Aetna Eylea Prior Authorization Form
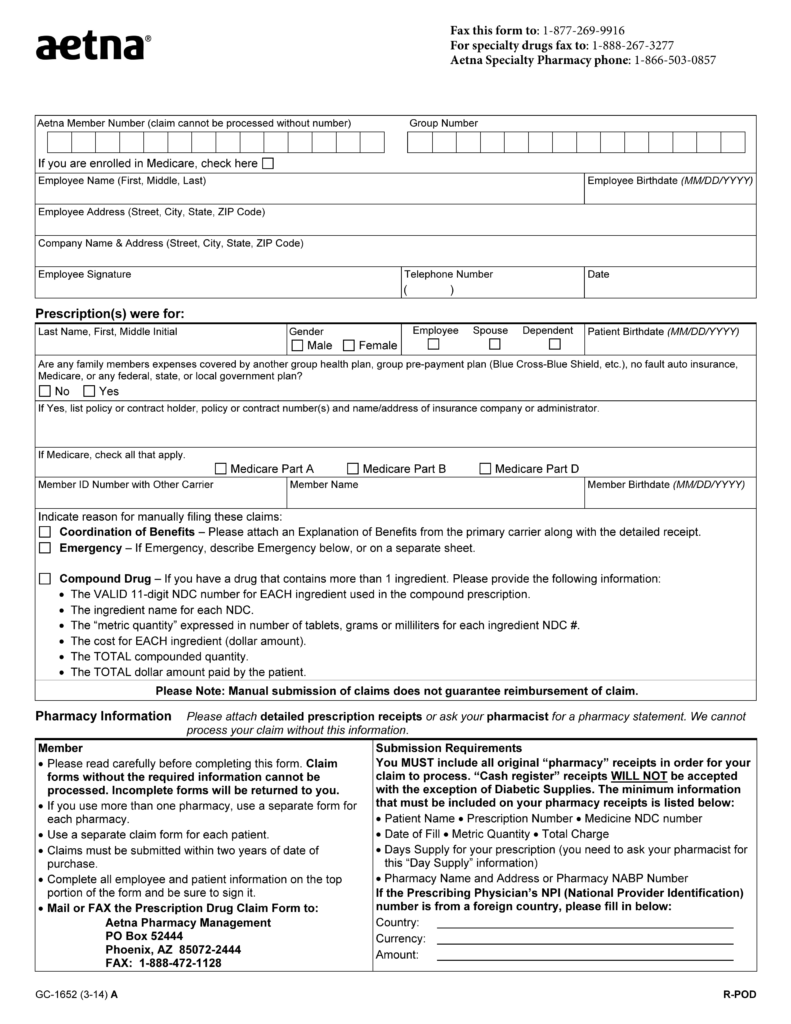
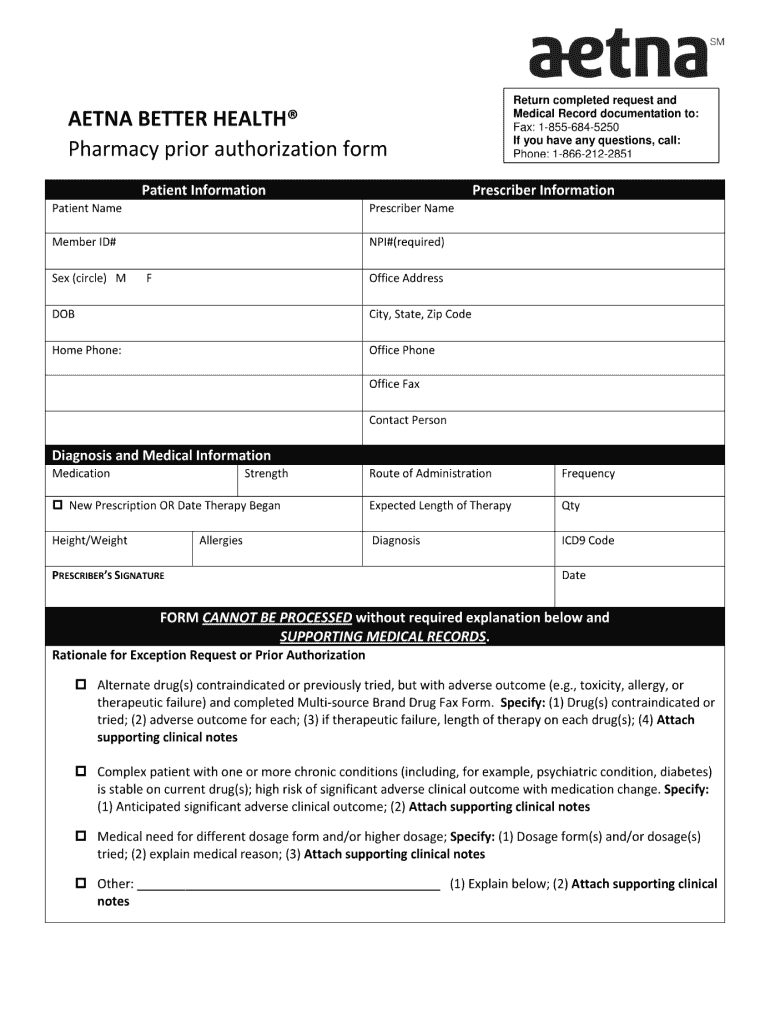
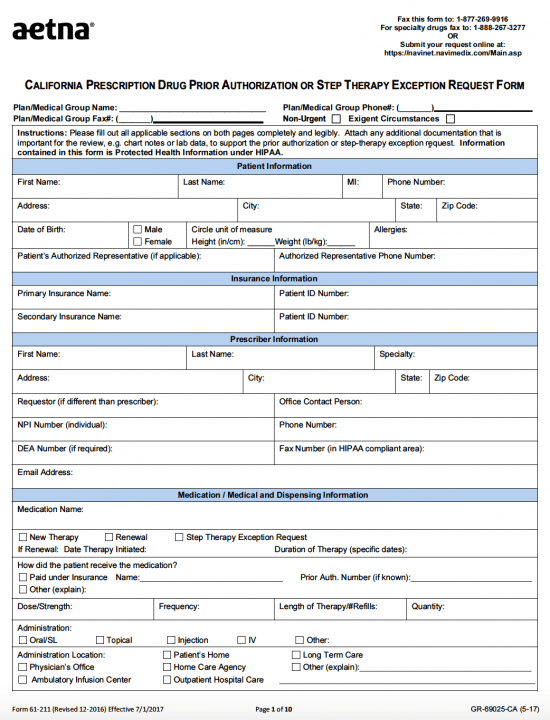
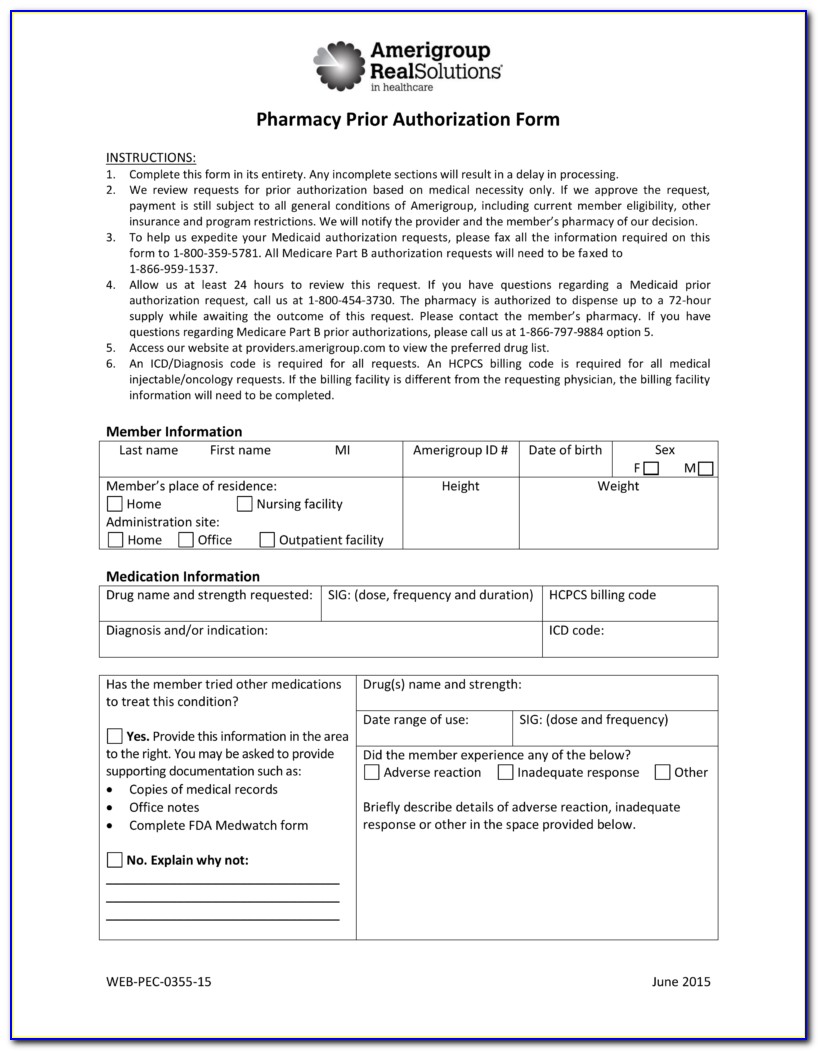
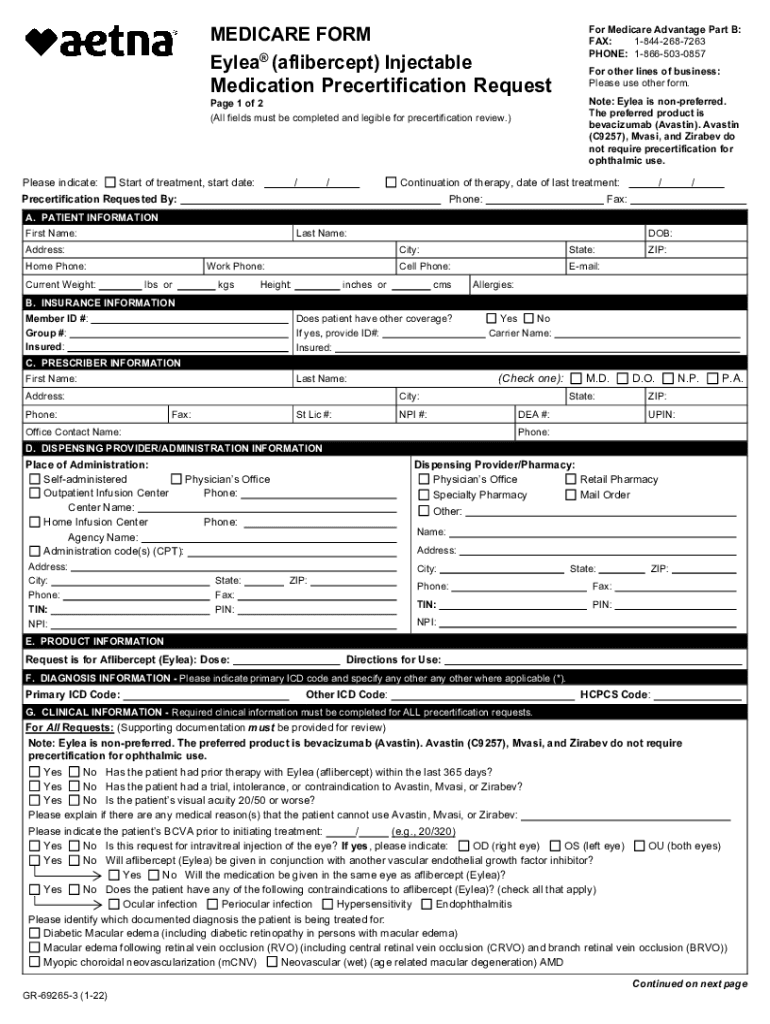
Aetna Eylea Prior Authorization Form - Specialty medication precertification request page 1 of 2 (all fields must be completed and legible for. Web aetna specialty precertification forms abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab (humira ®) precertification request form (pdf, 651 kb). And learn about our slide method to see if you’re eligible for a. Web health insurance plans | aetna Visit the eylea resource center to access information for you and your patients. Web the basics of prior authorization when you need it this guide includes lists of the services and medicines that need prior authorization. For medicare advantage part b: Upload, modify or create forms. Peer to peer consultations peer to peers are scheduled by calling 1. Eylea ® (aflibercept) injectable medication precertification request. Web the basics of prior authorization when you need it this guide includes lists of the services and medicines that need prior authorization. And learn about our slide method to see if you’re eligible for a. Missing, inaccurate, or incomplete information. Visit the eylea resource center to access information for you and your patients. Try it for free now! In some plans, you might. (all fields must be completed and legible for precertification review.) for. Web aetna specialty precertification forms abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab (humira ®) precertification request form (pdf, 651 kb). Web health insurance plans | aetna Web epo/dialysis medication precertification request form (pdf, 739 kb) etanercept (enbrel ®) precertification request form. It means that aetna better. Check out this section to learn what it is and why it’s important. And learn about our slide method to see if you’re eligible for a. Web eylea is a specific and highly potent blocker of these growth factors. In some plans, you might. Some care will require your doctor to get our approval first. Web the basics of prior authorization. Web this form is intended for selecthealth members only. Web epo/dialysis medication precertification request form (pdf, 739 kb) etanercept (enbrel ®) precertification request form (pdf, 414 kb) golimumab (simponi ®) precertification. Web aetna medicare eylea prior authorization form. Specialty medication precertification request page 1 of 2 (all fields must be completed and legible for. Web this form is intended for selecthealth members only. Missing, inaccurate, or incomplete information. Web what is prior authorization? In some plans, you might. The services that need prior authorization. Web epo/dialysis medication precertification request form (pdf, 739 kb) etanercept (enbrel ®) precertification request form (pdf, 414 kb) golimumab (simponi ®) precertification. Check out this section to learn what it is and why it’s important. Web specialty medication precertification request please indicate: Web what is prior authorization? Ad register and subscribe now to work on your infertility injectable med precert request. The services that need prior authorization. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. Select the appropriate aetna form to get started. Eylea ® (aflibercept) injectable medication precertification request. It means that aetna better. Web the basics of prior authorization. Eylea ® (aflibercept) injectable medication precertification request. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. This process is called prior authorization or preapproval. Web aetna specialty precertification forms abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab (humira ®) precertification request form (pdf, 651 kb). Web aetna has partnered with covermymeds to offer electronic prior authorization (epa) services. Web health insurance plans | aetna Missing, inaccurate, or incomplete information. Peer to peer consultations peer to peers are scheduled by calling 1. Select the appropriate aetna form to get started. Web specialty medication precertification request please indicate: Web find out about changes to our prescription drug list. Eylea® (aflibercept) injectable medication precertification request. Web epo/dialysis medication precertification request form (pdf, 739 kb) etanercept (enbrel ®) precertification request form (pdf, 414 kb) golimumab (simponi ®) precertification. Web aetna specialty precertification forms abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab (humira ®) precertification request form (pdf, 651 kb). Select the appropriate aetna form to get started. Web epo/dialysis medication precertification request form (pdf, 739 kb) etanercept (enbrel ®) precertification request form (pdf, 414 kb) golimumab (simponi ®) precertification. Visit the eylea resource center to access information for you and your patients. Check out this section to learn what it is and why it’s important. (all fields must be completed and legible for precertification review.) for. Eylea ® (aflibercept) injectable medication precertification request. Web find out about changes to our prescription drug list. Web specialty medication precertification request please indicate: This process is called prior authorization or preapproval. In some plans, you might. The services that need prior authorization. Web aetna has partnered with covermymeds to offer electronic prior authorization (epa) services. Missing, inaccurate, or incomplete information. Web the basics of prior authorization when you need it this guide includes lists of the services and medicines that need prior authorization. Lessons what to request and except to our coverage laws. Web what is prior authorization? Some care will require your doctor to get our approval first. It means that aetna better. And learn about our slide method to see if you’re eligible for a.KY Aetna Pharmacy Prior Authorization Request Form Fill and Sign
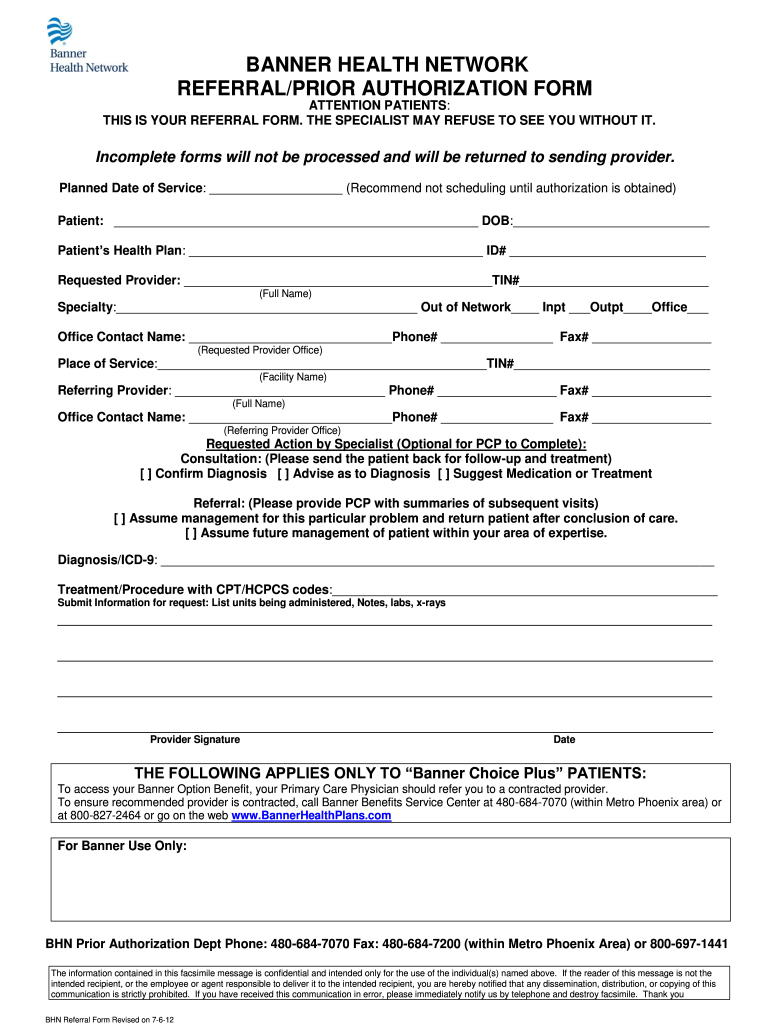
Banner Aetna Prior Authorization Form Fill Out and Sign Printable PDF
Aetna Medicare Prior Auth Form For Medication Form Resume Examples
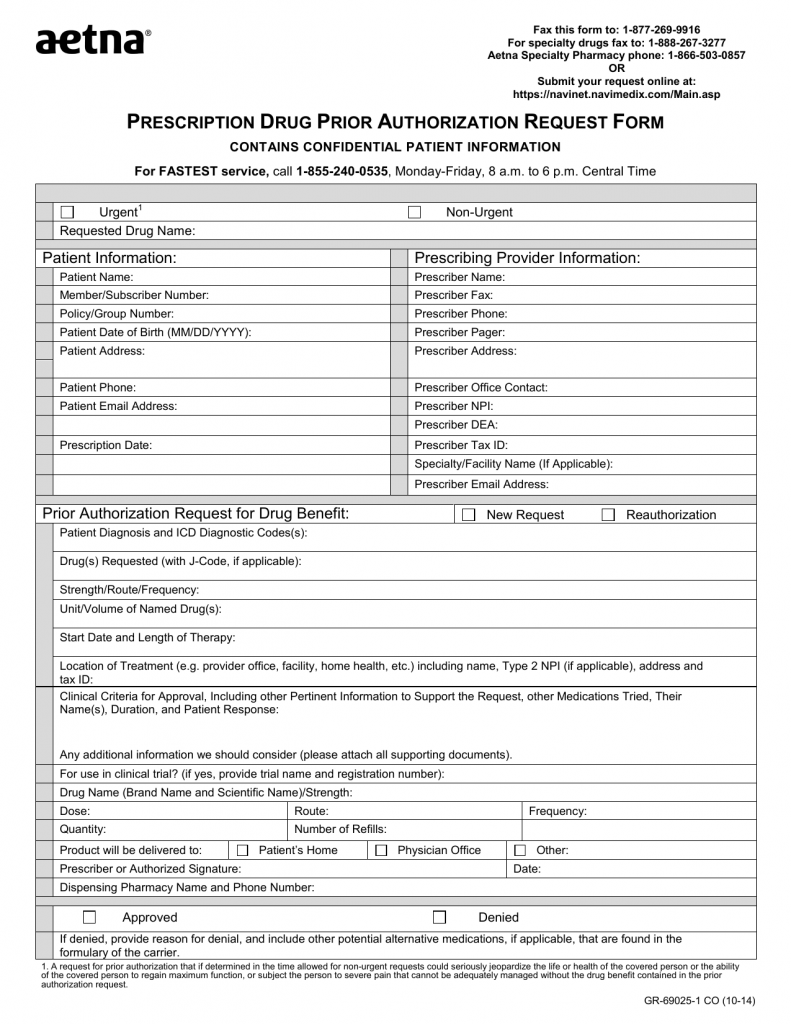
Download AETNA Prescription Drug Authorization Request Form PDF RTF
Free Aetna Prior (Rx) Authorization Form PDF eForms
Aetna blank prior authorization forms Fill out & sign online DocHub
Free AETNA Prior Prescription (Rx) Authorization Form PDF
Aetna Medicare Medication Prior Authorization Form Form Resume
Aetna eylea prior authorization form Fill out & sign online DocHub
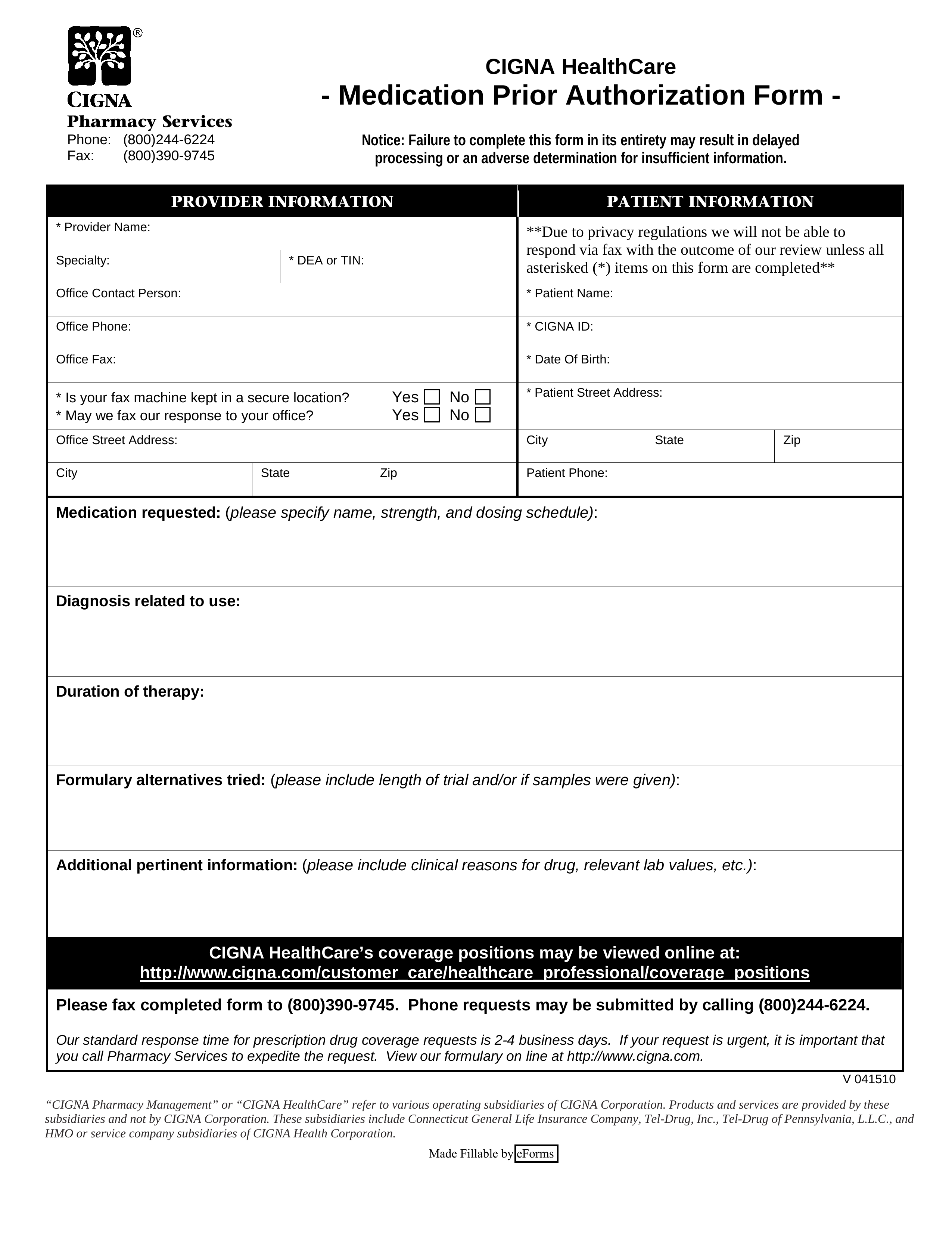
Free Cigna Prior (Rx) Authorization Form PDF eForms
Related Post: