Aetna Reconsideration Form For Providers
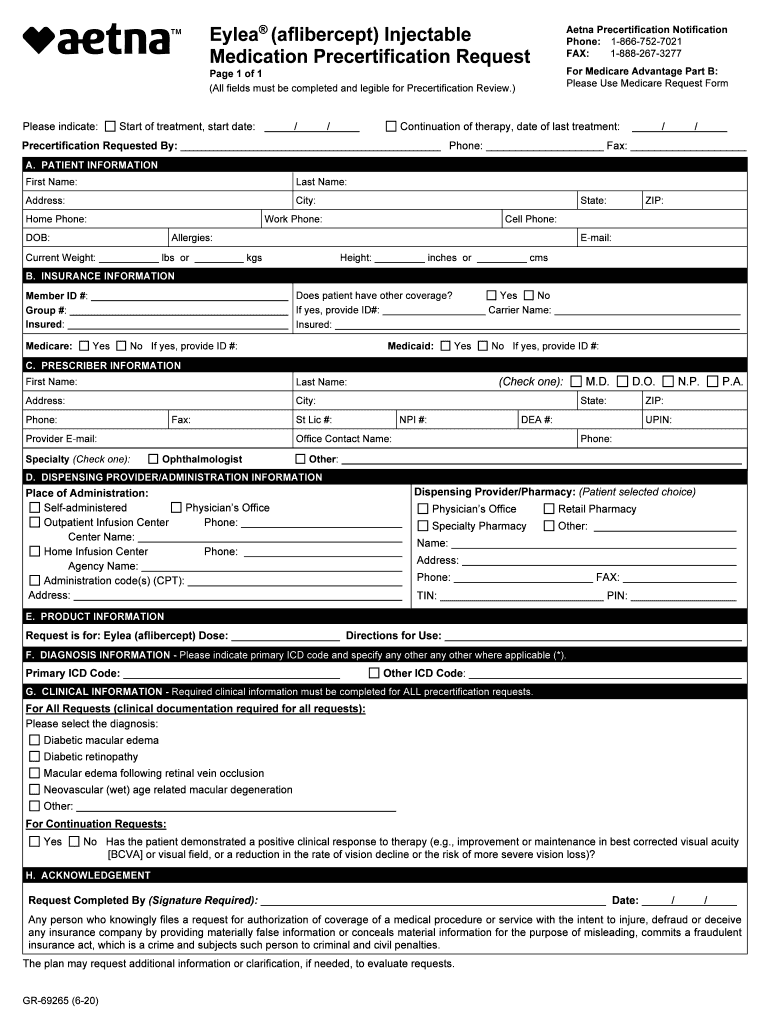
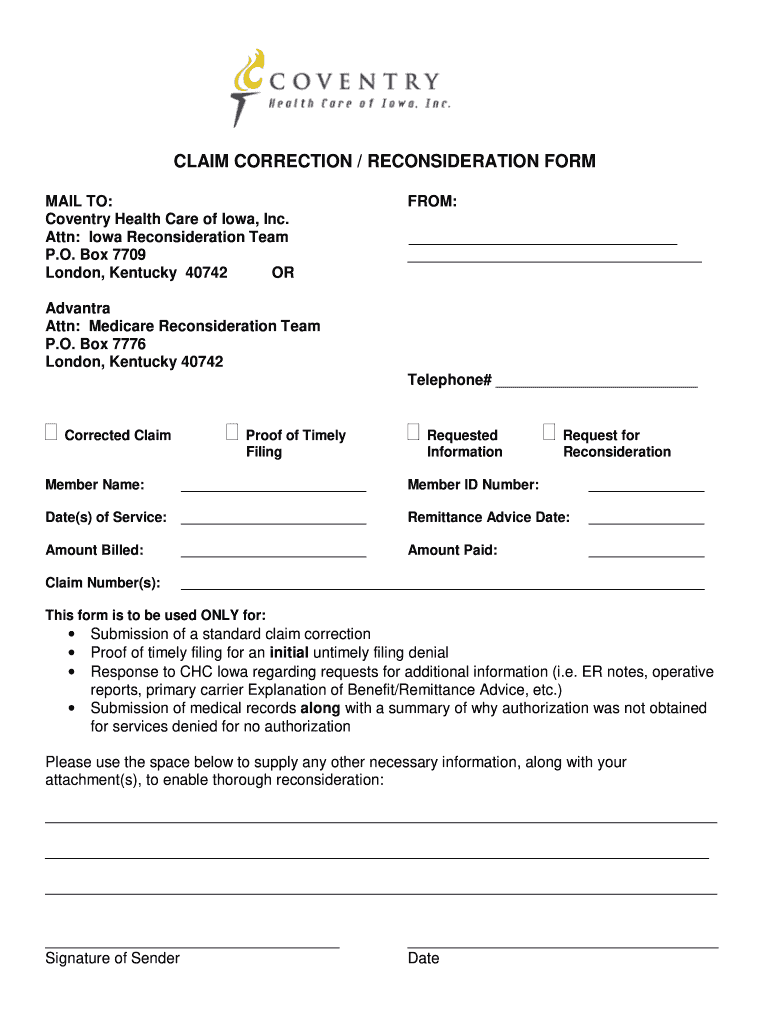
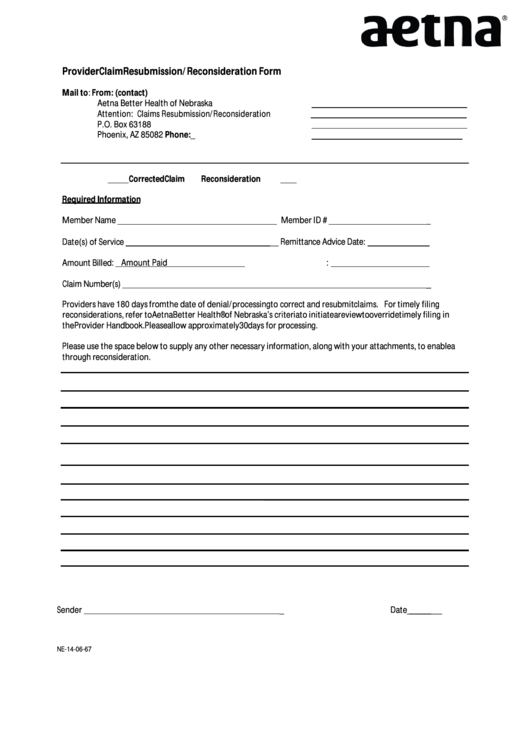
Aetna Reconsideration Form For Providers - Web a preferred provider that received an underpayment in relation to an audit must notify aetna within 270 days per texas law to qualify to receive a penalty for the underpaid. Upload, modify or create forms. Web may use this form to request an independent review of your drug plan’s decision. Web provider claim resubmission and dispute form (pdf) independent review provider reconsideration request form (pdf) personal appeal representative form (pdf) Try it for free now! Web if the request does not qualify for a reconsideration as defined below, the request must be submitted as an appeal online through our provider website on availity, or by mail/fax,. Ad signnow.com has been visited by 100k+ users in the past month To obtain a review submit this form as. Web claims reconsideration & appeals form complete this form and return to aetna better health of texas for processing your request. Easily fill out pdf blank, edit, and sign them. Web this form is for your representative's use in making suggestions or filing formal complaints or appeals regarding any aspect of the aetna health plan or any physician, hospital, or. The reconsideration decision (for claims disputes). Web may use this form to request an independent review of your drug plan’s decision. Web learn how to file a complaint or appeal. Web a preferred provider that received an underpayment in relation to an audit must notify aetna within 270 days per texas law to qualify to receive a penalty for the underpaid. Web if the request does not qualify for a reconsideration as defined below, the request must be submitted as an appeal online through our provider website on availity, or. Web this form is for your representative's use in making suggestions or filing formal complaints or appeals regarding any aspect of the aetna health plan or any physician, hospital, or. Web to help aetna review and respond to your request, please provide the following information. Web complete aetna reconsideration form online with us legal forms. The reconsideration decision (for claims. Web the availity appeals product supports aetna appeals and reconsideration processes for commercial and medicare claims adjudicated on the acas, hmo and. Web aetna better health® of florida. Discover how to submit a dispute. Upload, modify or create forms. Save or instantly send your ready documents. Save or instantly send your ready documents. Try it for free now! The reconsideration decision (for claims disputes). You can include supporting documents and information to help your case. To obtain a review submit this form as. You can include supporting documents and information to help your case. (this information may be found on correspondence from aetna.) you may use this form. Web if the request does not qualify for a reconsideration as defined below, the request must be submitted as an appeal online through our provider website on availity, or by mail/fax,. Web may use this. Web provider claim resubmission and dispute form (pdf) independent review provider reconsideration request form (pdf) personal appeal representative form (pdf) Web if the request does not qualify for a reconsideration as defined below, the request must be submitted in writing using the aetna provider complaint and appeal form. You have 60 days fromthedateof theplan’s redeterminationnoticetoask. Web aetna better health® of. Completion of this form is mandatory. Web to help aetna review and respond to your request, please provide the following information. Web provider claim resubmission and dispute form (pdf) independent review provider reconsideration request form (pdf) personal appeal representative form (pdf) Web a reconsideration is a formal review of a previous claim reimbursement or coding decision, or a claim that. Web this form is for your representative's use in making suggestions or filing formal complaints or appeals regarding any aspect of the aetna health plan or any physician, hospital, or. Try it for free now! Web you may request an appeal in writing using the aetna provider complaint and appeal form, if you are not satisfied with: Web claims reconsideration. You may disagree with a claim or utilization review decision. Save or instantly send your ready documents. Ad organization/facility app & more fillable forms, register and subscribe now! (this information may be found on correspondence from aetna.) you may use this form. You can include supporting documents and information to help your case. Web claims reconsideration & appeals form complete this form and return to aetna better health of texas for processing your request. To submit a request, call our precertification. Web if the request does not qualify for a reconsideration as defined below, the request must be submitted as an appeal online through our provider website on availity, or by mail/fax,. Web if the request does not qualify for a reconsideration as defined below, the request must be submitted in writing using the aetna provider complaint and appeal form. You may disagree with a claim or utilization review decision. Web this form is for your representative's use in making suggestions or filing formal complaints or appeals regarding any aspect of the aetna health plan or any physician, hospital, or. Upload, modify or create forms. You have 60 days fromthedateof theplan’s redeterminationnoticetoask. Web to help aetna review and respond to your request, please provide the following information. Web a preferred provider that received an underpayment in relation to an audit must notify aetna within 270 days per texas law to qualify to receive a penalty for the underpaid. Learn about the timeframe for appeals and. Web the availity appeals product supports aetna appeals and reconsideration processes for commercial and medicare claims adjudicated on the acas, hmo and. Reconsideration denial notification date(s) cpt/hcpc/service being disputed. Web learn how to file a complaint or appeal as a medicare contracted provider with aetna using this form. Discover how to submit a dispute. Web your claim reconsideration must include this completed form and any additional information (proof from primary payer, required documentation, cms or medicaid. Web a reconsideration is a formal review of a previous claim reimbursement or coding decision, or a claim that requires reprocessing where the denial is not based on medical necessity. Completion of this form is mandatory. To obtain a review submit this form as. Try it for free now!Aetna precertification form pdf Fill out & sign online DocHub
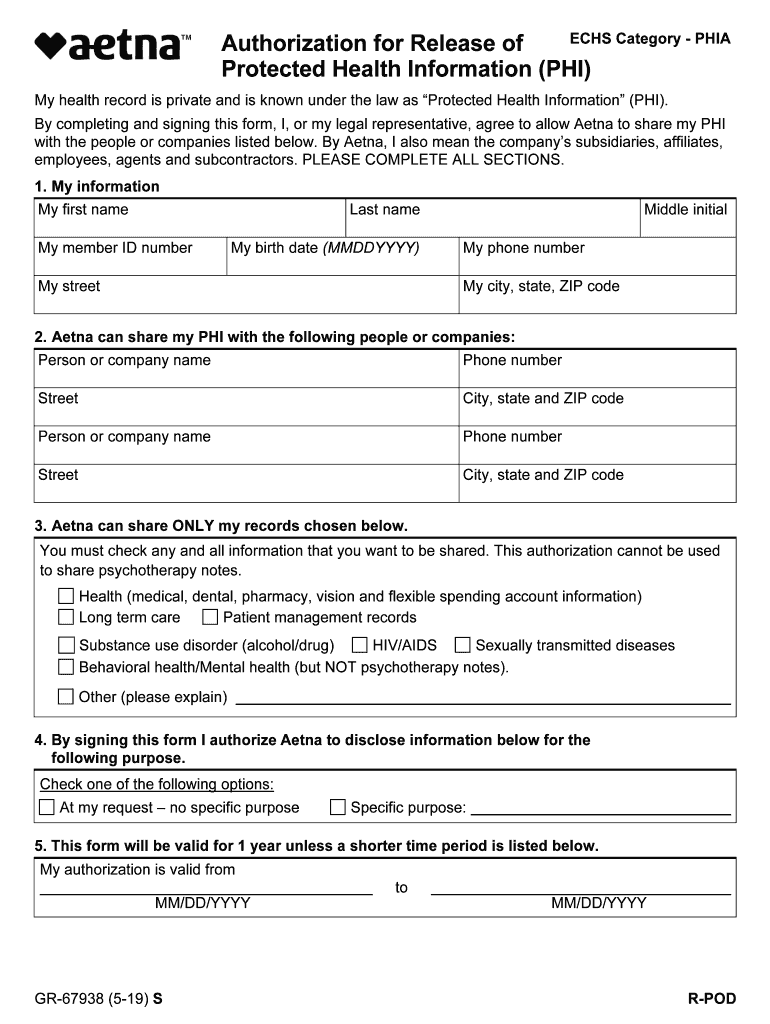
Aetna GR67938 S 20192021 Fill and Sign Printable Template Online
NJ Aetna DOBICAPPCAR 20102022 Fill and Sign Printable Template
Aetna Reconsideration Form 2022 Pdf Fill Out and Sign Printable PDF
Form Ne140667 Aetna Provider Claim Resubmission/reconsideration
Top 84 Aetna Forms And Templates free to download in PDF format
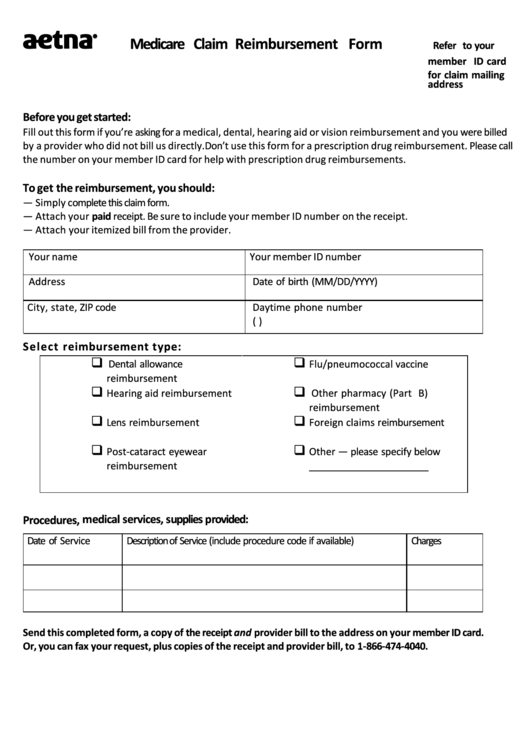
Download Aetna Medical Claim Form 2 for Free TidyTemplates
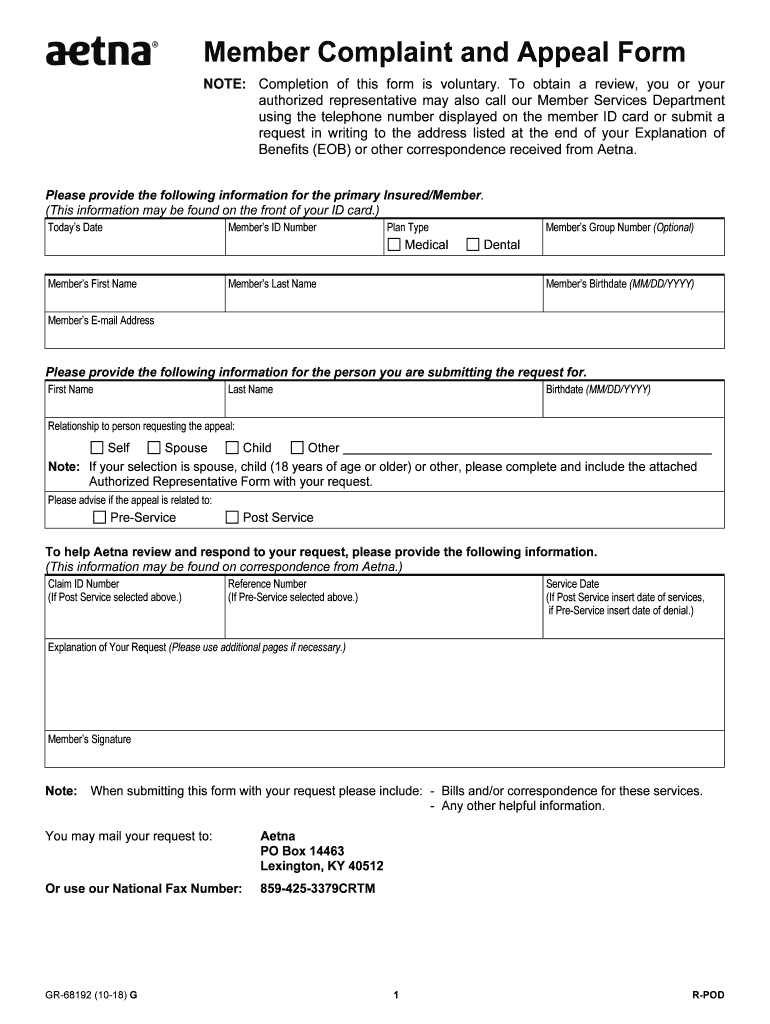
Member aetna com membersecure assets pdfs forms 68192 pdf Fill out
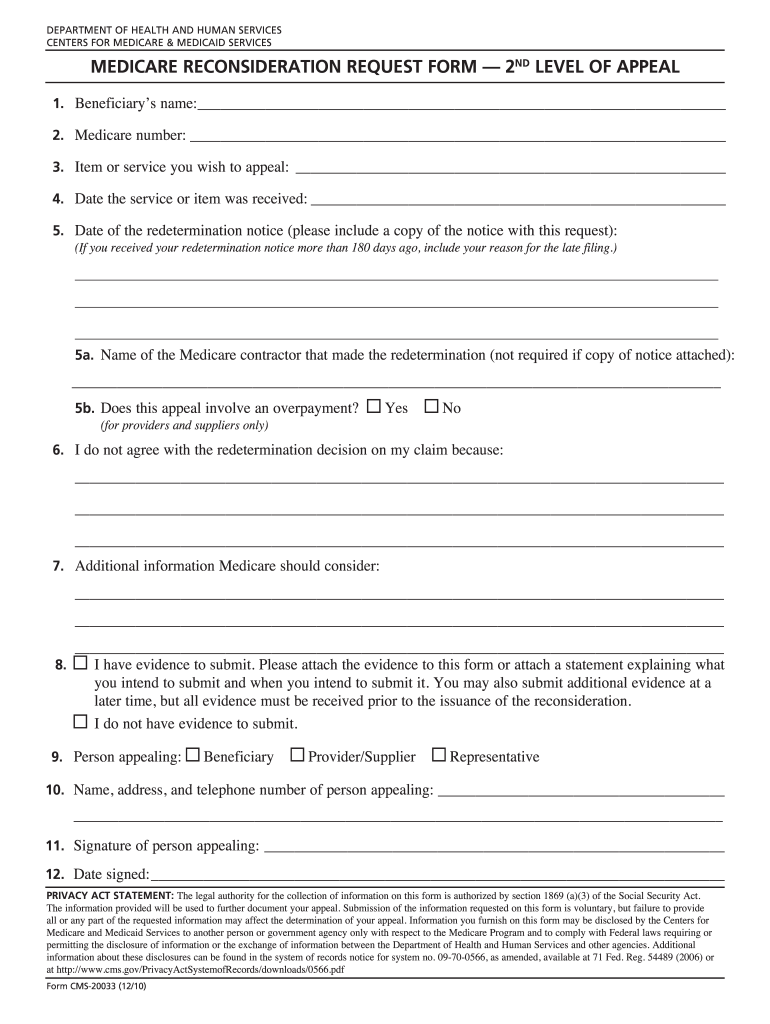
Forms for a Reconsideration Fill Out and Sign Printable PDF Template
Healthcare Partners Reconsideration Form Fill Online, Printable
Related Post: