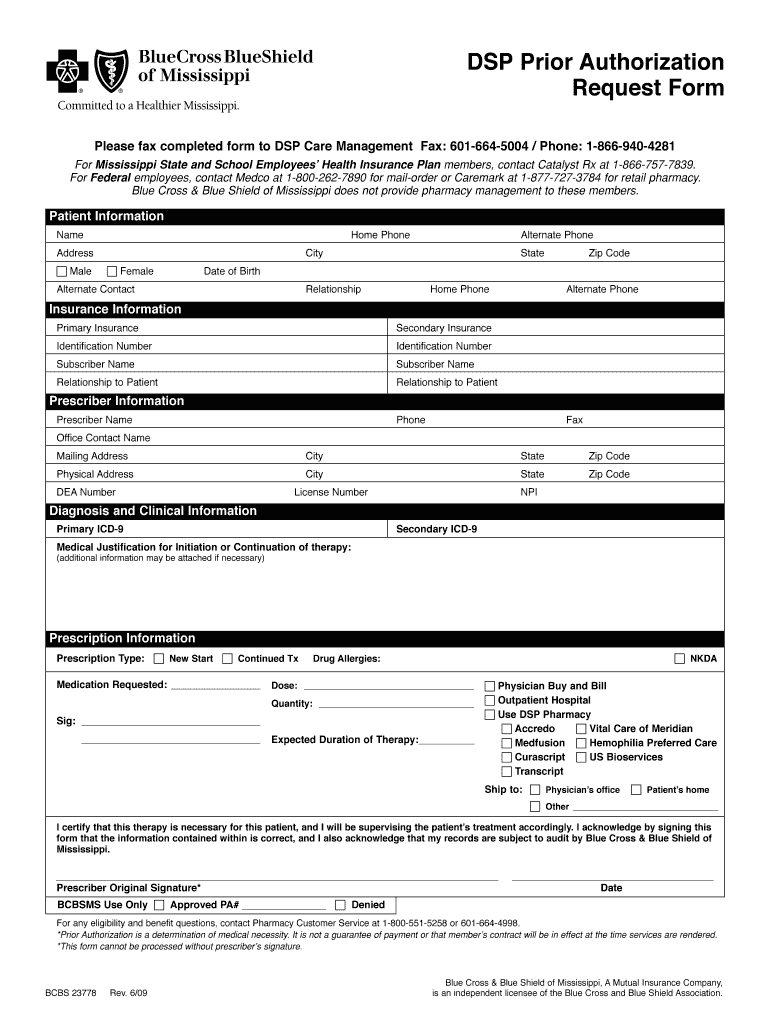
Bcbs Federal Predetermination Form - Web a recommended clinical review (formerly called predetermination) is a medical necessity review conducted before services are provided. If unable to fax, you may mail your. Select claims & payments from the navigation menu. Web 1 results found for search term : Web x21975r04 (9/20) blue cross ® and blue shield® of minnesota and blue plus ® are nonprofit independent licensees of the blue cross and blue shield association. Fax form and relevant clinical. Web aca bowel prep prevention coverage member request form. View and download our medical, pharmacy and overseas claim forms. Within the tool, select send attachment then predetermination attachment. Web a predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health benefit plan. Web a predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health benefit plan. Complete the member request form for aca bowel prep prevention coverage. Use this form to request a medical necessity review for a service or item that is not on our prior authorization list.. Edit, sign and save teamcare benefits request form. Web federal employee gender affirming surgery prior approval request form; Web how to file internal and external appeals. Complete the member request form for aca bowel prep prevention coverage. Ad register and subscribe now to work on teamcare medical predetermination of benefits req. Web aca bowel prep prevention coverage member request form. Web a predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health benefit plan. If the patient is retired from the federal government, butstill employed,please complete 4b yes no. How to request an advance benefit determination for your. Web federal employee gender affirming surgery prior approval request form; Use this form to request a medical necessity review for a service or item that is not on our prior authorization list. Web only use this form for requests for predetermination. Web 1 results found for search term : Federal employee predetermination / prior approval form; 1) submit a claim for payment or request payment on a claim; Web a recommended clinical review (formerly called predetermination) is a medical necessity review conducted before services are provided. Select claims & payments from the navigation menu. Do not use this form to: Complete the member request form for aca bowel prep prevention coverage. Submitting the request prior to rendering. Web federal employee gender affirming surgery prior approval request form; Web aca bowel prep prevention coverage member request form. 1) submit a claim for payment or request payment on a claim; You will be going to a. You will be going to a. Fax form and relevant clinical. Web a predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health benefit plan. View and download our medical, pharmacy and overseas claim forms. Web this page provides prior approval requirements, contact information, and forms for. Do not use this form to: Web a recommended clinical review (formerly called predetermination) is a medical necessity review conducted before services are provided. Complete the member request form for aca bowel prep prevention coverage. Submitting the request prior to rendering. If unable to fax, you may mail your. Do not use this form to: If the patient is retired from the federal government, butstill employed,please complete 4b yes no. View and download our medical, pharmacy and overseas claim forms. Ad register and subscribe now to work on teamcare medical predetermination of benefits req. Web a recommended clinical review (formerly called predetermination) is a medical necessity review conducted before. 1) submit a claim for payment or request payment on a claim; Web a predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health benefit plan. Web how to file internal and external appeals. Web log in to availity. Please complete this form and attach as your. Use this form to request a medical necessity review for a service or item that is not on our prior authorization list. You will be going to a. Edit, sign and save teamcare benefits request form. Please complete this form and attach as your cover sheet along with supporting documentation and clinical rationale for a predetermination review. Web aca bowel prep prevention coverage member request form. Web you must submit the predetermination to the blue cross and blue shield plan that issues or administers the patient’s health benefit plan which may not be the state where you are. Web a recommended clinical review (formerly called predetermination) is a medical necessity review conducted before services are provided. If unable to fax, you may mail your. Select claims & payments from the navigation menu. Federal employee predetermination / prior approval form; Within the tool, select send attachment then predetermination attachment. How to request an advance benefit determination for your local federal employee program patients. Complete the member request form for aca bowel prep prevention coverage. View and download our medical, pharmacy and overseas claim forms. Web 1 results found for search term : Web federal employee gender affirming surgery prior approval request form; Fax form and relevant clinical. Web only use this form for requests for predetermination. As a preferred provider, you can. 1) submit a claim for payment or request payment on a claim;Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
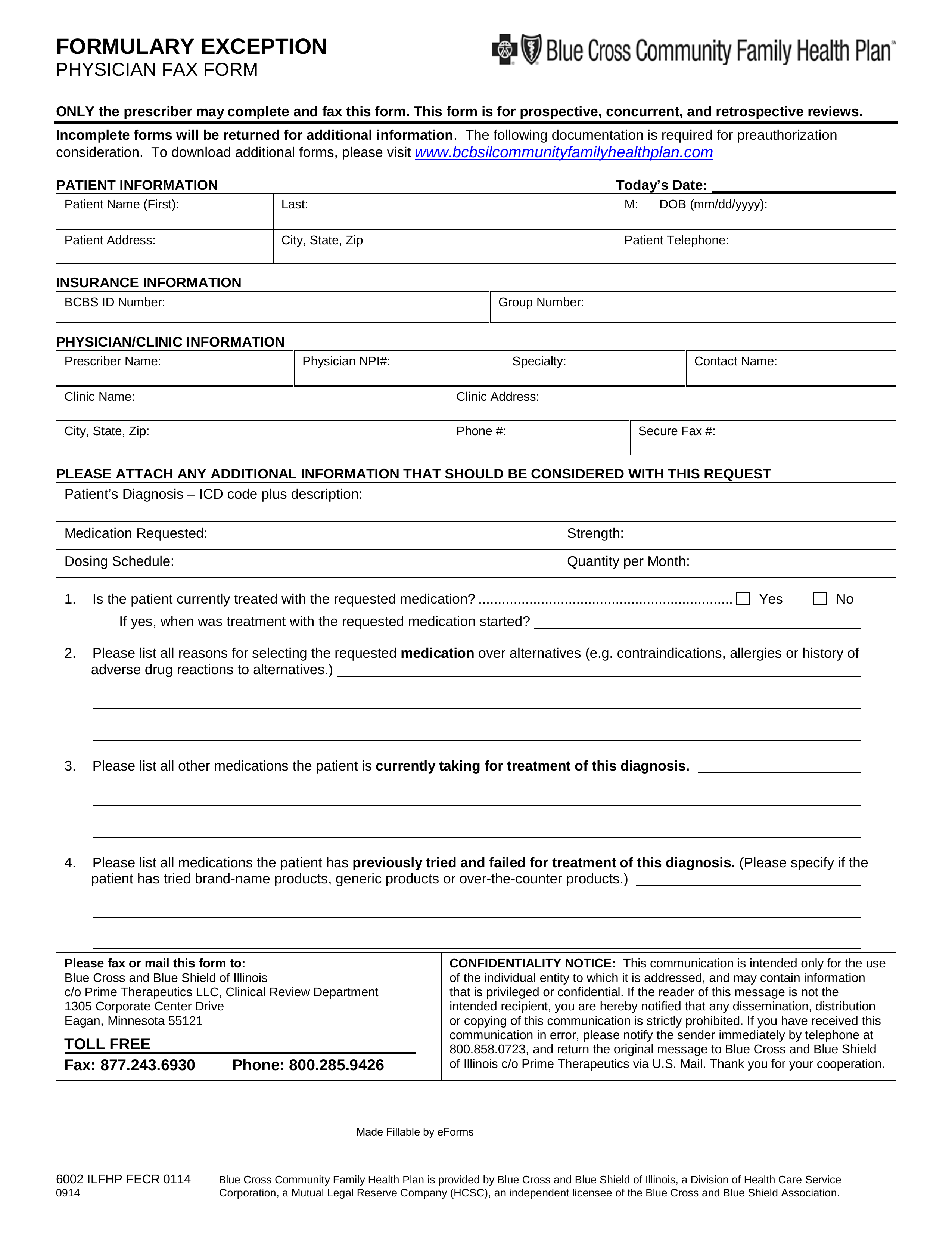
Prime Therapeutics Pharmacy Prior Authorization Form PharmacyWalls
20152023 Blue Advantage BCBS Medicare Part D Prescription Drug
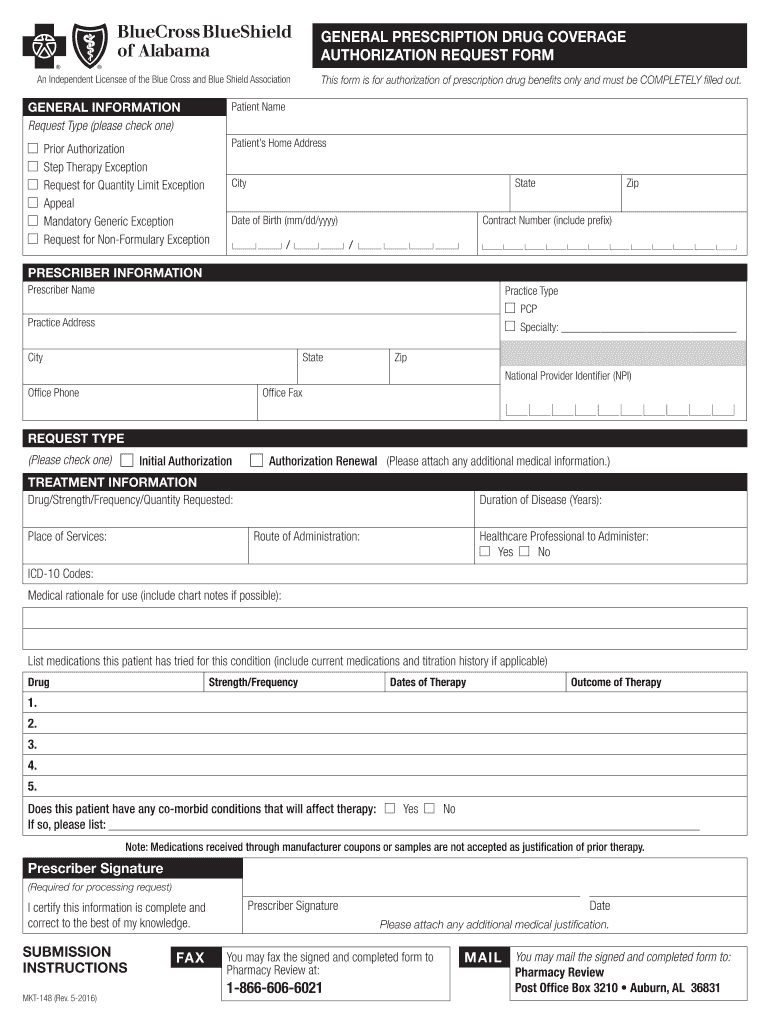
Bcbs Alabama Prior Authorization Fill Out and Sign Printable PDF
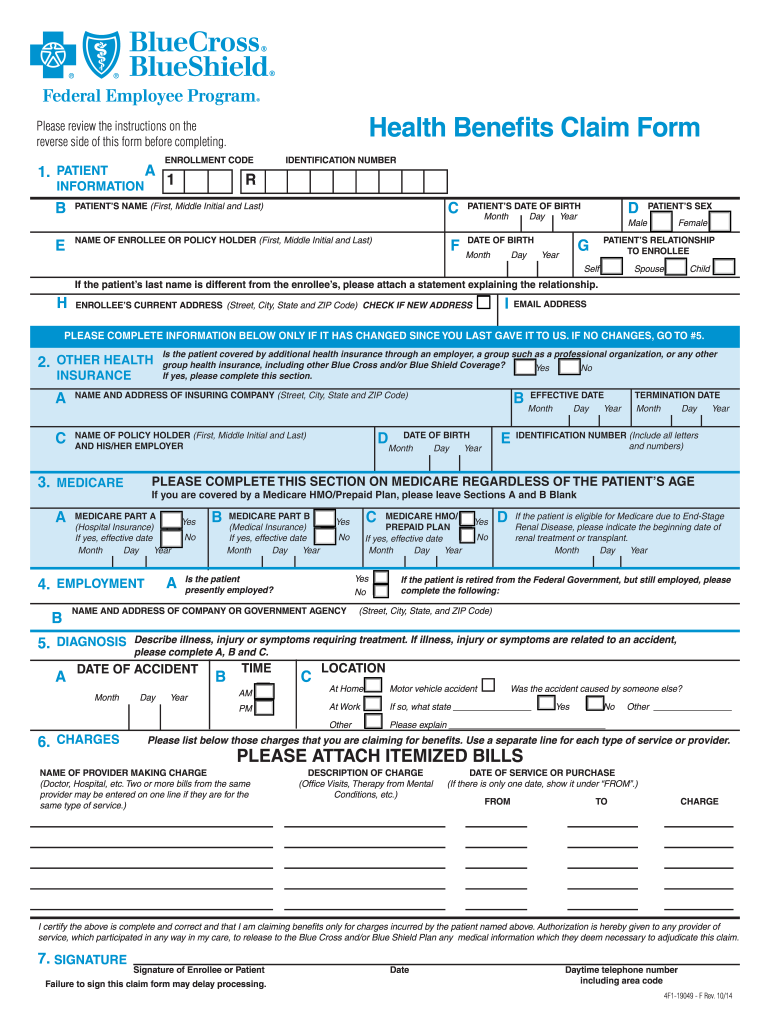
Bcbs federal claim form Fill out & sign online DocHub
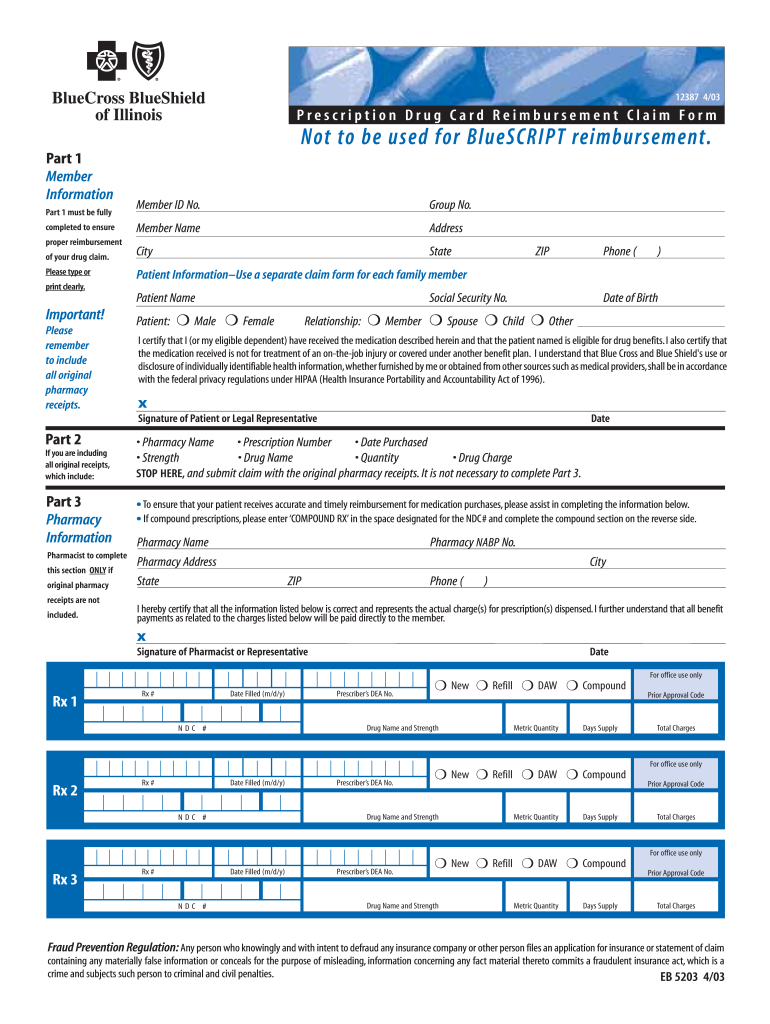
Blue Cross Blue Shield Of Illinois Claim Form Fill Out and Sign
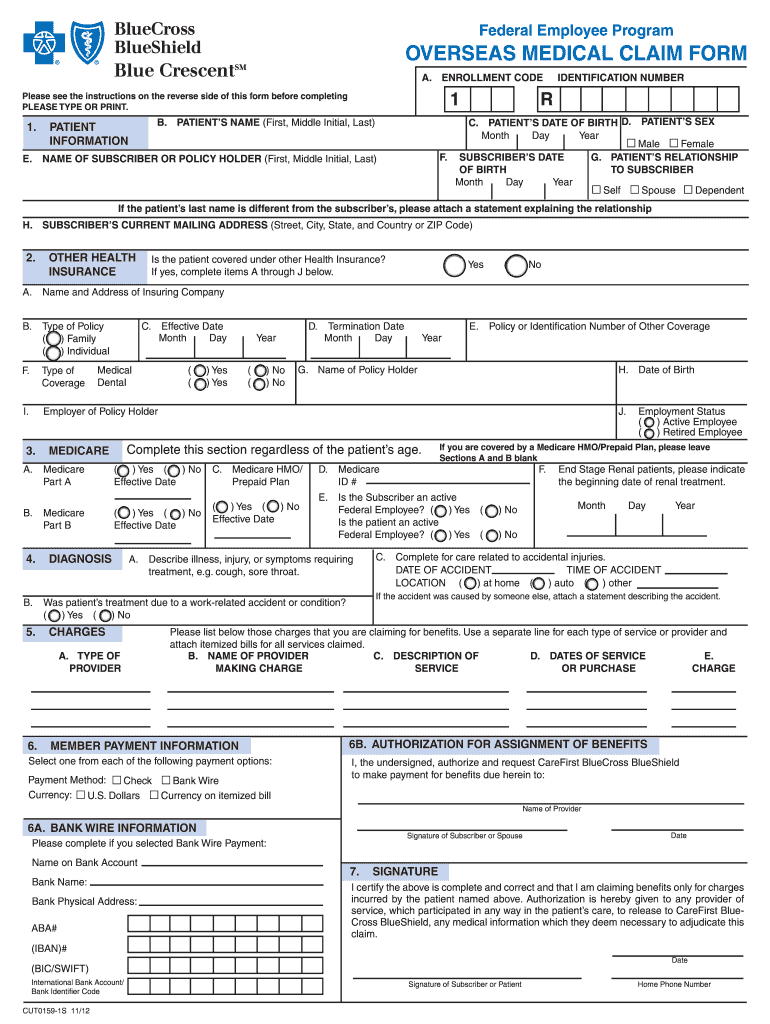
Federal BCBS Basic Overseas Claim Form Fill Out and Sign Printable
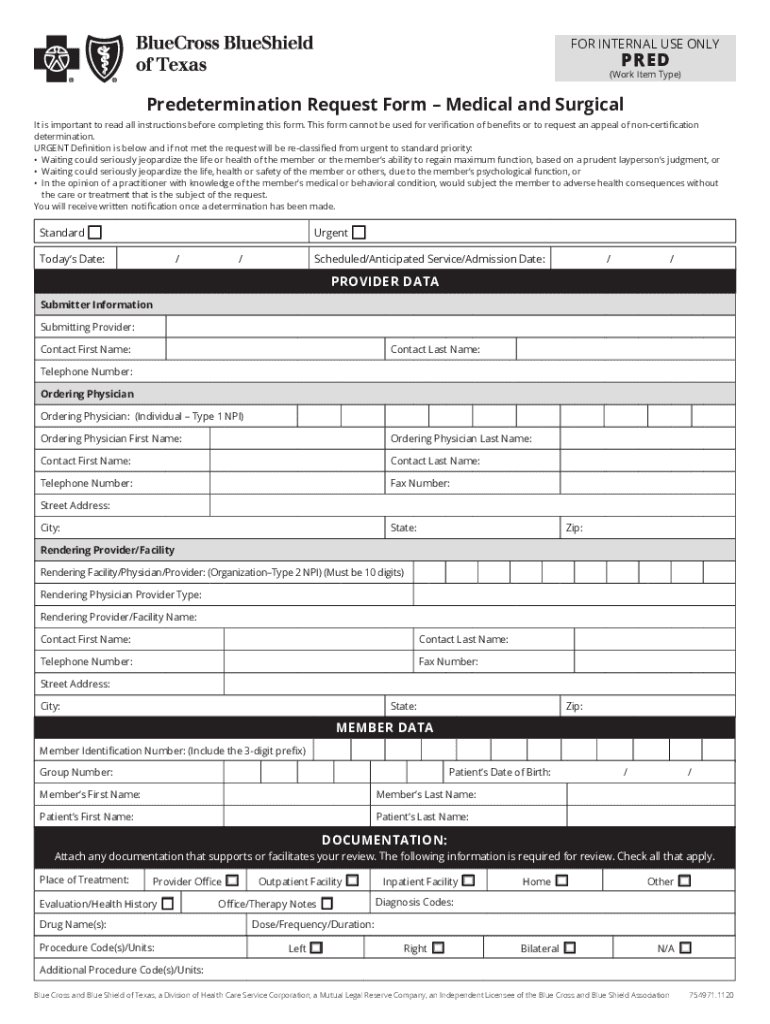
Bcbs Predetermination Form Fill Out and Sign Printable PDF Template
Empire Blue Cross Blue Shield Authorization To Release Information
AR BCBS Group Employee Application 2019 Fill and Sign Printable
Related Post: