Aetna Entyvio Prior Authorization Form
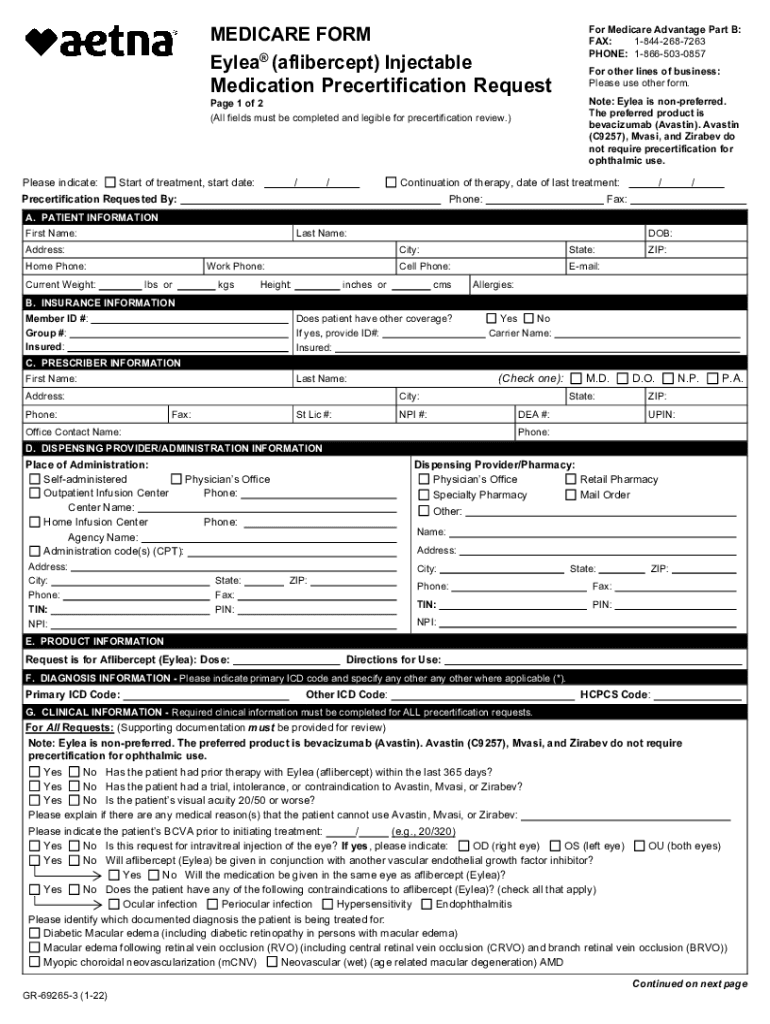
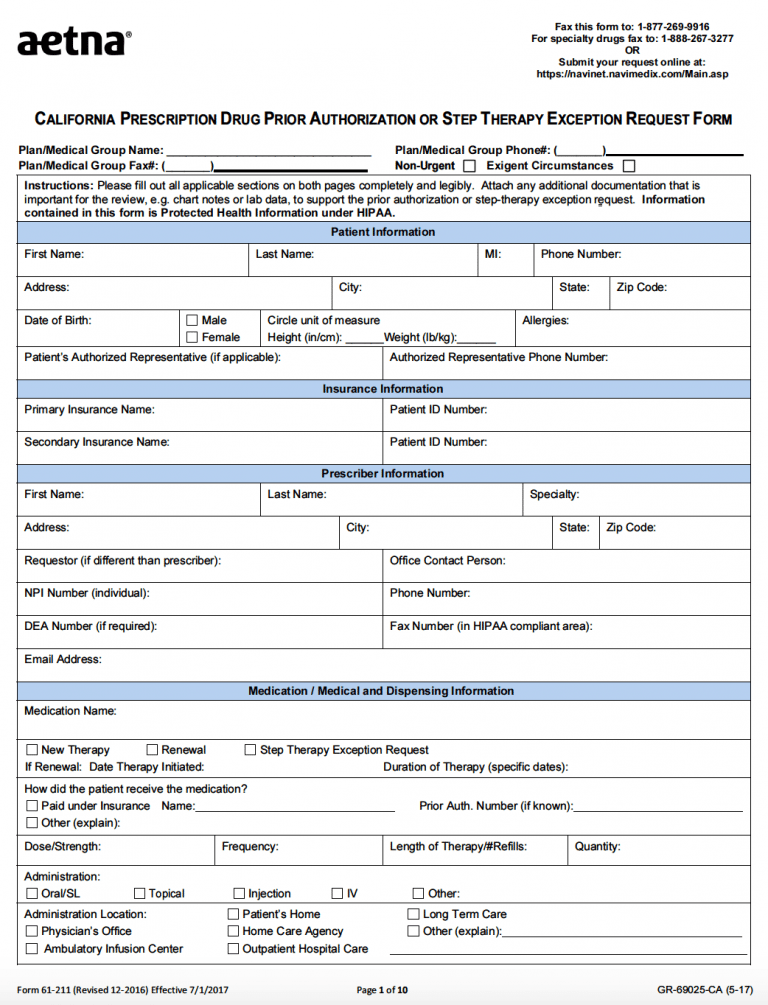
Aetna Entyvio Prior Authorization Form - It means that aetna better. Web initial authorization will be for no more than 14 weeks. To make an appropriate determination, providing the most. Start date / / continuation of therapy: Web to enroll in entyvioconnect, patients must provide information for sections 1 and 2 of the enrollment form and sign the patient hipaa authorization and patient support. Web aetna precertification notification phone: (belimumab) injectable medication precertification query. Web benefits verification—your doctor's office will work with your insurance company to determine if entyvio is covered. Web the basics of prior authorization when you need it this guide includes lists of the services and medicines that need prior authorization. Our standard response time for prescription drug coverage. To submit a request, call our precertification. Web aetna better health℠ premier plan requires prior authorization for select services. (all fields must be completed and legible for precertification review.) start. Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab (humira ®) precertification request form (pdf, 651. O for continuation of therapy , all of the following: Start date / / continuation of therapy: To submit a request, call our precertification. Web initial authorization will be for no more than 14 weeks. Web precertification of vedolizumab (entyvio) is required of all aetna participating providers and members in applicable plan designs. For precertification of vedolizumab, call (866) 752. Web aetna better health℠ premier plan requires prior authorization for select services. Our standard response time for prescription drug coverage. (all fields must be completed and legible for precertification review.) aetna precertification. Web to enroll in entyvioconnect, patients must provide information for sections 1 and 2 of the enrollment form and sign the patient hipaa authorization and patient support. Start. However, prior authorization is not required for emergency services. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home delivery, filing an appeal and more. O for continuation of therapy , all of the following: (vedolizumab) injectable medication precertification request. For precertification of vedolizumab, call (866) 752. Web forms library (belimumab) injectable medication precertification request. Web aetna specialty precertification forms. Web page 1 of 3. Web aetna pharmacy management administers, but does not offer, insure or otherwise underwrite the. To submit a request, call our precertification. Web forms library (belimumab) injectable medication precertification request. Ad uslegalforms.com has been visited by 100k+ users in the past month Documentation of positive clinical response to entyvio; Web aetna pharmacy management administers, but does not offer, insure or otherwise underwrite the. Web find the aetna medicare forms you need to help you get started with claims reimbursements, aetna rx home. Prior authorization—your doctor's office will submit. To submit a request, call our precertification. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. (all fields must be completed and legible for precertification review.) start of treatment: Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab (humira ®) precertification request form. Web aetna pharmacy management administers, but does not offer, insure or otherwise underwrite the. For precertification of vedolizumab, call (866) 752. (all fields must be completed and legible for precertification review.) start. Web patient hipaa authorization by signing the patient authorization section on the second page of this entyvioconnect enrollment form, i authorize my physician, health. Web to enroll in. To make an appropriate determination, providing the most. For precertification of vedolizumab, call (866) 752. Web forms library (belimumab) injectable medication precertification request. Web aetna specialty precertification forms. Start date / / continuation of therapy: (all fields must be completed and legible for precertification review.) start. Web aetna better health℠ premier plan requires prior authorization for select services. For precertification of vedolizumab, call (866) 752. Prior authorization—your doctor's office will submit. It means that aetna better. Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Start date / / continuation of therapy: Ad see if you are eligible for entyvio financial assistance. Documentation of positive clinical response to entyvio; Web forms library (belimumab) injectable medication precertification request. Web page 1 of 3. Web the basics of prior authorization when you need it this guide includes lists of the services and medicines that need prior authorization. (all fields must be completed and legible for precertification review.) start of treatment: (vedolizumab) injectable medication precertification request. Web aetna specialty precertification forms. Web precertification of vedolizumab (entyvio) is required of all aetna participating providers and members in applicable plan designs. Some care will require your doctor to get our approval first. For precertification of vedolizumab, call (866) 752. Check out this section to find out which prescription drugs need prior. Web aetna better health℠ premier plan requires prior authorization for select services. Web medicare form entyvio® (vedolizumab) injectable medication precertification request for medicare advantage part b: Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab (humira ®) precertification request form (pdf, 651. Web patient hipaa authorization by signing the patient authorization section on the second page of this entyvioconnect enrollment form, i authorize my physician, health. Web entyvio® (vedolizumab) injectable medication precertification request. Prior authorization—your doctor's office will submit.Aetna eylea prior authorization form Fill out & sign online DocHub
Aetna xolair prior authorization form Fill out & sign online DocHub
Prior Authorization Form Fill Out and Sign Printable PDF Template
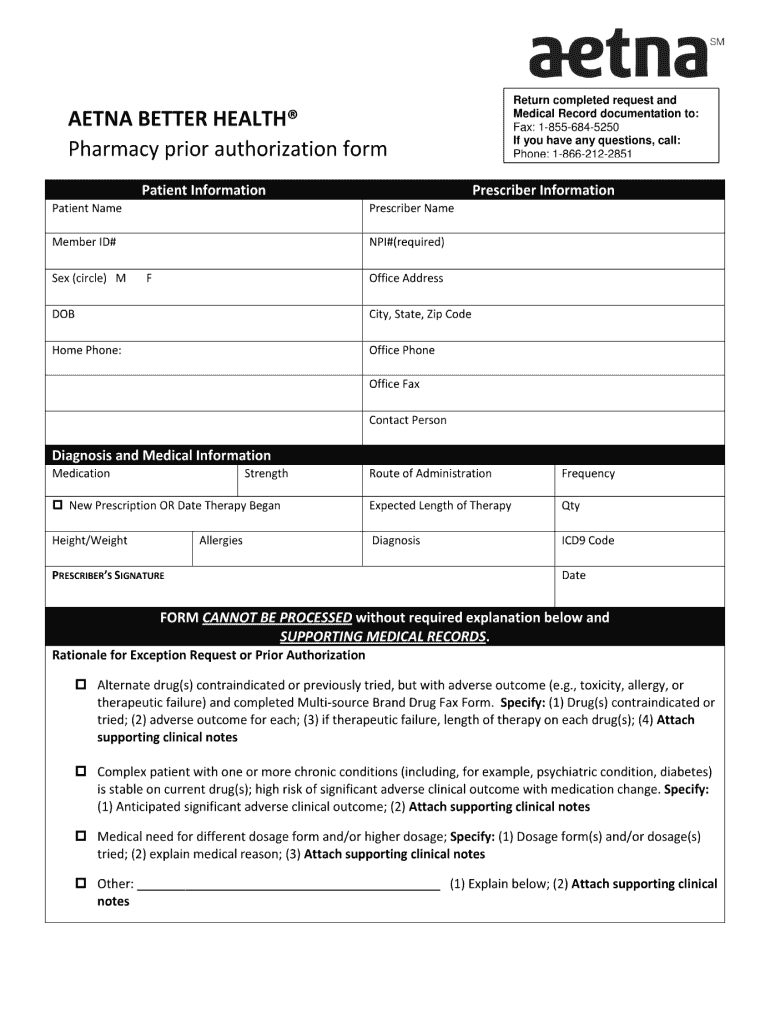
06/04/2013 Prior Authorization AETNA BETTER HEALTH OF PENNSYLVANIA Non
Aetna blank prior authorization forms Fill out & sign online DocHub
Free AETNA Prior Prescription (Rx) Authorization Form PDF
Aetna Prior Authorization Form PDF Medical Record Health Sciences
Covermymeds Humana Prior Auth Form / Aetna Prior Authorization Forms
Aetna Medicare Prior Auth Form For Medication Form Resume Examples
Aetna Prior Authorization Form printable pdf download
Related Post: